Anomalous left coronary artery from the pulmonary artery
| Anomalous left coronary artery from the pulmonary artery | |
|---|---|
| Other names: Bland-White-Garland syndrome | |
 | |
| Possible communication between left coronary artery and pulmonary artery in a 45-year-old woman with Bland-White-Garland syndrome. | |
Anomalous left coronary artery from the pulmonary artery (ALCAPA, Bland-White-Garland syndrome or White-Garland syndrome) is a rare congenital anomaly occurring in approximately 1 in 300,000 liveborn children. The diagnosis comprises between 0.24 and 0.46% of all cases of congenital heart disease.[1] The anomalous left coronary artery (LCA) usually arises from the pulmonary artery instead of the aortic sinus. In fetal life, the high pressure in the pulmonic artery and the fetal shunts enable oxygen-rich blood to flow in the LCA. By the time of birth, the pressure will decrease in the pulmonic artery and the child will have a postnatal circulation. The myocardium which is supplied by the LCA, will therefore be dependent on collateral blood flow from the other coronary arteries, mainly the RCA. Because the pressure in RCA exceeds the pressure in LCA a collateral circulation will increase. This situation ultimately can lead to blood flowing from the RCA into the LCA retrograde and into the pulmonary artery, thus forming a left-to-right shunt.[2]
Signs and symptoms
The development of symptoms in ALCAPA depends heavily on the amount of collaterals development. When only few collaterals are present, the myocardium will not get enough oxygen and will become ischemic. The symptoms in an infant with ALCAPA include signs of heart failure such as dyspnea and tachypnea, but sometimes the development is more subtle and the first sign of ischemia can be crying during feeding, sweating, failure to thrive and irritability. Approximately 90% of patients dies within the first year if left untreated.[1] The patients having a significant collateral circulation can live to adulthood in rare cases; their circulation is often not enough and they develop chronic ischemia, having a risk för sudden cardiac arrest, heart failure or maligant arrhythmia.[3][4] The mechanism of patient survival to adulthood is not fully understood.[4]
Cause
In terms of the etiology of ALCAPA we find in the development of the embryo that the heart muscle does not attach correctly.[5]
Diagnosis
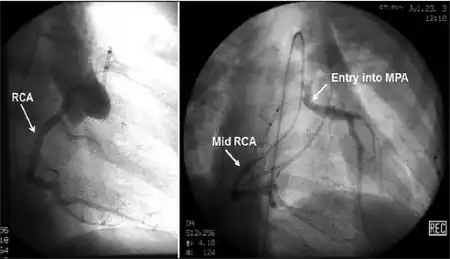
Historically ALCAPA was diagnosed with conventional angiography. Today echocardiography is easily used. It can provide direct visualisation of the anomalous coronary artery and other associated structural abnormalities, and it can also assess myocardial function .The use of pulse and color-flow doppler can sometimes visualise reversal flow in the pulmonic artery. Other non-invasive methods used are computed tomography (CT) as well as magnetic resonance imaging (MRI) which enable a direct visualisation of the arteries as well as the myocardial viability.[3]
Treatment
Surgery is indicated in all patients with ALCAPA independent of symptoms, since reconnection of the anomalous left coronary artery, to the aortic root, is crucial to the perfusion of the myocardium dependent on that vessel. Several surgical techniques have been described in ALCAPA repair, including reimplantation of the left coronary artery in to the aorta or creation of an intra-pulmonary buffer (Takeuchi procedure), bypass grafting. Establishment of a dual coronary system is the preferred method and if possible reimplantion of the artery is the approach of choice.[6] Surgery on the mitral valve at the same time as ALCAPA correction is controversial.[7] Even if surgery is carried in adulthood, reestablishment of a two-coronary system can make malignant arrhythmia disappear.
Prognosis
No difference in long-term mortality or left ventricle function has been shown between the different techniques to re-establish a two-coronary system. An exception is the ligation of the anomalous left coronary artery, which today is used in some cases and has a higher mortality. The development of surgical techniques and restoring of two-artery circulation has dramatically increased survival. Close long-term follow-up of these patients is necessary, to diagnose a recurrent left ventricle dysfunction, but also to understand better the natural evolution of a corrected heart.[7]
References
- 1 2 Kubota, Hiroshi; Endo, Hidehito; Ishii, Hikaru; Tsuchiya, Hiroshi; Inaba, Yusuke; Terakawa, Katsunari; Takahashi, Yu; Noma, Mio; Takemoto, Kazuya; Taniai, Seiichi; Sakata, Konomi (2020). "Adult ALCAPA: from histological picture to clinical features". Journal of Cardiothoracic Surgery. 15 (1): 14. doi:10.1186/s13019-020-1048-y. ISSN 1749-8090. PMC 6958604. PMID 31931842.
- ↑ Cardiology. Michael H. Crawford. Philadelphia. 2010. ISBN 978-0-7234-3644-7. OCLC 489073793.
{{cite book}}: CS1 maint: others (link) - 1 2 Peña, Elena; Nguyen, Elsie T.; Merchant, Naeem; Dennie, Carole (2009). "ALCAPA syndrome: not just a pediatric disease". Radiographics. 29 (2): 553–565. doi:10.1148/rg.292085059. ISSN 1527-1323. PMID 19325065. Archived from the original on 2022-08-06. Retrieved 2022-10-05.
- 1 2 Kwiatkowski, David M.; Mastropietro, Christopher W.; Cashen, Katherine; Chiwane, Saurabh; Flores, Saul; Iliopoulos, Ilias; Karki, Karan B.; Migally, Karl; Radman, Monique R.; Riley, Christine M.; Sassalos, Peter (2021). "Characteristics and Surgical Outcomes of Patients With Late Presentation of Anomalous Left Coronary Artery From the Pulmonary Artery: A Multicenter Study". Seminars in Thoracic and Cardiovascular Surgery. 33 (1): 141–150. doi:10.1053/j.semtcvs.2020.08.014. PMID 32858217. S2CID 221365678. Archived from the original on 2021-03-11. Retrieved 2022-10-05.
- ↑ "Anomalous left coronary artery from the pulmonary artery". Medline. Archived from the original on 21 October 2022. Retrieved 20 October 2022.
- ↑ Dodge-Khatami, Ali; Mavroudis, Constantine; Backer, Carl L (2002). "Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy". The Annals of Thoracic Surgery. 74 (3): 946–955. doi:10.1016/S0003-4975(02)03633-0. PMID 12238882. Archived from the original on 2022-06-21. Retrieved 2022-10-05.
- 1 2 Ismail, Muna; Jijeh, Abdulraouf; Alhuwaymil, Rathath M; Alahmari, Raneem; Alshahrani, Rawan; Almutairi, Reem; Habshan, Fahad; Shaath, Ghassan A (2020-12-01). "Long-Term Outcome of the Anomalous Origin of the Left Coronary Artery From the Pulmonary Artery (ALCAPA) in Children After Cardiac Surgery: A Single-Center Experience". Cureus. 12 (12): e11829. doi:10.7759/cureus.11829. ISSN 2168-8184. PMC 7781494. PMID 33409071. Archived from the original on 2022-10-21. Retrieved 2022-10-05.
External links
| External resources |
|---|