Thought disorder
| Thought disorder | |
|---|---|
| Other names | Formal thought disorder (FTD), thinking disorder |
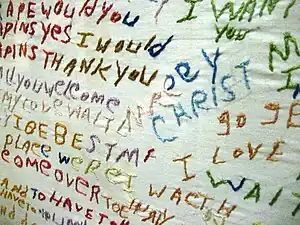 | |
| An embroidered cloth produced by a person with schizophrenia, showing the nonsensical associations between words and ideas characteristic of thought disorder | |
| Specialty | Psychiatry |
A thought disorder (TD) is any disturbance in cognition that adversely affects language and thought content, and thereby communication.[1][2] A variety of thought disorders were said to be characteristic of people with schizophrenia.[1][3] A content-thought disorder is typically characterized by the experience of multiple delusional fragments.[4] The term thought disorder is often used to refer to a formal thought disorder.[5]
A formal thought disorder (FTD) is a disruption of the form or structure of thought.[6] Formal thought disorder, also known as disorganized thinking, results in disorganized speech, and is recognized as a major feature of schizophrenia, and other psychoses.[7][8] FTD is also associated with conditions including mood disorders, dementia, mania, and neurological diseases.[9][7][3] Disorganized speech leads to an inference of disorganized thoughts.[10] From this behavior, we can infer an issue with the thought process of someone else.
Types of thought disorder include derailment,[11] pressured speech, poverty of speech, tangentiality, verbigeration and thought blocking.[3]
Formal thought disorder is a disorder of the form of thought rather than of content of thought that covers hallucinations and delusions.[12] FTD unlike hallucinations and delusions, is an observable objective sign of psychosis.[12] FTD is a common, and core symptom of a psychotic disorder and may be seen as a marker of its severity, and also as a predictor of prognosis.[3][13] It reflects a cluster of cognitive, linguistic, and affective disturbances, that has generated research interest from the fields of cognitive neuroscience, neurolinguistics, and psychiatry.[3]
Eugen Bleuler, who named schizophrenia, held that thought disorder was its defining characteristic.[14] However, disturbances of thinking and speech such as clanging or echolalia may be present in Tourette syndrome,[15] or other symptoms as found in delirium.[16] A clinical difference exists between these two groups. Those with psychoses are less likely to show an awareness or concern about the disordered thinking, while those with other disorders do show awareness and concerns about not being able to think straight.[17]
Content-thought disorder
Content-thought disorder is a thought disturbance in which a person experiences multiple, fragmented delusions, typically a feature of schizophrenia, and some other mental disorders including obsessive–compulsive disorder, and mania.[18][4] At the core of thought content disturbance are abnormal beliefs and convictions, after accounting for the person's culture and backgrounds, and range from overvalued ideas to fixed delusions.[19] Typically, abnormal beliefs and delusions are non-specific diagnostically,[20] even if some delusions are more prevalent in one disorder than another.[21]
Also neurotypical thought—consisting of awareness, concerns, beliefs, preoccupations, wishes, fantasies, imagination, and concepts—can be illogical, and can contain beliefs and prejudices/biases that are obviously contradictory.[22][23] Individuals also have considerable variations, and the same person's thinking also may shift considerably from time to time.[24]
Content-thought disorder is not limited to delusions. Other possible abnormalities include suicidal ideas, violent ideas, and homicidal ideas[25] as well as the following:[26][19]
- Preoccupation: centering thought to a particular idea in association with strong affection
- Obsession: a persistent thought, idea, or image that is intrusive or inappropriate, and is distressing or upsetting
- Compulsive behavior: the need to perform an act persistently and repetitively—without it necessarily leading to an actual reward or pleasure—to reduce distress
- Magical thinking: belief that one's thoughts by themselves can bring about effects in the world, or that thinking something corresponds with doing the same thing
- Overvalued ideas: false or exaggerated belief that is held with conviction but not with delusional intensity
- Phobias: irrational fears of objects or circumstances[27][28]
In psychosis, delusions are the most common thought-content abnormalities.[29] A delusion is a firm and fixed belief based on inadequate grounds not amenable to rational argument or evidence to the contrary, and not in sync with regional, cultural and educational background.[30] Delusions are common in people with mania, depression, schizoaffective disorder, delirium, dementia, substance use disorder, schizophrenia, and delusional disorders.[20] Common examples in mental status examination include the following:[27]
- Erotomania: belief that someone is in love with oneself
- Grandiose delusions: belief that one is the greatest, strongest, fastest, richest, and/or most intelligent person ever
- Persecutory delusion: belief that the person, or someone to whom the person is close, is being malevolently treated in some way
- Ideas of reference and delusions of reference: belief that insignificant remarks, coincident events, or innocuous objects in one's environment have personal meaning or significance
- Thought broadcasting: belief that others can hear or are aware of one's thoughts
- Thought insertion: belief that one's thoughts are not one's own, but rather belong to someone else and have been inserted into one's mind[30]
- Thought withdrawal: belief that thoughts have been 'taken out' of one's mind, and one has no power over this
- Influence: belief that other people or external agents are covertly exerting powers over oneself
- Outside control: belief that outside forces are controlling one's thoughts, feelings, and actions[31]
- Infidelity: belief that a partner is cheating on oneself
- Somatic: belief that one has a disease or medical condition
- Nihilistic: belief that the mind, body, the world at large, or parts thereof, no longer exist
Formal thought disorder
Overview
Formal thought disorder (FTD), or simply thought disorder, is also known as disorganized speech – evident from disorganized thinking, and is one of the hallmark features of schizophrenia.[6][8] Formal thought disorder is a disorder of the form of thought rather than of content of thought that covers hallucinations and delusions.[12] FTD, unlike hallucinations and delusions, is an observable objective sign of psychosis. FTD is a common, and core symptom of a psychotic disorder and may be seen as a marker of its severity, and also as a predictor of prognosis.[3][13] It reflects a cluster of cognitive, linguistic, and affective disturbances, that has generated research interest from the fields of cognitive neuroscience, neurolinguistics, and psychiatry.[3]
FTD is a complex, multidimensional syndrome characterized by deficiencies in the logical organizing of thought needed to achieve goals.[1] FTD can be subdivided into clusters of positive and negative symptoms, as well as objective versus subjective symptoms.[13] Within the scale of positive and negative symptoms they have been grouped into positive formal thought disorder (posFTD) and negative formal thought disorder (negFTD).[13][12] Positive subtypes were those of pressure of speech, tangentiality, derailment, incoherence, and illogicality.[13] Negative subtypes were those of poverty of speech and poverty of content.[12][13] The two groups were posited to be at either end of a spectrum of normal speech. However, later studies showed these to be poorly correlated.[12] A comprehensive measure of formal thought disorder is the Thought and Language Disorder (TALD) Scale.[32]
Nancy Andreasen preferred to call the thought disorders collectively as thought-language-communication disorders (TLC disorders).[33] Within the Thought, Language, Communication (TLC) Scale up to seven domains of FTD have been described with most of the variance accounted for by just two or three domains.[12] Some TLC disorders are more suggestive of a severe disorder and given priority by listing them in the first 11 items.[33]
Diagnoses
The DSM V categorises FTD as “a psychotic symptom, manifested as bizarre speech and communication.” FTD may include incoherence, peculiar words, disconnected ideas, or a lack of the unprompted content we would expect from normal speech.[34] Clinical psychologists typically assess FTD by initiating an exploratory conversation with patients and observing the patient’s verbal responses.[35] FTD is often used to establish a diagnosis of schizophrenia, as such, in cross-sectional studies 27–80% of patients with schizophrenia present with FTD. FTD, although a hallmark feature of schizophrenia, is also widespread amongst sufferers of other psychiatric disorders; up to 60% of those with schizoaffective disorder, and 53% of those with clinical depression show FTD, suggesting FTD is not pathognomonic of schizophrenia. Around 6% of healthy probands show a mild form of FTD. [36] The characteristics of FTD vary amongst disorders. Multiple studies show that FTD in mania is marked by irrelevant intrusions and pronounced combinatory thinking, usually with playfulness and flippancy lacking in Schizophrenic patients.[37][38][39]The FTD present in schizophrenic patients, however, was characterised by disorganisation, neologism, and fluid thinking; as well as confusion with word-finding difficulty.[40] There is limited data on the longitudinal course of FTD.[41] The most comprehensive longitudinal study of FTD done to date found a distinction in the longitudinal course of thought disorder symptoms between schizophrenia and other psychotic disorders. The study also found an association between pre-index assessments of social, work and educational functioning and the longitudinal course of FTD. [42]
Speculative Causes
Several theories have been developed to explain the causes of formal thought disorder. It has been proposed that formal thought disorder relates to neurocognition via semantic memory.[43] Semantic network impairment in people with schizophrenia—measured by the difference between fluency (number of animals' names produced in 60 seconds) and phonological fluency (number of words beginning with "F" produced in 60 seconds)—predicts severity of formal thought disorder, suggesting that verbal information (through semantic priming) is unavailable.[43] Other hypotheses include working memory deficit (being confused about what has already been said in a conversation) and attentional focus.[43] FTD in schizophrenia has been found to be associated with structural and functional abnormalities in the language network. Structural studies have found bilateral grey matter deficits in the language network, in particular, the bilateral inferior frontal gyrus, bilateral inferior parietal lobe and bilateral superior temporal gyrus to be FTD correlates. [44] However, there are studies that did not find an association between FTD and structural aberrations of the language network and regions not included in the language network have been associated with FTD. [45] Thus, future research is needed to clarify whether there is an association with FTD in schizophrenia and neural abnormalities in the language network. [46] There has also been investigation into the transmitter systems that might cause FTD. Studies have found that glutamate dysfunction due to a rarefication of glutamatergic synapses in the superior temporal gyrus in patients’ schizophrenia is a major cause for positive FTD. [47] The heritability of FTD has been demonstrated in myriad family and twin studies. Imaging genetics studies using a semantic verbal fluency task performed by the participants during functional MRI scanning revealed that alleles linked to glutamatergic transmission contribute to functional aberrations in typical language-related brain areas.[48] However, FTD is not solely genetically determined: environmental influences, such as allusive thinking in parents during childhood, and general environmental risk factors for schizophrenia (neurodevelopmental, childhood abuse, migration, social isolation, cannabis, etc) also contribute to the pathophysiology of FTD. [49] The origins of FTD have also been conceptualized from a social-learning perspective. Singer and Wynne contended that familial communication patterns play a key role in shaping the development of FTD— believing that dysfunctional social interactions undermine a child’s development of cohesive, stable mental representations of the world, therefore increasing their risk of developing FTD. [50]
Treatments
Antipsychotic medication is often utilised to treat FTD. The vast majority of studies examining the efficacy of antipsychotic treatment do not report the effects on syndromes or symptoms. Nevertheless, there are six older studies reporting on the effects of antipsychotic treatment on FTD. [51][52][53][54][55][56]From these studies and from clinical experience, we know that antipsychotics are often an effective treatment for patients with positive or negative FTD. There is, however, a subgroup of patients with treatment refractory FTD. Cognitive Behavioural Therapy is an another example of a treatment for FTD. There is currently very little research exploring the effectiveness of CBT for individuals with FTD. [57] Large randomised controlled trials evaluating the effectiveness of CBT for treating psychosis often exclude individuals with high levels of FTD due to FTD reducing therapeutic alliance which is associated with key outcomes in therapy.[58]However, there is some provisional evidence suggesting that FTD may not preclude the effectiveness of CBT.[59] Kircher and colleagues have suggested the following methods should be used in Cognitive-behavioural therapy for treating patients with formal thought disorder:[60]
• Practise structuring, summarising, and feedback methods
• Repeat and clarify the core issues and main emotions that the patient is trying to communicate
• Gently encourage patients to clarify what they are trying to communicate
• Ask patients to clearly state their communication goal
• Ask patients to slow down and explain how one-point leads to another
• Help patients identify the links between ideas
• Identify the main affect linked to the thought disorder
• Normalise problems with thinking
Signs and symptoms
In the general population, there will always be abnormalities in language and their presence is therefore not always diagnostic of any condition.[61] Language abnormalities can occur in schizophrenia and other disorders such as mania or depression, and can also occur in anybody who may simply be tired or stressed.[1][62] To distinguish thought disorder, patterns of speech, severity of symptoms, their frequency, and resulting functional impairment can be considered.[33]
Symptoms of thought disorder include derailment,[11] pressured speech, poverty of speech, tangentiality, and thought blocking.[3] FTD is a hallmark feature of schizophrenia, but is also associated with other conditions including mood disorders, dementia, mania, and neurological diseases.[6][9][62] Impaired attention, poor memory, and difficulty formulating abstract concepts may also reflect thought disorder, and can be observed or assessed with mental status tests such as serial sevens or memory tests.[29]
Types
There are many types of thought disorder.[63] They are also referred to as symptoms of formal thought disorder of which 30 are described including:[12]
Alogia (also poverty of speech)
- A poverty of speech, either in amount or content. Under negative/positive symptom classification of schizophrenia, it is classified as a negative symptom. When classifying symptoms into more dimensions, poverty of speech content—paucity of meaningful content with normal amount of speech—is a disorganization symptom, whereas poverty of speech—loss of speech production—is a negative symptom.[64] Under SANS, thought blocking is considered a part of alogia, and so is increased latency in response.[65]
Blocking or thought blocking (also deprivation of thought and obstructive thought).
- An abrupt stop in the middle of a train of thought which may or not be able to be continued.[66]
Circumstantial speech (also circumstantial thinking)[67]
- An inability to answer a question without giving excessive, unnecessary detail.[68] This differs from tangential thinking, in that the person does eventually return to the original point. For example, the patient answers the question "how have you been sleeping lately?" with "Oh, I go to bed early, so I can get plenty of rest. I like to listen to music or read before bed. Right now I'm reading a good mystery. Maybe I'll write a mystery someday. But it isn't helping, reading I mean. I have been getting only 2 or 3 hours of sleep at night."[69]
- A severe form of flight of ideas whereby ideas are related only by similar or rhyming sounds rather than actual meaning.[70][71] This may be heard as excessive rhyming and/or alliteration. e.g. "Many moldy mushrooms merge out of the mildewy mud on Mondays." "I heard the bell. Well, hell, then I fell." It is most commonly seen in bipolar disorder (manic phase), although it is often observed in patients with primary psychoses, namely schizophrenia and schizoaffective disorder.
Derailment (also loose association and knight's move thinking)[67]
- Thought frequently moves from one idea to another which is obliquely related or unrelated, often appearing in speech but also in writing,[72] e.g. "The next day when I'd be going out you know, I took control, like uh, I put bleach on my hair in California."[73]
Distractible speech
- During mid speech, the subject is changed in response to a nearby stimulus. e.g. "Then I left San Francisco and moved to... Where did you get that tie?"[74][75]
- Echoing of another's speech[70] that may only be committed once, or may be continuous in repetition. This may involve repeating only the last few words or last word of the examiner's sentences. This can happen immediately after a stimuli, or months to years later.[76] Echolalia is commonly seen with Autism and Tourette's Syndrome, although there are plenty of disorders that it can be attributed to.[77][78][79] e.g. "What would you like for dinner?", "What would you like for dinner?" "That's a good question." "That's a good question."
Evasion
- The next logical idea in a sequence is replaced with another idea closely but not accurately or appropriately related to it. Also called paralogia and perverted logic.[80][81] Example: "I... er ah... you are uh... I think you have... uh-- acceptable erm... uh... hair."
- A form of formal thought disorder marked by abrupt leaps from one topic to another, possibly with discernable links between successive ideas, perhaps governed by similarities between subjects or, in somewhat higher grades, by rhyming, puns, and word plays, or by innocuous environmental stimuli – e.g., the sound of birds chirping. It is most characteristic of the manic phase of bipolar illness.[70]
Illogicality[82]
- Conclusions are reached that do not follow logically (non-sequiturs or faulty inferences). e.g. "Do you think this will fit in the box?" draws a reply like "Well of course; it's brown, isn't it?"
Incoherence or word salad[67]
- Speech that is unintelligible because, though the individual words are real words, the manner in which they are strung together results in incoherent gibberish,[70] e.g. the question "Why do people comb their hair?" elicits a response like "Because it makes a twirl in life, my box is broken help me blue elephant. Isn't lettuce brave? I like electrons, hello please!"
Neologisms[67]
- forms completely new words or phrases whose origins and meanings are usually unrecognizable. Example is "I got so angry I picked up a dish and threw it at the geshinker."[83] These may also involve elisions of two words that are similar in meaning or in sound.[84] Although neologisms may sometimes refer to words that are formed incorrectly but whose origins are understandable (e.g. "headshoe" for hat), these can be more clearly referred to as word approximations.[85]
Overinclusion[76]
- The failure to eliminate ineffective, inappropriate, irrelevant, extraneous details associated with a particular stimulus.[28][86]
- Persistent repetition of words or ideas even when another person attempts to change the topic.[70] e.g. "It's great to be here in Nevada, Nevada, Nevada, Nevada, Nevada." This may also involve repeatedly giving the same answer to different questions. e.g. "Is your name Mary?" "Yes." "Are you in the hospital?" "Yes." "Are you a table?" "Yes." Perseveration can include palilalia and logoclonia, and can be an indication of organic brain disease such as Parkinson's.[76]
- Mispronunciation; syllables out of sequence. e.g. "I slipped on the lice and broke my arm."[87]
Pressured speech[88]
- Rapid speech without pauses, difficult to interrupt.
Referential thinking
- "Patients tendency to view innocuous stimuli as having a specific meaning for the self."[89] This could be seen as them repeatedly and inappropriately referring back to self. e.g. "What's the time?", "It's 7 o'clock. That's my problem."
- Substitution of inappropriate word. e.g. "I slipped on the coat, on the ice I mean, and broke my book."[90]
- Sentences may be stilted or vague. Speech characterized by the use of words or phrases that are flowery, excessive, and pompous,[70] e.g. "The attorney comported himself indecorously."
Tangential speech
Use of term
Some recent (2015, 2017) psychiatric/psychological glossaries defined thought disorder as disturbed thinking or cognition that affects communication, language, or thought content including poverty of ideas, neologisms, paralogia, word salad, and delusions[9][4] —which are disturbance of both thought content and thought form—and suggested the more specific terms of content thought disorder and formal thought disorder,[2] with content thought disorder defined as a thought disturbance characterized by multiple fragmented delusions,[18][4] and formal thought disorder defined as disturbance in the form or structure of thinking.[95][96] For example, DSM-5 (2013) only used the word formal thought disorder, mostly as a synonym of disorganized thinking and disorganized speech.[97] This is in contrast with ICD-10 (1992) which only used the word "thought disorder", always accompanied with "delusion" and "hallucination" separately,[98] and a general medical dictionary (2002) that although generally defined thought disorders similarly to the psychiatric glossaries,[99] but also used the word in other entries as ICD-10 did.[100]
The recent psychiatric text (2017) also mentioned when describing thought disorder as a "disorganization syndrome" within the context of schizophrenia:
"Thought disorder" here refers to disorganization of the form of thought and not content. An older use of the term "thought disorder" included the phenomena of delusions and sometimes hallucinations, but this is confusing and ignores the clear differences in the relationships between symptoms that have become apparent over the past 30 years. Delusions and hallucinations should be identified as psychotic symptoms, and thought disorder should be taken to mean formal thought disorders or a disorder of verbal cognition.
— Phenomenology of Schizophrenia (2017), THE SYMPTOMS OF SCHIZOPHRENIA[91]
The same text also mentioned that some clinicians use the term "formal thought disorder" broadly referring to abnormalities in thought form plus any psychotic cognitive sign or symptom,[101] and that various studies examining cognition and subsymdromes in schizophrenia may refer to formal thought disorder as "conceptual disorganization" or "disorganization factor."[91]
Still, there may be other dissenting opinions, including:
Unfortunately, "thought disorder" is often involved rather loosely to refer to both formal thought disorder and delusional content. For the sake of clarity, the unqualified use of the phrase "thought disorder" should be discarded from psychiatric communication. Even the designation "formal thought disorder" covers too wide a territory. It should always be made clear whether one is referring to derailment or loose associations, flight of ideas, or circumstantiality.
— The Mental Status Examination, The Medical Basis of Psychiatry (2016)[102]
Course, diagnosis, and prognosis
It was believed that thought disorder occurred only in schizophrenia, but later findings indicate it may occur in other psychiatric conditions including mania, and occurs even in people without mental illness.[103] Also, people with schizophrenia don't all exhibit thought disorder, so not having any thought disorder doesn't mean the person doesn't have schizophrenia, i.e. the condition is not very specific to the disease.[104]
When adopting specific definitions of thought disorder subtypes and classifying them as positive and negative symptoms, Nancy Andreasen found[104] that different subtypes of thought disorder occur at different frequencies among those with manic, depression, and schizophrenia. People with mania have pressured speech as the most prominent symptom, but also have relatively high rates of derailment, tangentiality, and incoherence which are as prominent as in those with schizophrenia. They are likelier to have pressured speech, distractibility, and circumstantiality.[104][105]
People with schizophrenia have more negative thought disorder including poverty of speech and poverty of content of speech, but also have relatively high rates of certain positive thought disorders.[104] Derailment, loss of goal, poverty of content of speech, tangentiality and illogicality are particularly characteristic of schizophrenia.[106] People with depression have relatively less thought disorders; the most prominent are poverty of speech, poverty of content of speech, and circumstantiality. She found the diagnostic usefulness of dividing the symptoms into subtypes, such as having negative thought disorders without the full affective symptoms highly suggest schizophrenia.[104][105]
She also found prognostic values of negative/positive symptom divisions. In manic patients, most thought disorders return to normal levels 6 months after evaluation which suggests that thought disorders in this condition, although as severe as in schizophrenia, tend to be recoverable.[104] In people with schizophrenia, however, negative thought disorders remain after six months, and sometimes worsen. Positive thought disorders get better somewhat. Also, negative thought disorder is a good predictor of some outcomes, e.g. patients with prominent negative thought disorders do worse on social functioning six months later.[104] So, in general, having more prominent negative symptoms suggest a worse outcome. Nevertheless, some people may do well, respond to medication, and have normal brain function. The positive symptoms are similar vice versa.[107]
At illness onset, prominent thought disorder also predicts worse prognosis, including:[91]
- illness begins earlier
- increased risk of hospitalization
- decreased functional outcomes
- increased disability rates
- increased inappropriate social behaviors
Thought disorder unresponsive to treatment also predicts worse illness course.[91] In schizophrenia, thought disorders' severity tend to be more stable than hallucinations and delusions. Prominent thought disorders are more unlikely to diminish in middle age compared to positive symptoms.[91] Less severe thought disorder may occur during the prodromal and residual periods of schizophrenia.[108] Treatment for thought disorder may include psychotherapy such as cognitive behavior therapy (CBT) and/or psychotropic medications.[109]
DSM-5 include delusions, hallucinations, disorganized thought process (formal thought disorder), and disorganized or abnormal motor behavior (including catatonia) as key symptoms in "psychosis."[8] Although not specific to different diagnoses, certain aspects of psychosis are characteristic of some diagnoses. Schizophrenia spectrum disorders (e.g., schizoaffective disorder, schizophreniform disorder) typically consist of prominent hallucinations and/or delusions as well as formal thought disorder—displayed as severe behavioral abnormalities including disorganized, bizarre, and catatonic behavior.[6][8] Psychotic disorders due to general medical conditions and substance-induced psychotic disorders typically consist of delusions and/or hallucinations.[8][110] Delusional disorder and shared psychotic disorder, which are more rare, typically consist of persistent delusions.[110] Research found that most formal thought disorders are commonly found in schizophrenia and mood disorders, but poverty of speech content is more common in schizophrenia.[111]
Experienced clinicians may distinguish true psychosis, such as in schizophrenia, and bipolar mania, from malingering, when an individual fakes illness for other gains, by clinical presentations. For example, malingerers feign thought contents with no irregularities in form such as derailment or looseness of associations.[112] Negative symptoms including alogia may not be present. In addition, chronic thought disorder is typically distressing.[112]
Typically, autism spectrum disorders (ASD), whose diagnosis requires onset of symptoms prior to 3 years of age, can be distinguished from early-onset schizophrenia by disease onset occurrence (schizophrenia manifestation under age 10 is extremely rare) and the fact that ASD patients don't display formal thought disorders.[113] However, it has been suggested that individuals with autism spectrum disorders (ASD) display language disturbances like those found in schizophrenia; a 2008 study found that children and adolescents with ASD showed significantly more illogical thinking and loose associations than control subjects.[114] The illogical thinking was related to cognitive functioning and executive control; the loose associations were related to communication symptoms and to parent reports of stress and anxiety.[114]
Rorschach inkblots have shown to be a very useful tool in assessing thought disorder in disturbed patients.[115][1] A series of inkblots are shown and the responses to them by the patients are recorded and further analyzed to determine disturbances of thought.[1] The nature of the assessment itself offers insight to the cognitive processes of another and how they respond to equivocal stimuli.[116] Hermann Rorschach first developed this test as a measure for diagnosing schizophrenia after realizing that people suffering from schizophrenia gave drastically different interpretations of Klecksographie inkblots as compared to others who's thought process was considered normal.[117] It has since been one of the most widely used assessment tools in diagnosing thought disorders.[1]
The Thought Disorder Index (TDI), also called the Delta Index, was developed to help further determine the severity of thought disorder in verbal responses.[1] TDI scores are mainly derived from verbally expressed interpretations of the Rorschach Inkblot Test, but TDI can also be used with other verbal samples including the Wechsler Adult Intelligence Scale.[1] TDI includes a twenty-three-category scoring index.[1] Each category scores the level of severity on a scale from 0-1, with .25 being mild and 1.00 being most severe (.25, .50, .75, 1.00).[1]
Criticisms
The concept of thought disorder has been criticized as being based on circular or incoherent definitions.[118] For example, symptoms of thought disorder are inferred from disordered speech, based on the assumption that disordered speech arises because of disordered thought. Incoherence, or word salad, refers to speech that is semantically unconnected and conveys no meaning to the listener.[70]
Furthermore, although thought disorder is typically associated with psychosis, similar phenomena can appear in different disorders, potentially leading to misdiagnosis—for example, in the case of incomplete yet potentially fruitful thought processes.[119]
Another criticism related to the separation of symptoms of schizophrenia into negative/positive symptoms, including thought disorder, is that it oversimplifies the complexity of thought disorder and its relationship with other positive symptoms.[120] Later factor analysis studies found that negative symptoms tend to correlate with one another, while positive symptoms tend to separate into two groups.[120] The three clusters became roughly known as negative symptoms, psychotic symptoms, and disorganization symptoms.[107] Alogia, a thought disorder traditionally classified as a negative symptom, can be separated into two separate groups: poverty of speech content as a disorganization symptom, and poverty of speech, response latency, and thought blocking as negative symptoms.[121] Nevertheless, the efforts that led to the positive/negative symptom diametrics may allow the more accurate characterization of schizophrenia in the later works.[122]
See also
- Aphasia
- Auditory processing disorder
- Emil Kraepelin's dream speech
- Speech and language pathology
References
- 1 2 3 4 5 6 7 8 9 10 11 Hart M, Lewine RR (May 2017). "Rethinking Thought Disorder". Schizophrenia Bulletin. 43 (3): 514–522. doi:10.1093/schbul/sbx003. PMC 5464106. PMID 28204762.
- 1 2 "Thought disorder". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 3 4 5 6 7 8 Roche E, Creed L, MacMahon D, Brennan D, Clarke M (July 2015). "The Epidemiology and Associated Phenomenology of Formal Thought Disorder: A Systematic Review". Schizophrenia Bulletin. 41 (4): 951–62. doi:10.1093/schbul/sbu129. PMC 4466171. PMID 25180313.
- 1 2 3 4 "Content-thought disorder". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- ↑ "Thought Disorder - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 15 July 2021.
- 1 2 3 4 "Formal thought disorder". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 "Disorganized speech". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 3 4 5 Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). American Psychiatric Association. 2013. p. 88. ISBN 9780890425541.
- 1 2 3 Kaplan and Sadock's Comprehensive Textbook of Psychiatry (2017), Appendix B: Glossary of Psychiatry and Psychology Terms. "thought disorder Any disturbance of thinking that affects language, communication, or thought content; the hallmark feature of schizophrenia. Manifestations range from simple blocking and mild circumstantiality to profound loosening of associations, incoherence, and delusions; characterized by a failure to follow semantic and syntactic rules that is inconsistent with the person's education, intelligence, or cultural background."
- ↑ Roche, E.; Creed, L.; MacMahon, D.; Brennan, D.; Clarke, M. (2015). "The Epidemiology and Associated Phenomenology of Formal Thought Disorder: A Systematic Review". Schizophrenia Bulletin. pp. 951–962. doi:10.1093/schbul/sbu129. PMC 4466171. PMID 25180313. Retrieved 6 June 2021.
- 1 2 "Derailment". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 3 4 5 6 7 8 Kircher T, Bröhl H, Meier F, Engelen J (June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet. Psychiatry. 5 (6): 515–526. doi:10.1016/S2215-0366(18)30059-2. PMID 29678679.
- 1 2 3 4 5 6 Bora E, Yalincetin B, Akdede BB, Alptekin K (July 2019). "Neurocognitive and linguistic correlates of positive and negative formal thought disorder: A meta-analysis". Schizophrenia Research. 209: 2–11. doi:10.1016/j.schres.2019.05.025. PMID 31153670. S2CID 167221363.
- ↑ Colman, A. M. (2001) Oxford Dictionary of Psychology, Oxford University Press. ISBN 0-19-860761-X
- ↑ Barrera A, McKenna PJ, Berrios GE (2009). "Formal thought disorder, neuropsychology and insight in schizophrenia". Psychopathology. 42 (4): 264–9. doi:10.1159/000224150. PMID 19521143. S2CID 26079338.
- ↑ Noble J, Greene HL (15 January 1996). Textbook of primary care medicine. Mosby. p. 1325. ISBN 978-0-8016-7841-7.
- ↑ Jefferson JW, Moore DS (2004). Handbook of medical psychiatry. Elsevier Mosby. p. 131. ISBN 0-323-02911-6.
- 1 2 Kaplan and Sadock's Comprehensive Textbook of Psychiatry (2017), "Appendix B: Glossary of Psychiatry and Psychology Terms" "content thought disorder Disturbance in thinking in which a person exhibits delusions that may be multiple, fragmented, and bizarre."
- 1 2 Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "Chapter 1 Psychiatric History and Mental Status Examination", MENTAL STATUS EXAMINATION, Thought Disorder, Thought Content., p. 7.
- 1 2 Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Thought Content, Disturbances in Thought Contents.
- ↑ Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Thought Content, Delusions.
- ↑ Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Thought Content.
- ↑ Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Types of Thinking.
- ↑ Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Normal Thinking.
- ↑ Psychiatric Interview, History, and Mental Status Examination of the Adult Patient (2017), HISTORY AND EXAMINATION, Risk Assessment "Suicidal, violent, and homicidal ideation fall under the category of thought content..."
- ↑ Houghtalen RP, Mcintyre JS (2017). "7.1 Psychiatric Interview, History, and Mental Status Examination of the Adult Patient". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. Table 7.1-5. Elements of the Mental Status Examination with Examples of Abnormal Findings. ISBN 978-1-4511-0047-1.
Thought content: obsession, delusion, magical thinking, overvalued ideas, ideas of reference or influence, persecutory ideas.
- 1 2 Sadock BJ (2017). "7.2 Outline for a Psychiatric Examination". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. MENTAL STATUS, Table 7.2–1. Common Questions for the Psychiatric History and Mental Status. ISBN 978-1-4511-0047-1.
Thought content: Delusions— persecutory (paranoid), grandiose, infidelity, somatic, sensory, thought broadcasting, thought insertion, ideas of reference, ideas of unreality, phobias, obsessions, compulsions, ambivalence, autism, dereism, blocking, suicidal or homicidal preoccupation, conflicts, nihilistic ideas, hypochondriasis, depersonalization, derealization, flight of ideas, idé fixe, magical thinking, neologisms.
- 1 2 Akiskal HS (2016). "1 The Mental Status Examination". In Fatemi SH, Clayton PJ (eds.). The Medical Basis of Psychiatry (4th ed.). New York: Springer Science+Business Media. 1.5.5. Speech and Thought., pp. 8–10. doi:10.1007/978-1-4939-2528-5. ISBN 978-1-4939-2528-5.
- "This form of thought is most characteristic of mania and tends to be overinclusive, with difficulty in excluding irrelevant, extraneous details from the association."
- 1 2 Thought Disorder (2016), 25.2. Definition., pp. 497–498. cited Fish FJ (1962). Schizophrenia. Bristol, England: Bright.
- 1 2 Psychiatric Interview, History, and Mental Status Examination of the Adult Patient (2017), HISTORY AND EXAMINATION, Thought Content & Table 7.1–7. Examples of Delusional Thought
- ↑ Fatemi SH, Folsom TD (2016). "6 Schizophrenia". In Fatemi SH, Clayton PJ (eds.). The Medical Basis of Psychiatry (4th ed.). New York: Springer Science+Business Media. 6.6. Clinical Findings, 6.6.2. Mental Status Examination in a Subject with Schizophrenia, 6.6.2.5. Thought Form and Content, p. 103. doi:10.1007/978-1-4939-2528-5. ISBN 978-1-4939-2528-5.
- ↑ Kircher T, Krug A, Stratmann M, Ghazi S, Schales C, Frauenheim M, et al. (December 2014). "A rating scale for the assessment of objective and subjective formal Thought and Language Disorder (TALD)". Schizophrenia Research. 160 (1–3): 216–21. doi:10.1016/j.schres.2014.10.024. PMID 25458572.
- 1 2 3 Andreasen NC (November 1979). "Thought, language, and communication disorders. I. Clinical assessment, definition of terms, and evaluation of their reliability". Archives of General Psychiatry. 36 (12): 1315–21. doi:10.1001/archpsyc.1979.01780120045006. PMID 496551.
- ↑ Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). Arlington, VA: American Psychiatric Association. 2013. ISBN 9780890425558.
- ↑ "Thought Disorder | Johns Hopkins Psychiatry Guide". www.hopkinsguides.com.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Holzman, Philip S.; Shenton, Martha E.; Solovay, Margie R. (1 January 1986). "Quality of Thought Disorder in Differential Diagnosis". Schizophrenia Bulletin. pp. 360–372. doi:10.1093/schbul/12.3.360.
- ↑ Nestor, Paul G.; Shenton, Martha E.; Wible, Cindy; Hokama, Hiroto; O'Donnell, Brian F.; Law, Susan; McCarley, Robert W. (9 February 1998). "A neuropsychological analysis of schizophrenic thought disorder". Schizophrenia Research. pp. 217–225. doi:10.1016/S0920-9964(97)00101-1.
- ↑ Solovay, Margie R.; Shenton, Martha E.; Holzman, Philip S. (1 January 1987). "Comparative Studies of Thought Disorders: I. Mania and Schizophrenia". Archives of General Psychiatry. pp. 13–20. doi:10.1001/archpsyc.1987.01800130015003.
- ↑ Solovay, Margie R.; Shenton, Martha E.; Holzman, Philip S. (1 January 1987). "Comparative Studies of Thought Disorders: I. Mania and Schizophrenia". Archives of General Psychiatry. pp. 13–20. doi:10.1001/archpsyc.1987.01800130015003.
- ↑ Yalincetin, Berna; Bora, Emre; Binbay, Tolga; Ulas, Halis; Akdede, Berna Binnur; Alptekin, Koksal (July 2017). "Formal thought disorder in schizophrenia and bipolar disorder: A systematic review and meta-analysis". Schizophrenia Research. pp. 2–8. doi:10.1016/j.schres.2016.12.015.
- ↑ Marengo, Joanne T.; Harrow, Martin (1 January 1997). "Longitudinal Courses of Thought Disorder in Schizophrenia and Schizoaffective Disorder". Schizophrenia Bulletin. pp. 273–285. doi:10.1093/schbul/23.2.273.
- 1 2 3 Harvey PD, Keefe RS, Eesley CE (2017). "12.10 Neurocognition in Schizophrenia". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. RELATIONSHIP OF NEUROCOGNITIVE IMPAIRMENT TO SCHIZOPHRENIA SYMPTOMS, Formal Thought Disorder. ISBN 978-1-4511-0047-1.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ de Sousa, Paulo; Spray, Amy; Sellwood, William; Bentall, Richard P. (15 December 2015). "'No man is an island'. Testing the specific role of social isolation in formal thought disorder". Psychiatry Research. pp. 304–313. doi:10.1016/j.psychres.2015.09.010.
- ↑ Singer, M. T.; Wynne, L. C. (February 1965). "THOUGHT DISORDER AND FAMILY RELATIONS OF SCHIZOPHRENICS. IV. RESULTS AND IMPLICATIONS". Archives of General Psychiatry. pp. 201–212. doi:10.1001/archpsyc.1965.01720320089010.
- ↑ Cuesta, M. J.; Peralta, V.; de Leon, J. (January 1994). "Schizophrenic syndromes associated with treatment response". Progress in Neuro-Psychopharmacology & Biological Psychiatry. pp. 87–99. doi:10.1016/0278-5846(94)90026-4.
- ↑ Wang, Xiaohong; Savage, Robert; Borisov, Andrey; Rosenberg, Jill; Woolwine, Bobbi; Tucker, Melanie; May, Roberta; Feldman, Jacqueline; Nemeroff, Charles B.; Miller, Andrew H. (October 2006). "Efficacy of risperidone versus olanzapine in patients with schizophrenia previously on chronic conventional antipsychotic therapy: a switch study". Journal of Psychiatric Research. pp. 669–676. doi:10.1016/j.jpsychires.2006.03.008.
- ↑ Remberk, Barbara; Namysłowska, Irena; Rybakowski, Filip (3 December 2012). "Cognition and communication dysfunctions in early-onset schizophrenia: effect of risperidone". Progress in Neuro-Psychopharmacology & Biological Psychiatry. pp. 348–354. doi:10.1016/j.pnpbp.2012.07.007.
- ↑ "APA PsycNet". psycnet.apa.org.
- ↑ Hurt, S. W.; Holzman, P. S.; Davis, J. M. (December 1983). "Thought disorder. The measurement of its changes". Archives of General Psychiatry. pp. 1281–1285. doi:10.1001/archpsyc.1983.01790110023005.
- ↑ Spohn, H. E.; Coyne, L.; Larson, J.; Mittleman, F.; Spray, J.; Hayes, K. (1986). "Episodic and residual thought pathology in chronic schizophrenics: effect of neuroleptics". Schizophrenia Bulletin. pp. 394–407. doi:10.1093/schbul/12.3.394.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Palmier-Claus, Jasper; Griffiths, Robert; Murphy, Elizabeth; Parker, Sophie; Longden, Eleanor; Bowe, Samantha; Steele, Ann; French, Paul; Morrison, Anthony; Tai, Sara (2 October 2017). "Cognitive behavioural therapy for thought disorder in psychosis". Psychosis. pp. 347–357. doi:10.1080/17522439.2017.1363276.
- ↑ Palmier-Claus, Jasper; Griffiths, Robert; Murphy, Elizabeth; Parker, Sophie; Longden, Eleanor; Bowe, Samantha; Steele, Ann; French, Paul; Morrison, Anthony; Tai, Sara (2 October 2017). "Cognitive behavioural therapy for thought disorder in psychosis". Psychosis. pp. 347–357. doi:10.1080/17522439.2017.1363276.
- ↑ Kircher, Tilo; Bröhl, Henrike; Meier, Felicitas; Engelen, Jennifer (1 June 2018). "Formal thought disorders: from phenomenology to neurobiology". The Lancet Psychiatry. pp. 515–526. doi:10.1016/S2215-0366(18)30059-2.
- ↑ Çokal, Derya; Sevilla, Gabriel; Jones, William Stephen; Zimmerer, Vitor; Deamer, Felicity; Douglas, Maggie; Spencer, Helen; Turkington, Douglas; Ferrier, Nicol; Varley, Rosemary; Watson, Stuart (19 September 2018). "The language profile of formal thought disorder". NPJ Schizophrenia. 4 (1): 18. doi:10.1038/s41537-018-0061-9. ISSN 2334-265X. PMC 6145886. PMID 30232371.
- 1 2 Thought Disorder (2016), 25.3. What Are the Boundaries of Thought Disorder?., pp. 498–499.
- ↑ Thought Disorder (2016), 25.4. What Are the Common Types of Thought Disorder?, pp. 498–499.
- ↑ Phenomenology of Schizophrenia (2017), THE SYMPTOMS OF SCHIZOPHRENIA, Categories of Negative Symptoms.
- "... In this way, alogia is conceived of as a 'negative thought disorder.' ..."
- "... The paucity of meaningful content in the presence of a normal amount of speech that is sometimes included in alogia is actually a disorganization of thought and not a negative symptom and is properly included in the disorganization cluster of symptoms. ..."
- ↑ Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "6 Psychiatric Rating Scales", Table 6–5 Scale for the Assessment of Negative Symptoms (SANS), p. 44.
- ↑ "Blocking". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 3 4 5 Houghtalen, Rory P; McIntyre, John S (2017). "7.1 Psychiatric Interview, History, and Mental Status Examination of the Adult Patient". In Sadock, Virginia A; Sadock, Benjamin J; Ruiz, Pedro (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. HISTORY AND EXAMINATION, Thought Process/Form, Table 7.1–6. Examples of Disordered Thought Process/Form. ISBN 978-1-4511-0047-1. indicates and briefly defines the follow types: Clanging, Circumstantial, Derailment (loose associations), Flight of ideas, Incoherence (word salad), Neologism, Tangential, Thought blocking
- ↑ Videbeck S (2017). "8. Assessment". Psychiatric-Mental Health Nursing (7th ed.). Wolters Kluwer. CONTENT OF THE ASSESSMENT, Thought Process and Content, p. 232. ISBN 9781496355911.
- ↑ Videbeck (2017), Chapter 16 Schizophrenia, APPLICATION OF THE NURSING PROCESS, Thought Process and Content, p. 446.
- 1 2 3 4 5 6 7 8 Videbeck, S (2008). Psychiatric-Mental Health Nursing, 4th ed. Philadelphia: Wolters Kluwers Health, Lippincott Williams & Wilkins.
- ↑ "Thought disorder" (PDF). Retrieved 26 February 2020.
- ↑ APA dictionary of psychology (2015), p. 299 "derailment n. a symptom of thought disorder, often occurring in individuals with schizophrenia, marked by frequent interruptions in thought and jumping from one idea to another unrelated or indirectly related idea. It is usually manifested in speech (speech derailment) but can also be observed in writing. Derailment is essentially equivalent to loosening of associations. See cognitive derailment; thought derailment."
- ↑ Thought Disorder (2016), 25.4.2.8. Distractible Speech, p. 502.
- ↑ Thought Disorder (2016), 25.4.2.8. Distractible Speech, p. 502.
- ↑ "Distractible speech". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 3 March 2020.
- 1 2 3 4 5 Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "10 Schizophrenia", CLINICAL FEATURES, Thought, pp. 168–169.
- "Form of Thought. Disorders of the form of thought are objectively observable in patients' spoken and written language. The disorders include looseness of associations, derailment, incoherence, tangentiality, circumstantiality, neologisms, echolalia, verbigeration, word salad, and mutism."
- "Thought Process. ... Disorders of thought process include flight of ideas, thought blocking, impaired attention, poverty of thought content, poor abstraction abilities, perseveration, idiosyncratic associations (e.g., identical predicates and clang associations), overinclusion, and circumstantiality."
- ↑ Ganos, Christos; Ogrzal, Timo; Schnitzler, Alfons; Münchau, Alexander (1 September 2012). "The pathophysiology of echopraxia/echolalia: Relevance to Gilles De La Tourette syndrome". Movement Disorders. 27 (10): 1222–1229. doi:10.1002/mds.25103. PMID 22807284. S2CID 22422642.
- ↑ Fred R. Volkmar; et al. (2005). Handbook of autism and pervasive developmental disorders. Vol. 1: Diagnosis, development, neurobiology, and behavior (3rd ed.). Hoboken, NJ: John Wiley. ISBN 978-0-470-93934-5. OCLC 60394857.
- ↑ Duffy, Joseph R. (2013). Motor speech disorders: substrates, differential diagnosis, and management (Third ed.). St. Louis, MI. ISBN 978-0-323-07200-7. OCLC 819941855.
- ↑ "Evasion". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- ↑ Kaplan & Sadock's Comprehensive Textbook of Psychiatry (2017), Appendix B Glossary of Psychiatry and Psychology Terms. "evasion ... consists of suppressing an idea that is next in a thought series and replacing it with another idea closely related to it. Also called paralogia; perverted logic."
- ↑ Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "Chapter 6 Psychiatric Rating Scales", OTHER SCALES, Table 6–6 Scale for the Assessment of Positive Symptoms (SAPS), Positive formal thought disorder, p. 45 includes and defines Derailment, Tangentiality, Incoherence, Illogicality, Circumstantiality, Pressure of speech, Distractible speech, Clanging.
- ↑ Thought Disorder (2016), 25.4.2.6. Neologisms, p. 502.
- ↑ Rohrer JD, Rossor MN, Warren JD (February 2009). "Neologistic jargon aphasia and agraphia in primary progressive aphasia". Journal of the Neurological Sciences. 277 (1–2): 155–9. doi:10.1016/j.jns.2008.10.014. PMC 2633035. PMID 19033077.
- ↑ Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "Chapter 4 Signs and Symptoms in Psychiatry", GLOSSARY OF SIGNS AND SYMPTOMS, p. 29
- ↑ APA dictionary of psychology (2015), p. 751 overinclusion n. failure of an individual to eliminate ineffective or inappropriate responses associated with a particular stimulus.
- ↑ Kurowski, Kathleen; Blumstein, Sheila E. (February 2016). "Phonetic Basis of Phonemic Paraphasias in Aphasia: Evidence for Cascading Activation". Cortex; A Journal Devoted to the Study of the Nervous System and Behavior. 75: 193–203. doi:10.1016/j.cortex.2015.12.005. ISSN 0010-9452. PMC 4754157. PMID 26808838.
- ↑ "Pressured speech". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- ↑ Cicero, David C.; Kerns, John G. (1 April 2011). "Unpleasant and Pleasant Referential Thinking: Relations with Self- Processing, Paranoia, and Other Schizotypal Traits". Journal of Research in Personality. 45 (2): 208–218. doi:10.1016/j.jrp.2011.02.002. ISSN 0092-6566. PMC 4447705. PMID 26028792.
- ↑ Buckingham, H. W.; Rekart, D. M. (May 1979). "Semantic paraphasia". Journal of Communication Disorders. 12 (3): 197–209. doi:10.1016/0021-9924(79)90041-8. ISSN 0021-9924. PMID 438359.
- 1 2 3 4 5 6 Lewis SF, Escalona R, Keith SJ (2017). "12.2 Phenomenology of Schizophrenia". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. THE SYMPTOMS OF SCHIZOPHRENIA, Disorganization, Thought Disorder. ISBN 978-1-4511-0047-1.
- As quoted in the templated quote.
- "Thought disorder is the most studied form of the disorganization symptoms. It is referred to as "formal thought disorder," or "conceptual disorganization," or as the "disorganization factor" in various studies that examine cognition or subsyndromes in schizophrenia. ..."
- ↑ "Tangential speech". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 23 February 2020.
- 1 2 Clinical Manifestations of Psychiatric Disorders (2017), THINKING DISTURBANCES, Continuity. "Word salad describes the stringing together of words that seem to have no logical association, and verbigeration describes the disappearance of understandable speech, replaced by strings of incoherent utterances."
- ↑ Kaplan and Sadock's Concise Textbook of Clinical Psychiatry (2008), "Chapter 4 Signs and Symptoms in Psychiatry", GLOSSARY OF SIGNS AND SYMPTOMS, p. 32
- ↑ Kaplan and Sadock's Comprehensive Textbook of Psychiatry (2017), "Appendix B: Glossary of Psychiatry and Psychology Terms" "formal thought disorder Disturbance in the form of thought rather than the content of thought; thinking characterized by loosened associations, neologisms, and illogical constructs; thought process is disordered, and the person is defined as psychotic. Characteristic of schizophrenia."
- ↑ APA dictionary of psychology (2015), p. 432 "formal thought disorder disruptions in the form or structure of thinking. Examples include derailment and tangentiality. It is distinct from thought disorder, in which the disturbance relates to thought content."
- ↑ American Psychiatry Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington: American Psychiatric Publishing. ISBN 978-0-89042-555-8.
- As the proper formal thought disorder: "Schizophrenia Spectrum and Other Psychotic Disorders", Key Features That Define the Psychotic Disorders, Disorganized Thinking (Speech), p. 88 "Disorganized thinking (formal thought disorder) is typically inferred from the individual's speech. ..."
- As possibly something else: "Dissociative Disorders", Differential Diagnosis, Psychotic disorders, p. 296 "... Dissociative experiences of identity fragmentation or possession, and of perceived loss of control over thoughts, feelings, impulses, and acts, may be confused with signs of formal thought disorder, such as thought insertion or withdrawal. ..."
- ↑ "The ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines (CDDG)" (PDF). World Health Organization. 1992. Archived (PDF) from the original on 17 October 2004.
- F06.2 Organic delusional [schizophrenia-like] disorder, p.59: Features suggestive of schizophrenia, such as bizarre delusions, hallucinations, or thought disorder, may also be present. ... Diagnostic guidelines ... Hallucinations, thought disorder, or isolated catatonic phenomena may be present. ...
- F20.0 Paranoid schizophrenia, p. 80: ... Thought disorder may be obvious in acute states, but if so it does not prevent the typical delusions or hallucinations from being described clearly. ...
- F20.1 Hebephrenic schizophrenia, p. 81: ... In addition, disturbances of affect and volition, and thought disorder are usually prominent. Hallucinations and delusions may be present but are not usually prominent. ...
- ↑ The British Medical Association Illustrated Medical Dictionary. Dorling Kindersley. 2002. p. 547. ISBN 0-7513-3383-2.
thought disorders Abnormalities in the structure or content of thought, as reflected in a person's speech, writing, or behaviour. ...
- ↑ The BMA Illustrated Medical Dictionary (2002)
- p. 470 psychosis: ... Symptoms include delusions, hallucinations, thought disorders, loss of affect, mania, and depression. ...
- p. 499-500 schizophrenia: ... The main symptoms are various forms of delusions such as those of persecution (which are typical of paranoid schizophrenia); hallucinations, which are usually auditory (hearing voices), but which may also be visual or tactile; and thought disorder, leading to impaired concentration and thought processes. ...
- ↑ Matorin AA, Shah AA, Ruiz P (2017). "8 Clinical Manifestations of Psychiatric Disorders". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. THINKING DISTURBANCES, Flow and Form Disturbances. ISBN 978-1-4511-0047-1.
Although formal thought disorder typically refers to marked abnormalities in the form and flow or connectivity of thought, some clinicians use the term broadly to include any psychotic cognitive sign or symptom.
- ↑ The Mental Status Examination (2016), 1.6.2. Disturbances in Thinking., pp. 14–15.
- ↑ Wensing, T.; Cieslik, E. C.; Müller, V. I.; Hoffstaedter, F.; Eickhoff, S. B.; Nickl-Jockschat, T. (2017). "Neural correlates of formal thought disorder: An activation likelihood estimation meta-analysis". Human Brain Mapping. 38 (10): 4946–4965. doi:10.1002/hbm.23706. PMC 5685170. PMID 28653797.
- 1 2 3 4 5 6 7 Thought Disorder (2016), 25.5. Diagnostic and Prognostic Significance of Thought Disorder, pp. 502–503. cited
- Andreasen NC (November 1979). "Thought, language, and communication disorders. I. Clinical assessment, definition of terms, and evaluation of their reliability". Archives of General Psychiatry. 36 (12): 1315–21. doi:10.1001/archpsyc.1979.01780120045006. PMID 496551.
- Andreasen NC (November 1979). "Thought, language, and communication disorders. II. Diagnostic significance". Archives of General Psychiatry. 36 (12): 1325–30. doi:10.1001/archpsyc.1979.01780120055007. PMID 496552.
- Andreasen NC, Hoffrnann RE, Grove WM (1984). Alpert M (ed.). Mapping abnormalities in language and cognition. Controversies in schizophrenia, 1985. New York: Guilford Press. pp. 199–226.
- 1 2 Coryell W, Clayton PJ (2016). "4 Bipolar Illness". In Fatemi SH, Clayton PJ (eds.). The Medical Basis of Psychiatry (4th ed.). New York: Springer Science+Business Media. 4.7. Clinical Picture, 4.7.2. Symptoms, p. 59. doi:10.1007/978-1-4939-2528-5. ISBN 978-1-4939-2528-5.
- ↑ Oyebode F (2015). "10 Disorder of Speech and Language". Sims' Symptoms in the Mind: Textbook of Descriptive Psychopathology (5th ed.). Saunders Elsevier. Schizophrenic Language Disorder, CLINICAL DESCRIPTION AND THOUGHT DISORDER, p. 167. ISBN 978-0-7020-5556-0.
- 1 2 Thought Disorder (2016), 25.6. Relationship Between Thought Disorders and Other Symptoms of Schizophrenia., pp. 503–504.
- ↑ DSM-5 (2013), Schizophrenia Spectrum and Other Psychotic Disorders, Key Features That Define the Psychotic Disorders, Disorganized Thinking (Speech), p. 88.
- ↑ "Thought Disorder | Johns Hopkins Psychiatry Guide". www.hopkinsguides.com. Retrieved 15 July 2021.
- 1 2 Ivleva EI, Tamminga CA (2017). "12.16 Psychosis as a Defining Dimension in Schizophrenia". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. DSM-5: AN UPDATED DEFINITION OF PSYCHOSIS. ISBN 978-1-4511-0047-1.
- ↑ Akiskal HS (2017). "13.4 Mood Disorders: Clinical Features". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. BIPOLAR DISORDERS, Bipolar I Disorder, Acute Mania. ISBN 978-1-4511-0047-1.
- 1 2 Ninivaggi FJ (2017). "28.1 Malingering". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. CLINICAL PRESENTATIONS OF MALINGERING, Psychological Symptomatology: Clinical Presentations, Psychosis. ISBN 978-1-4511-0047-1.
- ↑ Sikich L, Chandrasekhar T (2017). "53 Early-Onset Psychotic Disorders". In Sadock VA, Sadock BJ, Ruiz P (eds.). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. DIFFERENTIAL DIAGNOSIS, Autism Spectrum Disorders. ISBN 978-1-4511-0047-1.
- 1 2 Solomon M, Ozonoff S, Carter C, Caplan R (September 2008). "Formal thought disorder and the autism spectrum: relationship with symptoms, executive control, and anxiety". Journal of Autism and Developmental Disorders. 38 (8): 1474–84. doi:10.1007/s10803-007-0526-6. PMC 5519298. PMID 18297385.
- ↑ Hart, Mara; Lewine, Richard R. J. (May 2017). "Rethinking Thought Disorder". Schizophrenia Bulletin. 43 (3): 514–522. doi:10.1093/schbul/sbx003. ISSN 0586-7614. PMC 5464106. PMID 28204762.
- ↑ "Rapaport, D. Diagnostic psychological testing. Chicago: Year Book Publishers, 1945, 1946, pp. 1089, two volumes. $13.00 (both vols.)". Journal of Clinical Psychology. 2 (3): 301–302. 1946. doi:10.1002/1097-4679(194607)2:3<301::AID-JCLP2270020320>3.0.CO;2-X. ISSN 1097-4679.
- ↑ "What's behind the Rorschach inkblot test?". BBC News. 24 July 2012. Retrieved 15 July 2021.
- ↑ Bentall, R. (2003) Madness explained: Psychosis and Human Nature. London: Penguin Books Ltd. ISBN 0-7139-9249-2
- ↑ Tufan, Ali Evren; Bilici, Rabia; Usta, Genco; Erdoğan, Ayten (22 June 2012). "Mood disorder with mixed, psychotic features due to vitamin b12 deficiency in an adolescent: case report". Child and Adolescent Psychiatry and Mental Health. 6 (1): 25. doi:10.1186/1753-2000-6-25. ISSN 1753-2000. PMC 3404901. PMID 22726236.
- 1 2 Thought Disorder (2016), 25.6. Relationship Between Thought Disorders and Other Symptoms of Schizophrenia., pp. 503–504. cited
- Arndt S, Alliger RJ, Andreasen NC (March 1991). "The distinction of positive and negative symptoms. The failure of a two-dimensional model". The British Journal of Psychiatry. 158: 317–22. doi:10.1192/bjp.158.3.317. PMID 2036528.
- Bilder RM, Mukherjee S, Rieder RO, Pandurangi AK (1985). "Symptomatic and neuropsychological components of defect states". Schizophrenia Bulletin. 11 (3): 409–19. doi:10.1093/schbul/11.3.409. PMID 4035304.
- Liddle PF (August 1987). "The symptoms of chronic schizophrenia. A re-examination of the positive-negative dichotomy". The British Journal of Psychiatry. 151: 145–51. doi:10.1192/bjp.151.2.145. PMID 3690102.
- ↑ Miller DD, Arndt S, Andreasen NC (2004). "Alogia, attentional impairment, and inappropriate affect: their status in the dimensions of schizophrenia". Comprehensive Psychiatry. 34 (4): 221–6. doi:10.1016/0010-440X(93)90002-L. PMID 8348799.
- ↑ Phenomenology of Schizophrenia (2017), THE SYMPTOMS OF SCHIZOPHRENIA, Negative Symptoms. "The two-syndrome concept as formulated by T. J. Crow was especially important in spurring research into the nature of negative symptoms. ...—but this does not diminish the creative efforts that led to these scales or importance of these scales for research. In fact, it was only through careful analysis of the structure of symptoms in these scales that a more accurate characterization of the phenomenology of schizophrenia was possible."
Further reading
- VandenBos GR, ed. (2015). APA dictionary of psychology (2nd ed.). Washington, DC: American Psychological Association. doi:10.1037/14646-000. ISBN 978-1-4338-1944-5.
- Sadock VA, Sadock BJ, Ruiz P, eds. (2017). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. ISBN 978-1-4511-0047-1.
- Sadock BJ, Sadock VA (2008). Kaplan and Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. ISBN 9780781787468.
- Andreasen NC (2016). "25 Thought Disorder". In Fatemi SH, Clayton PJ (eds.). The Medical Basis of Psychiatry (4th ed.). New York: Springer Science+Business Media. pp. 497–505. doi:10.1007/978-1-4939-2528-5. ISBN 978-1-4939-2528-5.
- McKenna PJ, Oh TM (2005). Schizophrenic Speech: Making Sense of Bathroots and Ponds that Fall in Doorways. Cambridge University Press. ISBN 978-0-521-81075-3.