ALK positive lung cancer
| ALK positive lung cancer | |
|---|---|
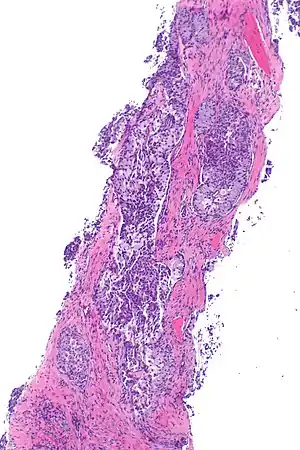 | |
| Micrograph showing ALK positive lung adenocarcinoma. H&E stain. | |
| Specialty | Oncology |
ALK positive lung cancer is a primary malignant lung tumor whose cells contain a characteristic abnormal configuration of DNA wherein, most frequently, the echinoderm microtubule-associated protein-like 4 (EML4) gene is fused to the anaplastic lymphoma kinase (ALK) gene. Less frequently, there will be novel translocation partners for the ALK gene, in place of EML4.[1] This abnormal gene fusion leads to the production of a protein that appears, in many cases, to promote and maintain the malignant behavior of the cancer cells.[2]
The transforming EML4-ALK fusion gene was first reported in non-small cell lung carcinoma (NSCLC) in 2007.[3]
Signs and symptoms
The signs and symptoms of this cancer include
- A cough that doesn't go away
- Chest pain that gets worse with deep breathing, coughing, or laughing
- Hoarseness
- Weight loss without trying or loss of appetite
- Coughing up blood
- Shortness of breath
- A weak or tired feeling
- Wheezing[4]
Diagnosis
Classification
Most lung carcinomas containing the ALK gene fusion are adenocarcinomas.
Some studies suggest that the papillary adenocarcinoma and the signet ring cell adenocarcinoma[5] variants are more likely to carry this fused gene than other histological variants.
The median age at diagnosis is around 50 years and the majority are female. [4][6]
Screening

Screening for ALK positive lung cancer is now a standard of care in the United States and Canada. Screening can be done with immunostaining, FISH, or next-generation sequencing (NGS).
Treatment
Crizotinib is a targeted therapy (FDA approved in 2011), manufactured by Pfizer and marketed under the brand name Xalkori and Crizalk that targets the EML4/ALK fusion gene.
Ceritinib is a second generation targeted therapy (FDA approved in 2014), manufactured by Novartis and sold under the brand name Zykadia that also targets the EML4 fusion gene, but as a second generation drug it has a smaller molecule that allows superior penetration of the Blood Brain Barrier (BBB) over Crizotinib and is more capable of protecting the Central Nervous System (CNS).
Alectinib another second generation targeted therapy and was approved (for this) by Japan in 2014[7] and by US FDA in 2015.,[8] manufactured by Genentech and marketed under the brand name Alecensa.
Brigatinib a second generation targeted therapy (FDA approved in 2017), manufactured by Takeda and is marketed under the brand name Alunbrig.
Ensartinib is a second generation targeted therapy (trial drug X-396), manufactured by XCovery.[9]
Lorlatinib is a third generation targeted therapy (FDA approved in 2018), manufactured by Pfizer.[10]
NVL-655 is a fourth generation targeted therapy (currently in clinical trials), developed by Nuvalent.[10][11]
Although treatment with immune checkpoint inhibitors has proved effective with some types of non-small cell lung cancer, it seems to be generally ineffective with ALK positive non-small cell lung cancer.[12]
Prognosis
Treatment with crizotinib achieves 60% response rate.[13] However, crizotinib showed no improvement on overall survival compared to chemotherapy.[14] This may be due to the fact that there was a 70% crossover rate to crizotinib in patients treated initially with chemotherapy.[15] Also, patients who tested negative for EML4/ALK fusion had a response rate to crizotinib of up to 35%.[16]
According to patient advocacy group ALK Positive, a study in December 2018 found that the median survival for people with stage 4 (IV) ALK-positive lung cancer was 6.8 years with the right care.[4]
Epidemiology
EML4-ALK gene fusions occur almost exclusively in carcinomas arising in non-smokers.[17][18] About 4% of non-small-cell lung carcinomas involve an EML4-ALK tyrosine kinase fusion gene.[19] 4–6% of lung adenocarcinomas involve the fusion gene.[13]
EML4-ALK mutation rarely occurs in combination with K-RAS or EGFR mutations.
References
- ↑ Iyevleva, Aglaya G.; Raskin, Grigory A.; Tiurin, Vladislav I.; Sokolenko, Anna P.; Mitiushkina, Natalia V.; Aleksakhina, Svetlana N.; Gariullina, Aigul R.; Strelkova, Tatiana N.; Merkulov, Valery O.; Ivantsov, Alexandr O.; Kuligina, Ekatherina Sh.; Pozharisski, Kazimir M.; Togo, Alexandr V.; Imyanitov, Evgeny N. (28 June 2015). "Novel ALK fusion partners in lung cancer". Cancer Letters. 362 (1): 116–121. doi:10.1016/j.canlet.2015.03.028. PMID 25813404 – via Science Direct.
- ↑ Soda M, Choi YL, Enomoto M, et al. (August 2007). "Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer". Nature. 448 (7153): 561–6. Bibcode:2007Natur.448..561S. doi:10.1038/nature05945. PMID 17625570. S2CID 2172543.
- ↑ Sasaki T, Rodig SJ, Chirieac LR, Jänne PA (July 2010). "The biology and treatment of EML4-ALK non-small cell lung cancer". Eur. J. Cancer. 46 (10): 1773–80. doi:10.1016/j.ejca.2010.04.002. PMC 2888755. PMID 20418096.
- 1 2 3 ALK Positive (5 February 2023). "What is ALK-Positive lung cancer?". ALK Positive. Archived from the original on 7 October 2020. Retrieved 5 February 2023.
- ↑ Koh Y, Kim DW, Kim TM, et al. (May 2011). "Clinicopathologic characteristics and outcomes of patients with anaplastic lymphoma kinase-positive advanced pulmonary adenocarcinoma: suggestion for an effective screening strategy for these tumors". J Thorac Oncol. 6 (5): 905–12. doi:10.1097/JTO.0b013e3182111461. PMID 21358343. S2CID 38377715.
- ↑ ALK Positive UK (5 February 2023). "Facts". ALK Positive UK. Archived from the original on 17 January 2023. Retrieved 5 February 2023.
- ↑ "Japan becomes first country to approve Roche's alectinib for people with a specific form of advanced lung cancer". Archived from the original on 2018-02-15. Retrieved 2016-02-11.
- ↑ New Oral Therapy To Treat ALK-Positive Lung Cancer. Dec 2015
- ↑ Xcovery (5 February 2023). "Ensartinib". Xcovery. Archived from the original on 3 December 2022. Retrieved 5 February 2023.
- 1 2 Ou, Sai-Hong Ignatius; Nagasaka, Misako; Brazel, Danielle; Hou, Yujie; Zhu, Viola W. (November 2021). "Will the clinical development of 4th-generation "double mutant active" ALK TKIs (TPX-0131 and NVL-655) change the future treatment paradigm of ALK+ NSCLC?". Translational Oncology. 14 (11): 1–9. doi:10.1016/j.tranon.2021.101191. PMC 8353359. PMID 34365220.
- ↑ Nuvalent Pipeline (5 February 2023). "Nuvalent Pipeline". Nuvalent. Archived from the original on 8 December 2022. Retrieved 5 February 2023.
- ↑ Jahanzeb, Mohammad; Lin, Huamao M; Pan, Xiaoyun; Yin, Yu; Baumann, Pia; Langer, Corey J (17 September 2020). "Immunotherapy Treatment Patterns and Outcomes Among ALK-Positive Patients With Non-Small-Cell Lung Cancer". Clinical Lung Cancer. 22 (1): 49–57. doi:10.1016/j.cllc.2020.08.003. PMID 33250347. S2CID 224908622.
- 1 2 Bayliss, R; Choi, J (March 2016). "Molecular mechanisms that underpin EML4-ALK driven cancers and their response to targeted drugs". Cellular and Molecular Life Sciences. 73 (6): 1209–1224. doi:10.1007/s00018-015-2117-6. PMC 4761370. PMID 26755435.
- ↑ Highlights of prescribing information FDA
- ↑ Solomon, Benjamin J.; Mok, Tony; Kim, Dong-Wan; Wu, Yi-Long; Nakagawa, Kazuhiko; Mekhail, Tarek; Felip, Enriqueta; Cappuzzo, Federico; Paolini, Jolanda; Usari, Tiziana; Iyer, Shrividya; Reisman, Arlene; Wilner, Keith D.; Tursi, Jennifer; Blackhall, Fiona; PROFILE 1014 Investigators (2014). "First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer". New England Journal of Medicine. 371 (23): 2167–2177. doi:10.1056/NEJMoa1408440. hdl:2434/426878. PMID 25470694.
- ↑ Summary of safety and effectiveness data FDA
- ↑ Shaw AT, Yeap BY, Mino-Kenudson M, et al. (September 2009). "Clinical Features and Outcome of Patients With Non–Small-Cell Lung Cancer Who Harbor EML4-ALK". Journal of Clinical Oncology. 27 (26): 4247–4253. doi:10.1200/JCO.2009.22.6993. PMC 2744268. PMID 19667264.
- ↑ Martelli MP, Sozzi G, Hernandez L, et al. (February 2009). "EML4-ALK rearrangement in non-small cell lung cancer and non-tumor lung tissues". Am. J. Pathol. 174 (2): 661–70. doi:10.2353/ajpath.2009.080755. PMC 2630573. PMID 19147828.
- ↑ Kumar, V; Abbas AK; Aster JC (2013). "Chapter 5". Robbins Basic Pathology (9th ed.). Elsevier Saunders. p. 212. ISBN 978-1-4377-1781-5.