Interventional neuroradiology
Endovascular Surgical Neuroradiology (ESN), also known as Neurointerventional Surgery (NIS), Interventional Neuroradiology (INR), and Endovascular Neurosurgery, is a medical subspecialty of Radiology, Neurosurgery, and Neurology specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and spine.[1]
History
Diagnostic angiography
Cerebral angiography was developed by Portuguese neurologist Egas Moniz at the University of Lisbon, in order to identify central nervous system diseases such as tumors or arteriovenous malformations. He performed the first brain angiography in Lisbon in 1927[3] by injecting an iodinated contrast medium into the internal carotid artery and using the X-rays discovered 30 years earlier by Roentgen in order to visualize the cerebral vessels. In pre-CT and pre-MRI, it was the only tool to observe the structures within the skull and was also used to diagnose extravascular pathologies.
Subsequently, European radiologists further developed the angiographic technique by replacing the traumatic direct puncture with catheterization: in 1953, Swedish physician Sven Seldinger introduced the technique of arterial and venous catheterization still in practice,[4] dubbed the Seldinger Technique. In 1964, the Norwegian radiologist Per Amudsen was the first to perform a complete brain angiography with a transfemoral approach, as it is performed today; he then moved to San Francisco to teach the technique to American neuroradiologists.[5] These two stages, at the basis of modern invasive vascular diagnostics, prepared the way for later therapeutic developments.
The first treatments: balloon occlusion
The first to carry out a true endovascular procedure was Charles Dotter, the father of angioplasty and considered by many as the father of all interventional radiology, as well as the first doctor to have performed endovascular treatment. On January 16, 1964, he performed a therapeutic angioplasty of a superficial femoral artery in an 82-year-old woman with an ischemic leg refusing amputation.[6] The artery remained open for the next 2 and a half years, after which the woman died of pneumonia.
The concept of using balloons to treat cerebrovascular lesions was inspired by a 1959 May Day celebration in Moscow’s Red Square. While watching children use tether lines to manipulate helium balloons, Fedor Serbinenko, a Russian neurosurgeon, began to envision small balloons moving through tortuous arteries.[7] In the 1970s Fedor Serbinenko developed a technique for closing intracranial aneurysms with balloons that were released into the internal carotid artery by occluding the lumen. The first treatment was performed in 1970 in Moscow, with the occlusion of an internal carotid to treat a carotid-cavernous fistula. He can be considered, therefore, the first interventional neuroradiologist. This technique was subsequently refined by neuroradiologists all over the world and mainly in France, where interventional neuroradiology developed and flourished.
Parallel to the development of catheters, in the radiology and neuroradiology units, image technology dramatically improved: Charles Mistretta in 1979 invented digital subtraction angiography (DSA), the technique currently in use. It consists of performing skull radiography under basic conditions which are then "subtracted" to the image after contrast media injection, to provide an image where only brain vessels are displayed, with great improvement in the diagnostic potential.
Coils replace balloon occlusion
Between the end of the '80s and the beginning of the '90s, INR was suddenly revolutionized after the work of two Italian physicians: Cesare Gianturco and Guido Guglielmi. The first combined a deep knowledge of diagnostic radiology with a great ability to solve technical and manual problems. He invented Gianturco's coils, which he used to make the first attempts to embolize arteries and aneurysms.[8] Gianturco also patented the first endovascular stent approved by the American FDA;[8] a device with a great legacy. In the second half of the 1980s, Sadek Hilal was the first in Columbia University to use coils to treat brain aneurysms; but this technique was inaccurate and dangerous because the coils were released with little control with great risk of occluding the vessel from which the aneurysm originated (parent vessel).[9] The coil embolization was revolutionized by the work of Guido Guglielmi in UCLA, who realized that electricity could function as a controlled release mechanism for coils; in 1991 he published two works dealing with the embolization of brain aneurysms by means of detachable platinum coils[10] (Guglielmi's coils). The treatment of aneurysms was thus made more accessible and safe.
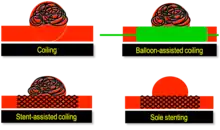
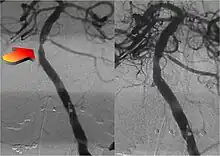
New techniques: Sole stenting and flow diversion stents
From the early 2000s, intracranial stents were used to prevent the coils inside the aneurysmal sac from protruding into the parent artery.[11][12] Flow diversion devices were later developed, with the function of reconstructing the vessel's normal anatomy without directly closing the aneurysm neck and therefore preserving side branches and preventing ischemia.[13] The sole stenting [14] procedure involves the insertion of a stent only (without any coils) into the vessel that has an aneurysm.[15]
Not just hemorrhages: the treatment of ischemic stroke
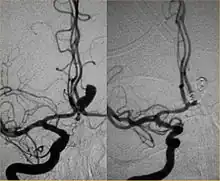
Between January and June 2015, five major randomized trials were published in the New England Journal of Medicine (NEJM) with the collaboration of interventional neuroradiologists and stroke neurologists (in the Netherlands,[16] Canada,[17] Australia,[18] USA[19] and Spain[20]) regarding the role of mechanical thrombectomy in the treatment of ischemic stroke, demonstrating that if it is performed in centers with proven experience, intra-arterial mechanical thrombectomy is more effective than traditional treatment (intravenous thrombolytic injection). The promising results of these mechanical thrombectomy trials were highlighted by the NEJM in an editorial, which concluded with the statement: "Endovascular equipoise no longer exists. It's about time."[21]
Thrombectomy is currently recommended by the guidelines written by the main American (AHA/ASA) [22] and European (ESO-ESNR-ESMINT) [23] societies of stroke neurologists and interventional neuroradiologists.
Diseases and conditions
The following is a list of diseases and conditions typically treated by neurointerventionalists.
- Cerebral aneurysm
- Brain arteriovenous malformation (AVM)
- Carotid-cavernous fistula (CCF)
- Dural arteriovenous fistula
- Extracranial (brachiocephalic) atherosclerosis
- Extracranial (head and neck) and paraspinal vascular malformations
- Head and neck tumors
- Intracranial atherosclerosis
- Juvenile nasopharyngeal tumor
- Meningiomas
- Nosebleeds
- Paragangliomas
- Stroke
- Spinal vascular malformations
- Traumatic vascular lesions
- Vasospasm
- Vertebral body tumors
- Vertebral body compression fractures
See also
References
- ↑ Chen, M.; Nguyen, T. (2008). "Emerging Subspecialties in Neurology: Endovascular surgical neuroradiology". Neurology. 70 (6): e21–e24. doi:10.1212/01.wnl.0000299086.22147.89. PMID 18250282. S2CID 26791160.
- ↑ Zenteno, M (March 2012). "Endovascular approach in the management of intracranial aneurysms. Part 1: basic concepts and devices". Gac Med Mex. 148 (2): 169–79. PMID 22622317.
- ↑ Artico, M (2017). "Egas Moniz: 90 Years (1927-2017) from Cerebral Angiography". Front Neuroanat. 11: 81. doi:10.3389/fnana.2017.00081. PMC 5610728. PMID 28974927.
- ↑ Seldinger, Sven Ivar (1953-05-01). "Catheter Replacement of the Needle in Percutaneous Arteriography: A new technique". Acta Radiologica. 39 (5): 368–376. doi:10.3109/00016925309136722. ISSN 0001-6926. PMID 13057644.
- ↑ Rosenbaum, Arthur E.; Eldevik, O. Petter; Mani, John R.; Pollock, Arliss J.; Mani, Richard L.; Gabrielsen, Trygve O. (2001-03-01). "In Re: Amundsen P. Cerebral angiography via the femoral artery with particular reference to cerebrovascular disease. Acta Neurol Scand 1967; Suppl. 31:115". American Journal of Neuroradiology. 22 (3): 584–589. ISSN 0195-6108. PMC 7976838. PMID 11237988.
- ↑ Busch, U (Mar 2014). "50 years ago: Charles Dotter and the first percutaneous transluminal angioplasty". Rofo (in German). 186 (3): 294–5. doi:10.1055/s-0034-1368886. PMID 24557558.
- ↑ Alaraj, A (Feb 2014). "Balloons in endovascular neurosurgery: history and current applications". Neurosurgery. 74 (Suppl 1): S163-90. doi:10.1227/NEU.0000000000000220. PMID 24402485.
- 1 2 LaGumina, Salvatore J.; Cavaioli, Frank J.; Primeggia, Salvatore; Varacalli, Joseph A. (2003). The Italian American Experience: An Encyclopedia. Routledge. p. 451. ISBN 9781135583330.
- ↑ Group, British Medical Journal Publishing (1963-03-16). "Obliteration of Intracranial Aneurysms by Pilojection". Br Med J. 1 (5332): 700. doi:10.1136/bmj.1.5332.700-a. ISSN 0007-1447. S2CID 30623125.
- ↑ Currie, S; Mankad, K; Goddard, A (Jan 2011). "Endovascular treatment of intracranial aneurysms: review of current practice". Postgraduate Medical Journal. 87 (1023): 41–50. doi:10.1136/pgmj.2010.105387. PMID 20937736. S2CID 30220296.
- ↑ Fessler, Richard D. (January 2000). "Intracranial Stent Placement to Trap an Extruded Coil During Endovascular Aneurysm Treatment: Technical Note". Neurosurgery. 46 (1): 248–253. doi:10.1093/neurosurgery/46.1.248. PMID 10626961.
- ↑ Biondi, Alessandra (September 2007). "Neuroform Stent-Assisted Coil Embolization of Wide-Neck Intracranial Aneurysms". Neurosurgery. 61 (3): 460–469. doi:10.1227/01.NEU.0000290890.62201.A9. PMID 17881956. S2CID 24343785.
- ↑ Krishna, Chandan (Oct–Dec 2014). "The Expanding Realm of Endovascular Neurosurgery: Flow Diversion for Cerebral Aneurysm Management". Methodist Debakey Cardiovascular Journal. 10 (4): 214–219. doi:10.14797/mdcj-10-4-214. PMC 4300059. PMID 25624975.
- ↑ Zenteno, M (Feb 2010). "Ten-year follow-up of giant basilar aneurysm treated by sole stenting technique: a case report". J Med Case Rep. 4: 64. doi:10.1186/1752-1947-4-64. PMC 2843709. PMID 20175900.
- ↑ Zenteno, MA (Jul 2005). "Sole stenting bypass for the treatment of vertebral artery aneurysms: technical case report". Neurosurgery. 57 (1 Suppl): E208. doi:10.1227/01.neu.0000163683.64511.24. PMID 15987592. S2CID 41571535.
- ↑ Berkhemer, Olvert A.; Fransen, Puck S.S.; Beumer, Debbie; van den Berg, Lucie A.; Lingsma, Hester F.; Yoo, Albert J.; Schonewille, Wouter J.; Vos, Jan Albert; Nederkoorn, Paul J.; Wermer, Marieke J.H.; van Walderveen, Marianne A.A. (2015-01-01). "A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke". New England Journal of Medicine. 372 (1): 11–20. doi:10.1056/NEJMoa1411587. hdl:2066/153000. ISSN 0028-4793. PMID 25517348.
- ↑ Goyal, Mayank; Demchuk, Andrew M.; Menon, Bijoy K.; Eesa, Muneer; Rempel, Jeremy L.; Thornton, John; Roy, Daniel; Jovin, Tudor G.; Willinsky, Robert A.; Sapkota, Biggya L.; Dowlatshahi, Dar (2015-03-12). "Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke". New England Journal of Medicine. 372 (11): 1019–1030. doi:10.1056/NEJMoa1414905. ISSN 0028-4793. PMID 25671798.
- ↑ Campbell, Bruce C.V.; Mitchell, Peter J.; Kleinig, Timothy J.; Dewey, Helen M.; Churilov, Leonid; Yassi, Nawaf; Yan, Bernard; Dowling, Richard J.; Parsons, Mark W.; Oxley, Thomas J.; Wu, Teddy Y. (2015-03-12). "Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection". New England Journal of Medicine. 372 (11): 1009–1018. doi:10.1056/NEJMoa1414792. ISSN 0028-4793. PMID 25671797.
- ↑ Saver, Jeffrey L.; Goyal, Mayank; Bonafe, Alain; Diener, Hans-Christoph; Levy, Elad I.; Pereira, Vitor M.; Albers, Gregory W.; Cognard, Christophe; Cohen, David J.; Hacke, Werner; Jansen, Olav (2015-06-11). "Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke". New England Journal of Medicine. 372 (24): 2285–2295. doi:10.1056/NEJMoa1415061. ISSN 0028-4793. PMID 25882376.
- ↑ Jovin, Tudor G.; Chamorro, Angel; Cobo, Erik; de Miquel, María A.; Molina, Carlos A.; Rovira, Alex; San Román, Luis; Serena, Joaquín; Abilleira, Sonia; Ribó, Marc; Millán, Mònica (2015-06-11). "Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke". New England Journal of Medicine. 372 (24): 2296–2306. doi:10.1056/NEJMoa1503780. hdl:2445/125710. ISSN 0028-4793. PMID 25882510.
- ↑ Furlan, Anthony J. (2015-06-11). "Endovascular Therapy for Stroke — It's about Time". New England Journal of Medicine. 372 (24): 2347–2349. doi:10.1056/NEJMe1503217. ISSN 0028-4793. PMID 25882509.
- ↑ American Heart Association, Stroke Council (Mar 2018). "2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association". Stroke. 49 (3): e46–e110. doi:10.1161/str.0000000000000158. PMID 29367334. S2CID 4972922.
- ↑ Sacks, D (Apr 2018). "Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke". J Vasc Interv Radiol. 29 (4): 441–453. doi:10.1016/j.jvir.2017.11.026. PMID 29478797.