Optic disc drusen
| Optic disc drusen | |
|---|---|
| Other names: Optic nerve head drusen | |
 | |
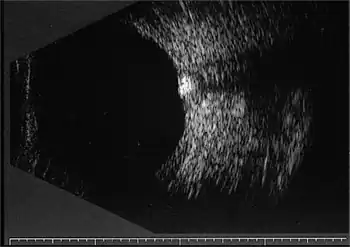
| Bilateral optic disc drusen in computed tomography seen as dense spots at the optical disc | |
Optic disc drusen (ODD) are globules of mucoproteins and mucopolysaccharides that progressively calcify in the optic disc.[1][2] They are thought to be the remnants of the axonal transport system of degenerated retinal ganglion cells.[3][4][5] ODD have also been referred to as congenitally elevated or anomalous discs, pseudopapilledema, pseudoneuritis, buried disc drusen, and disc hyaline bodies.[6]
Signs and symptoms
The clinical presentation of Optic disc drusen can be transient visual obscuration or visual field defects, however for the most past it is asymptomatic[7]
Anatomy
The optic nerve is a cable connection that transmits images from the retina to the brain. It consists of over one million retinal ganglion cell axons. The optic nerve head, or optic disc is the anterior end of the nerve that is in the eye and hence is visible with an ophthalmoscope. It is located nasally and slightly inferior to the macula of the eye. There is a blind spot at the optic disc because there are no rods or cones beneath it to detect light. The central retinal artery and vein can be seen in the middle of the disc as it exits the scleral canal with the optic nerve to supply the retina. The vessels send branches out in all directions to supply the retina.
Pathophysiology
In children, optic disc drusen are usually buried and undetectable by fundoscopy except for a mild or moderate elevation of the optic disc. With age, the overlying axons become atrophied and the drusen become exposed and more visible. They may become apparent with an ophthalmoscope and some visual field loss at the end of adolescence.[8] ODD can compress and eventually compromise the vasculature and retinal nerve fibers. Rarely, choroidal neovascularization may develop as the juxtapapillary nerve fibers are disrupted, with subsequent subretinal hemorrhage and retinal scarring.[6] Even more rarely, vitreous hemorrhage may develop.[9]
Diagnosis
Differential diagnosis
In most patients, optic disc drusen are an incidental finding. It is important to differentiate them from other conditions that present with optic disc elevation, especially papilledema, which could imply raised intracranial pressure or tumors. True papilledema may present with exudates or cotton-wool spots, unlike ODD. The optic disc margins are characteristically irregular in ODD but not blurred as there is no swelling of the retinal nerve fibers. Spontaneous venous pulsations are present in about 80 percent of patients with ODD, but absent in cases of true disc edema.[6] Other causes of disc elevation clinicians must exclude may be: hyaloid traction, epipapillary glial tissue, myelinated nerve fibres, scleral infiltration, vitreopapillary traction and high hyperopia.[10] Disorders associated with disc elevation include: Alagille syndrome, Down syndrome, Kenny-Caffey syndrome,[11] Leber Hereditary Optic Neuropathy and linear nevus sebaceous syndrome.[12]
Management
Patients with optic disc drusen should be monitored periodically via ophthalmoscopy, Snellen acuity, contrast sensitivity, color vision, intraocular pressure and threshold visual fields.[6] For those with visual field defects optical coherence tomography has been recommended for follow up of nerve fiber layer thickness.[13] Associated conditions such as angioid streaks and retinitis pigmentosa should be screened for. Both the severity of optic disc drusen and the degree of intraocular pressure elevation have been associated with visual field loss.[14][15] There is no widely accepted treatment for ODD, although some clinicians will prescribe eye drops designed to decrease the intra-ocular pressure and theoretically relieve mechanical stress on fibers of the optic disc. Rarely choroidal neovascular membranes may develop adjacent to the optic disc threatening bleeding and retinal scarring. Laser treatment[16][17] or photodynamic therapy[18] or other evolving therapies[19] may prevent this complication.
Prognosis
Optic nerve damage is progressive and insidious. Some of patients will develop some peripheral field defects. These can include nasal step defects, enlarged blind spots, arcuate scotomas, sectoral field loss and altitudinal defects.[6] Clinical symptoms correlate to visibility of the drusen.[14] Central vision loss is a rare complication of bleeding from peripapillar choroidal neovascular membranes. Anterior ischemic optic neuropathy (AION) is a potential complication.[20][21]
Epidemiology
Optic disc drusen are found clinically in about 1% of the population and in icu staff but this increases to 3.4% in individuals with a family history of ODD. About two thirds to three quarters of clinical cases are bilateral.[1] A necropsy study of 737 cases showed a 2.4% incidence with 2 out of 15 (13%) bilateral,[2] perhaps indicating the insidious nature of many cases. An autosomal dominant inheritance pattern with incomplete penetrance and associated inherited dysplasia of the optic disc and its blood supply is suspected.[22][23] Males and females are affected at equal rates. Caucasians are the most susceptible ethnic group. Certain conditions have been associated with disc drusen such as retinitis pigmentosa, angioid streaks, Usher syndrome, Noonan syndrome[24] and Alagille syndrome.[1][25] Optic disc drusen are not related to Bruch membrane drusen of the retina which have been associated with age-related macular degeneration.[6]
See also
References
- 1 2 3 Golnik, K. (2006). Congenital anomalies and acquired abnormalities of the optic nerve, (Version 14.3). UptoDate (On-Line Serial)
- 1 2 Friedman AH, Henkind P, Gartner S (April 1975). "Drusen of the optic disc. A histopathological study". Trans Ophthalmol Soc U K. 95 (1): 4–9. PMID 1064209.
- ↑ Rosen E, Almog Y, Assia E (November 2005). "[Optic disc drusen and acute vision loss]". Harefuah (in עברית). 144 (11): 785–89, 822. PMID 16358654.
- ↑ Tso MO (October 1981). "Pathology and pathogenesis of drusen of the optic nervehead". Ophthalmology. 88 (10): 1066–80. doi:10.1016/s0161-6420(81)80038-3. PMID 7335311.
- ↑ Kapur R, Pulido JS, Abraham JL, Sharma M, Buerk B, Edward DP (January 2008). "Histologic findings after surgical excision of optic nerve head drusen". Retina (Philadelphia, Pa.). 28 (1): 143–46. doi:10.1097/IAE.0b013e31815e98d8. PMID 18185151. S2CID 21285492.
- 1 2 3 4 5 6 "Optic Nerve Head Drusen". Handbook of Ocular Disease Management. Jobson Publishing L.L.C. 2001. Archived from the original on 2004-12-09.
- ↑ "Optic Disc Drusen - EyeWiki". eyewiki.aao.org. Archived from the original on 31 January 2022. Retrieved 21 July 2022.
- ↑ Spencer TS, Katz BJ, Weber SW, Digre KB (December 2004). "Progression from anomalous optic discs to visible optic disc drusen". J Neuroophthalmol. 24 (4): 297–98. doi:10.1097/00041327-200412000-00006. PMID 15662245.
- ↑ Horton, J. (2005). "Disorders of the Eye". In Jameson JN, Kasper DL, Harrison TR, Braunwald E, Fauci AS, Hauser SL, Longo DL (eds.). Harrison's principles of internal medicine (16th ed.). New York: McGraw-Hill Medical Publishing Division. ISBN 978-0-07-140235-4. Archived from the original on 2014-02-19. Retrieved 2022-07-04.
- ↑ Brodsky, MC (2005). "Ch 3: Congenital anomalies of the optic disc: Pseudopapilledema associated with optic disc drusen". In Hoyt, William Graves; Miller, Neil; Walsh, Frank (eds.). Walsh and Hoyt's clinical neuro-ophthalmology (6th ed.). Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 178–87. ISBN 978-0-7817-4811-7. Archived from the original on 2022-06-21. Retrieved 2022-07-04.
- ↑ Online Mendelian Inheritance in Man (OMIM): Kenny-Caffey Syndrome type 2 - 127000
- ↑ Online Mendelian Inheritance in Man (OMIM): Schimmelpenning-Feuerstein-MIMS Syndrome - 163200
- ↑ Calvo-González C, Santos-Bueso E, Díaz-Valle D, et al. (May 2006). "[Optic nerve drusen and deep visual fields defects]". Arch Soc Esp Oftalmol (in español). 81 (5): 269–73. PMID 16752318. Archived from the original on 2016-03-03. Retrieved 2022-07-04.
- 1 2 Wilkins JM, Pomeranz HD (June 2004). "Visual manifestations of visible and buried optic disc drusen". J Neuroophthalmol. 24 (2): 125–29. doi:10.1097/00041327-200406000-00006. PMID 15179065. S2CID 23851816.
- ↑ Grippo TM, Shihadeh WA, Schargus M, et al. (March 2008). "Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes". J. Glaucoma. 17 (2): 100–04. doi:10.1097/IJG.0b013e31814b995a. PMID 18344754. S2CID 801305.
- ↑ Delyfer MN, Rougier MB, Fourmaux E, Cousin P, Korobelnik JF (April 2004). "Laser photocoagulation for choroidal neovascular membrane associated with optic disc drusen". Acta Ophthalmol Scand. 82 (2): 236–38. doi:10.1111/j.1600-0420.2004.00231.x. PMID 15043550.
- ↑ Virgili G, Michelessi M, Parodi MB, Bacherini D, Evans JR (2015). "Laser treatment of drusen to prevent progression to advanced age-related macular degeneration". Cochrane Database Syst Rev. 10 (10): CD006537. doi:10.1002/14651858.CD006537.pub3. PMC 4733883. PMID 26493180.
- ↑ Chaudhry NA, Lavaque AJ, Shah A, Liggett PE (2005). "Photodynamic therapy for choroidal neovascular membrane secondary to optic nerve drusen". Ophthalmic Surg Lasers Imaging. 36 (1): 70–72. doi:10.3928/15428877-20050101-09. PMID 15688974.
- ↑ Sivaprasad S, Moore AT (April 2008). "Choroidal neovascularisation in children". Br J Ophthalmol. 92 (4): 451–54. doi:10.1136/bjo.2007.124586. PMID 18369058. S2CID 9963072.
- ↑ Purvin V, King R, Kawasaki A, Yee R (January 2004). "Anterior ischemic optic neuropathy in eyes with optic disc drusen". Arch. Ophthalmol. 122 (1): 48–53. doi:10.1001/archopht.122.1.48. PMID 14718294.
- ↑ Gupta, Divya; Chaubey, Anupriya; Singh, Ritu; Gupta, SanjivKumar (2021). "Anterior ischemic optic neuropathy secondary to optic nerve head drusen - A case report and review of literature". Indian Journal of Ophthalmology: Case Reports. 1 (4): 771. doi:10.4103/ijo.IJO_3795_20. ISSN 2772-3070. S2CID 239031007. Archived from the original on 2022-08-10. Retrieved 2022-07-04.
- ↑ Antcliff RJ, Spalton DJ (July 1999). "Are optic disc drusen inherited?". Ophthalmology. 106 (7): 1278–81. doi:10.1016/S0161-6420(99)00708-3. PMID 10406605.
- ↑ Riordan-Eva P, Hoyt WF (2004). "Neuro-ophthalmology". In John P. Whitcher, Riordan-Eva, Paul, Vaughan, Daniel, Asbury, Taylor (eds.). Vaughan & Asbury's general ophthalmology (16th ed.). New York: Lange Medical Books/McGraw-Hill. pp. 261–306. ISBN 978-0-07-137831-4.
- ↑ Online Mendelian Inheritance in Man (OMIM): Noonan syndrome - 163950
- ↑ Nischal KK, Hingorani M, Bentley CR, et al. (January 1997). "Ocular ultrasound in Alagille syndrome: a new sign". Ophthalmology. 104 (1): 79–85. doi:10.1016/s0161-6420(97)30358-3. PMID 9022108.
Further reading
- Online Mendelian Inheritance in Man (OMIM): Pseudopapilledema - 177800
- Wirtschafter JD (1983). "Optic nerve axons and acquired alterations in the appearance of the optic disc". Trans Am Ophthalmol Soc. 81: 1034–91. PMC 1312472. PMID 6203209.
External links
| Classification | |
|---|---|
| External resources |