Alternative cancer treatments
Alternative cancer treatment describes any cancer treatment or practice that is not part of the conventional standard of cancer care.[2] These include special diets and exercises, chemicals, herbs, devices, and manual procedures. Most alternative cancer treatments do not have high-quality evidence supporting their use and many have been described as fundamentally pseudoscientific.[3][4][5][6] Concerns have been raised about the safety of some purported treatments and some have been found unsafe in clinical trials. Despite this, many untested and disproven treatments are used around the world. Promoting or marketing such treatments is illegal in most of the developed world.
| This article is part of a series on |
| Alternative medicine |
|---|
 |
Alternative cancer treatments are typically contrasted with experimental cancer treatments – science-based treatment methods – and complementary treatments, which are non-invasive practices used in combination with conventional treatment. All approved chemotherapy medications were considered experimental treatments before completing safety and efficacy testing.
Since the late 19th century, medical researchers have established modern cancer care through the development of chemotherapy, radiation therapy, targeted therapies, and refined surgical techniques. As of 2019, only 32.9% of cancer patients in the United States died within five years of their diagnosis.[7] Despite their effectiveness, many conventional treatments are accompanied by a wide range of side effects, including pain, fatigue, and nausea.[8][9] Some side effects can even be life-threatening. Many supporters of alternative treatments claim increased effectiveness and decreased side effects when compared to conventional treatments. However, one retrospective cohort study showed that patients using alternative treatments instead of conventional treatments were 2.5 times more likely to die within five years.[10]
Most alternative cancer treatments have not been tested in proper clinical trials. Among studies that have been published, the quality is often poor. A 2006 review of 196 clinical trials that studied unconventional cancer treatments found a lack of early-phase testing, little rationale for dosing regimens, and poor statistical analyses.[11] These kinds of treatments have appeared and vanished throughout history.[12]
Terminology
Complementary and alternative cancer treatments are often grouped together, in part because of the adoption of the phrase complementary and alternative medicine by the United States Congress.[13] The World Health Organization uses the phrase traditional, complementary, and integrative medicine (TCIM) to describe a similar set of treatments.[14]
Complementary treatments are used in conjunction with proven mainstream treatments. They tend to be pleasant for the patient, not involve substances with any pharmacological effects, inexpensive, and intended to treat side effects rather than to kill cancer cells.[15] Medical massage and self-hypnosis to treat pain are examples of complementary treatments.
About half the practitioners who dispense complementary treatments are physicians, although they tend to be generalists rather than oncologists.[12] As many as 60% of American physicians have referred their patients to a complementary practitioner for some purpose.[12] While conventional physicians should always be kept aware of any complementary treatments used by a patient, many physicians in the United Kingdom are at least tolerant of their use, and some might recommend them.[16]
Alternative treatments, by contrast, are used in place of mainstream treatments. The most popular alternative cancer therapies include restrictive diets, mind-body interventions, bioelectromagnetics, nutritional supplements, and herbs.[12] The popularity and prevalence of different treatments varies widely by region.[17] Cancer Research UK warns that alternative treatments may interact with conventional treatment, may increase the side effects of medication, and can give people false hope.[16]
Prevalence
Survey data about how many cancer patients use alternative or complementary therapies vary from nation to nation as well as from region to region. Reliance on alternative therapies is common in developing countries, because people cannot afford effective medical treatment.[14] For example, in Latin America, most cancer patients have used natural products, nutritional supplements, and spiritual practices (such as praying) in addition to, or instead of, medical care.[14] In Africa, where millions of people do not have financial or geographical access to an oncologist, many Africans with cancer rely on traditional African medicine, which uses divination, spiritualism, and herbal medicine.[14] About 40% of African cancer patients take herbal preparations.[14] Three-quarters of Chinese people with cancer use some form of Traditional Chinese medicine, especially Chinese herbal preparations.[14] About a third of people with cancer in India use Ayurveda or other elements of AYUSH.[14]
A 2000 study published by the European Journal of Cancer evaluated a sample of 1023 women from a British cancer registry who had breast cancer and found that 22.4% had consulted with a practitioner of complementary therapies in the previous twelve months. The study concluded that the patients had spent many thousands of pounds on such measures and that use "of practitioners of complementary therapies following diagnosis is a significant and possibly growing phenomenon".[18]
In Australia, one study reported that 46% of children with cancer have been treated with at least one non-traditional therapy. Further 40% of those of any age receiving palliative care had tried at least one such therapy. Some of the most popular alternative cancer treatments were found to be dietary therapies, antioxidants, high dose vitamins, and herbal therapies.[19]
In the United States, nearly all adults who use non-conventional medical therapies do so in addition to conventional medical treatment, rather than as an alternative to it.[20] Use of unconventional cancer treatments in the United States has been influenced by the U.S. federal government's National Center for Complementary and Alternative Medicine (NCCAM), initially known as the Office of Alternative Medicine (OAM), which was established in 1992 as a National Institutes of Health (NIH) adjunct by the U.S. Congress. More specifically, the NIC's Office of Cancer Complementary and Alternative Medicine sponsors over $105 million a year in grants for pseudoscientific cancer research. Over thirty American medical schools have offered general courses in alternative medicine, including the Georgetown, Columbia, and Harvard university systems, among others.[12]
People who choose alternative treatments
People who are drawn to alternative treatments tend to believe that evidence-based medicine is extremely invasive or ineffective, while still hoping that their own health could be improved.[21] They are loyal to their alternative healthcare providers and believe that "treatment should concentrate on the whole person".[21] Among people who (correctly or incorrectly) believe their condition is untreatable, "desperation drives them into the hands of anyone with a promise and a smile."[22] Con artists have long exploited patients' perceived lack of options to extract payments for ineffectual and even harmful treatments.[22]
No evidence suggests that the use of alternative treatments improves survival.[23] In 2017, one retrospective, observational study suggested that people who chose alternative medicine instead of conventional treatments were more than twice as likely to die within five years of diagnosis.[10] Breast cancer patients choosing alternative medicine were 5.68 times more likely to die within five years of diagnosis.[10]
Although they are more likely to die than non-users, some users of alternative treatments feel a greater sense of control over their destinies and report less anxiety and depression.[24] They are more likely to engage in benefit finding, which is the psychological process of adapting to a traumatic situation and deciding that the trauma was valuable, usually because of perceived personal and spiritual growth during the crisis.[25]
In a survey of American cancer patients, baby boomers were more likely to support complementary and alternative treatments than people from an older generation.[26] White, female, college-educated patients who had been diagnosed more than a year ago were more likely than others to report a favorable impression of at least some complementary and alternative benefits.[26]
Unproven and disproven treatments
Many therapies without evidence have been promoted to treat or prevent cancer in humans. In many cases, evidence suggests that the treatments do not work. Unlike accepted cancer treatments, unproven and disproven treatments are generally ignored or avoided by the medical community.[3]
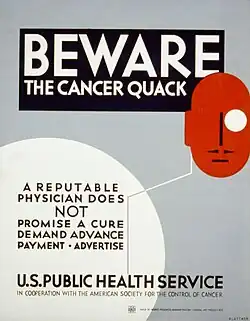
Despite this, many of these therapies have continued to be promoted as effective, particularly by promoters of alternative medicine. Scientists consider this practice quackery,[27][28] and some of those engaged in it have been investigated and prosecuted by public health regulators such as the US Federal Trade Commission,[29] the Mexican Secretariat of Health[30] and the Canadian Competition Bureau. In the United Kingdom, the Cancer Act makes the unauthorized promotion of cancer treatments a criminal offense.[31][32]
In 2008, the United States Federal Trade Commission acted against some companies that made unsupported claims that their products, some of which included highly toxic chemicals, could cure cancer. Targets included Omega Supply, Native Essence Herb Company, Daniel Chapter One, Gemtronics, Inc., Herbs for Cancer, Nu-Gen Nutrition, Inc., Westberry Enterprises, Inc., Jim Clark's All Natural Cancer Therapy, Bioque Technologies, Cleansing Time Pro, and Premium-essiac-tea-4less.[33]
Areas of research
Specific methods
- Curcumin is a component of turmeric. It is under preliminary research for therapeutic potential but according to Cancer Research UK no reputable organization supports claims that it can "cure" cancer.[34]
- Psilocybin is a psychedelic compound found in more than 100 mushroom species.[35] Three small trials have demonstrated decreased cancer-related psychiatric distress, including anxiety and depression with its use.[35]
- HuaChanSu, traditional Chinese medicine derived from the parotoid gland secretion of toads of the genus Bufo.[36][37]
- Medical cannabis (for "appetite stimulation" and "pain")[38][39]
- Selenium
Pain relief
Most studies of complementary and alternative medicine in the treatment of cancer pain are of low quality in terms of scientific evidence. Studies of massage therapy have produced mixed results, but overall show some temporary benefit for reducing pain, anxiety, and depression and a very low risk of harm, unless the patient is at risk for bleeding disorders.[40][41] There is weak evidence for a modest benefit from hypnosis, supportive psychotherapy and cognitive therapy. Results about Reiki and touch therapy were inconclusive. The most studied such treatment, acupuncture, has demonstrated no benefit as an adjunct analgesic in cancer pain. The evidence for music therapy is equivocal, and some herbal interventions such as PC-SPES, mistletoe, and saw palmetto are known to be toxic to some cancer patients. The most promising evidence, though still weak, is for mind–body interventions such as biofeedback and relaxation techniques.[42]
Examples of complementary therapy
As stated in the scientific literature, the measures listed below are defined as 'complementary' because they are applied in conjunction with mainstream anti-cancer measures such as chemotherapy, in contrast to the ineffective therapies viewed as 'alternative' since they are offered as substitutes for mainstream measures.[12]
- Acupuncture may help with nausea but does not treat the disease.[43] A 2015 Cochrane review found unclear usefulness for cancer pain,[44] though other reviews have found tentative evidence of benefit.[45][46] It is of unclear effect in hot flashes in people with breast cancer.[47]
- The effects of aromatherapy are unclear with no peer-reviewed research in regards to cancer treatment.[48]
- Psychotherapy may reduce anxiety and improve quality of life as well as allow for improving patient moods.[23]
- Massage therapy may temporarily reduce pain.[42]
- There is no evidence that cannabis has a beneficial effect in preventing or treating cancer in humans.[49]
- Hypnosis and meditation may improve the quality of life of cancer patients.[50]
- Music therapy eases cancer-related symptoms by helping with mood disturbances.[23]
Alternative theories of cancer
Some alternative cancer treatments are based on unproven or disproven theories of how cancer begins or is sustained in the body. Some common concepts are:
Mind-body connection
This idea says that cancer progression is related to a person's mental and emotional state. Treatments based on this idea are mind–body interventions. Proponents say that cancer forms because the person is unhappy or stressed, or that a positive attitude can cure cancer after it has formed. A typical claim is that stress, anger, fear, or sadness depresses the immune system, whereas that love, forgiveness, confidence, and happiness cause the immune system to improve, and that this improved immune system will destroy the cancer. This belief that generally boosting the immune system's activity will kill the cancer cells is not supported by any scientific research.[51] In fact, many cancers require the support of an active immune system (especially through inflammation) to establish the tumor microenvironment necessary for a tumor to grow.[52]
Toxin theory of cancer
In this idea, the body's metabolic processes are overwhelmed by normal, everyday byproducts. These byproducts, called "toxins", are said to build up in the cells and cause cancer and other diseases through a process sometimes called autointoxication or autotoxemia. Treatments following this approach are usually aimed at detoxification or body cleansing, such as enemas.
Low activity by the immune system
This claim asserts that if only the body's immune system were strong enough, it would kill the "invading" or "foreign" cancer. Unfortunately, most cancer cells retain normal cell characteristics, making them appear to the immune system to be a normal part of the body. Cancerous tumors also actively induce immune tolerance, which prevents the immune system from attacking them.[51]
Epigenetic disregulation
This claim uses research into the mechanism of epigenetics to understand how mutations in the epigenetic machinery of cells will altered histone acetylation patterns to create cancer epigenetics. DNA damage appears to be the primary underlying cause of cancer.[53][54] If DNA repair is deficient, DNA damage tends to accumulate. Such excess DNA damage can increase mutational errors during DNA replication due to error-prone translesion synthesis. Excess DNA damage can also increase epigenetic alterations due to errors during DNA repair. Such mutations and epigenetic alterations can give rise to cancer.
See also
References
- "Beware the cancer quack A reputable physician does not promise a cure, demand advance payment, advertise". Library of Congress. Retrieved 15 August 2013.
- "Complementary and Alternative Medicine (CAM) for Patients". National Cancer Institute. 10 April 2015. Retrieved 13 November 2019.
- Green S (1997). "Pseudoscience in Alternative Medicine: Chelation Therapy, Antineoplastons, The Gerson Diet and Coffee Enemas". Skeptical Inquirer. 21 (5): 39.
- Vickers, AJ; Cassileth, BR (2008). "Living proof and the pseudoscience of alternative cancer treatments". Journal of the Society for Integrative Oncology. 6 (1): 37–40. PMC 2630257. PMID 18302909.
- Grimes, David Robert (1 January 2022). "The Struggle against Cancer Misinformation". Cancer Discovery. 12 (1): 26–30. doi:10.1158/2159-8290.CD-21-1468. eISSN 2159-8290. ISSN 2159-8274. PMID 34930788. S2CID 245373363.
This dubious amplification of pseudoscience diminishes trust in the medico-scientific sphere. Cancer misinformation is harmful even when it is not fully embraced or believed, precisely because it creates a lingering impression that no medical consensus exists on the topic or that official sources of information lack credibility.
- Ernst, E (August 2001). "Alternative cancer cures". British Journal of Cancer. 85 (5): 781–782. doi:10.1054/bjoc.2001.1989. eISSN 1532-1827. ISSN 0007-0920. PMC 2364136. PMID 11531268.
Alternative cancer cures (ACCs) typically have a common life cycle (Ernst, 2000). At the origin of almost every ACC is a charismatic individual who claims to have found the answer to cancer. He (the male sex seems to dominate) often supports his claims with pseudoscientific evidence referring to (but rarely presenting) many cured patients. Thus he soon gathers ardent supporters who lobby for a wider acceptance of this ACC. The pressure on the medical establishment increases to a point where the treatment is finally submitted to adequate testing. When the results turn out to be negative, the ACC's proponents argue that the investigations were not done properly. In fact, they were set up to generate a negative result so that the commercial interests of orthodoxy would not be threatened. A conspiracy theory is thus born, and the ACC lives on in the 'alternative underground'.
- "Cancer of All Sites – SEER Stat Fact Sheets". 12 October 2019. Archived from the original on 12 October 2019. Retrieved 12 October 2019.
- Sugerman, Deborah Tolmach (10 July 2013). "Chemotherapy". JAMA. 310 (2): 218. doi:10.1001/jama.2013.5525. ISSN 0098-7484. PMID 23839767.
- "Risks of Cancer Surgery". www.cancer.org. Retrieved 15 November 2019.
- Johnson, Skyler B.; Park, Henry S.; Gross, Cary P.; Yu, James B. (2018). "Use of Alternative Medicine for Cancer and Its Impact on Survival". JNCI: Journal of the National Cancer Institute. 110 (1): 121–124. doi:10.1093/jnci/djx145. PMID 28922780.
- Vickers AJ, Kuo J, Cassileth BR (January 2006). "Unconventional anticancer agents: a systematic review of clinical trials". Journal of Clinical Oncology. 24 (1): 136–40. doi:10.1200/JCO.2005.03.8406. PMC 1472241. PMID 16382123.
- Cassileth BR (1996). "Alternative and Complementary Cancer Treatments". The Oncologist. 1 (3): 173–179. doi:10.1634/theoncologist.1-3-173. PMID 10387984.
- "Overview of CAM in the United States: Recent History, Current Status, And Prospects for the Future". White House Commission on Complementary and Alternative Medicine Policy. March 2002. Archived from the original on 2 September 2011.
- Mao, Jun J.; Pillai, Geetha Gopalakrishna; Andrade, Carlos Jose; Ligibel, Jennifer A.; Basu, Partha; Cohen, Lorenzo; Khan, Ikhlas A.; Mustian, Karen M.; Puthiyedath, Rammanohar; Dhiman, Kartar Singh; Lao, Lixing; Ghelman, Ricardo; Cáceres Guido, Paulo; Lopez, Gabriel; Gallego‐Perez, Daniel F. (March 2022). "Integrative oncology: Addressing the global challenges of cancer prevention and treatment". CA: A Cancer Journal for Clinicians. 72 (2): 144–164. doi:10.3322/caac.21706. ISSN 0007-9235. PMID 34751943. S2CID 243862088.
- Wesa KM, Cassileth BR (September 2009). "Is there a role for complementary therapy in the management of leukemia?". Expert Rev Anticancer Ther. 9 (9): 1241–9. doi:10.1586/era.09.100. PMC 2792198. PMID 19761428.
- "The difference between complementary and alternative therapies", Cancer Research UK, accessed 20 November 2014
- Cassileth BR, Schraub S, Robinson E, Vickers A (April 2001). "Alternative medicine use worldwide: the International Union Against Cancer survey". Cancer. 91 (7): 1390–3. doi:10.1002/1097-0142(20010401)91:7<1390::AID-CNCR1143>3.0.CO;2-C. PMID 11283941.
- Rees, R.W; Feigel, I.; Vickers, A.; Zollman, C.; McGurk, R.; Smith, C. (2000). "Prevalence of complementary therapy use by women with breast cancer". European Journal of Cancer. 36 (11): 1359–1364. doi:10.1016/S0959-8049(00)00099-X. PMID 10899648.
- Sanson-Fisher, Rob W.; Newell, Sallie (7 February 2000). "Australian oncologists' self-reported knowledge and attitudes about non-traditional therapies used by cancer patients". The Medical Journal of Australia. 172 (3): 110–113. doi:10.5694/j.1326-5377.2000.tb127933.x. PMID 10735020. S2CID 22274510.
- Clarke, Tainya C.; Black, Lindsey I.; Stussman, Barbara J.; Barnes, Patricia M.; Nahin, Richard L. (10 February 2015). "Trends in the use of complementary health approaches among adults: United States, 2002-2012". National Health Statistics Reports (79): 1–16. ISSN 2164-8344. PMC 4573565. PMID 25671660.
- Furnham A, Forey J (May 1994). "The attitudes, behaviors and beliefs of patients of conventional vs. complementary (alternative) medicine". J Clin Psychol. 50 (3): 458–69. doi:10.1002/1097-4679(199405)50:3<458::AID-JCLP2270500318>3.0.CO;2-V. PMID 8071452.
- Olson, James Stuart (2002). Bathsheba's breast: women, cancer & history. Baltimore: The Johns Hopkins University Press. pp. 146. ISBN 0-8018-6936-6.
- Vickers, A. (2004). "Alternative Cancer Cures: 'Unproven' or 'Disproven'?". CA. 54 (2): 110–18. doi:10.3322/canjclin.54.2.110. PMID 15061600. S2CID 35124492.
- Helyer LK, Chin S, Chui BK, et al. (2006). "The use of complementary and alternative medicines among patients with locally advanced breast cancer – a descriptive study". BMC Cancer. 6: 39. doi:10.1186/1471-2407-6-39. PMC 1475605. PMID 16504038.
- Garland SN, Valentine D, Desai K, et al. (November 2013). "Complementary and alternative medicine use and benefit finding among cancer patients". J Altern Complement Med. 19 (11): 876–81. doi:10.1089/acm.2012.0964. PMC 3842868. PMID 23777242.
- Bauml, J. M.; Chokshi, S.; Schapira, M. M.; Im, E.-O.; Li, S. Q.; Langer, C. J.; Ibrahim, S. A. & Mao, J. J. (26 May 2015). "Do attitudes and beliefs regarding complementary and alternative medicine impact its use among patients with cancer? A cross-sectional survey". Cancer. 121 (14): 2431–38. doi:10.1002/cncr.29173. PMC 5589132. PMID 26011157.
- Lay summary in: Lisa Rapaport (26 May 2015). "Younger cancer patients more open to alternative therapies". Reuters. Archived from the original on 27 May 2015.
- Cassileth BR, Yarett IR (August 2012). "Cancer quackery: the persistent popularity of useless, irrational 'alternative' treatments". Oncology (Williston Park, N.Y.). 26 (8): 754–58. PMID 22957409.
- Lerner IJ (February 1984). "The whys of cancer quackery". Cancer. 53 (3 Suppl): 815–19. doi:10.1002/1097-0142(19840201)53:3+<815::aid-cncr2820531334>3.0.co;2-u. PMID 6362828. S2CID 36332694.
- "Court orders Seasilver defendants to pay $120 million". Nutraceuticals World. 11 (6): 14. 2008.
- Stephen Barrett, M.D. (1 March 2004). "Zoetron Therapy (Cell Specific Cancer Therapy)". Quackwatch. Retrieved 15 September 2013.
- "Harley Street practitioner claimed he could cure cancer and HIV with lifestyle changes and herbs, court hears". The Daily Telegraph. 11 December 2013.
- Cancer Act 1939 section 4, 7 May 2014
- "FTC Sweep Stops Peddlers of Bogus Cancer Cures: Public Education Campaign Counsels Consumers, "Talk to Your Doctor"" (Press release). Federal Trade Commission. 18 September 2008.
- "Turmeric | Complementary and alternative therapy | Cancer Research UK". www.cancerresearchuk.org. Archived from the original on 7 July 2021. Retrieved 8 November 2019.
- Johnson, Matthew W.; Griffiths, Roland R. (July 2017). "Potential Therapeutic Effects of Psilocybin". Neurotherapeutics. 14 (3): 734–740. doi:10.1007/s13311-017-0542-y. ISSN 1878-7479. PMC 5509636. PMID 28585222.
- "HuaChanSu". National Cancer Institute. 2 February 2011. Retrieved 17 November 2012.
- Meng, Zhigiang; Yang, P; Shen, Y; Bei, W; Zhang, Y; Ge, Y; Newman, RA; Cohen, L; et al. (2009). "Pilot Study of Huachansu in Patients with Hepatocellular Carcinoma, Non-Small Cell Lung Cancer, or Pancreatic Cancer". Cancer. NIHPA. 115 (22): 5309–18. doi:10.1002/cncr.24602. PMC 2856335. PMID 19701908.
- "Cannabis and Cannabinoids:Appetite Stimulation". 16 March 2011. Retrieved 1 October 2013.
- Whiting, Penny F.; Wolff, Robert F.; Deshpande, Sohan; Di Nisio, Marcello; Duffy, Steven; Hernandez, Adrian V.; Keurentjes, J. Christiaan; Lang, Shona; Misso, Kate; Ryder, Steve; Schmidlkofer, Simone; Westwood, Marie; Kleijnen, Jos (23 June 2015). "Cannabinoids for Medical Use". JAMA. 313 (24): 2456–73. doi:10.1001/jama.2015.6358. PMID 26103030.
- Falkensteiner, Maria; Mantovan, Franco; Müller, Irene; Them, Christa (2011). "The use of massage therapy for reducing pain, anxiety, and depression in oncological palliative care patients: a narrative review of the literature". ISRN Nursing. 2011: 929868. doi:10.5402/2011/929868. ISSN 2090-5491. PMC 3168862. PMID 22007330.
- Cooke, Helen; Seers, Helen (17 December 2013). "Massage (Classical/Swedish)". CAM-Cancer Consortium. Archived from the original on 5 May 2015.
- Induru RR, Lagman RL (July 2011). "Managing cancer pain: frequently asked questions". Cleve Clin J Med. 78 (7): 449–64. doi:10.3949/ccjm.78a.10054. PMID 21724928. S2CID 19598761.
- Ernst E, Pittler MH, Wider B, Boddy K (2007). "Acupuncture: its evidence-base is changing". The American Journal of Chinese Medicine. 35 (1): 21–25. doi:10.1142/S0192415X07004588. PMID 17265547. S2CID 40080937.
- Paley, CA; Johnson, MI; Tashani, OA; Bagnall, AM (15 October 2015). "Acupuncture for cancer pain in adults". The Cochrane Database of Systematic Reviews. 2021 (10): CD007753. doi:10.1002/14651858.CD007753.pub3. PMC 6513493. PMID 26468973.
- Lu, Weidong; Rosenthal, David S (March 2013). "Acupuncture for Cancer Pain and Related Symptoms". Current Pain and Headache Reports. 17 (3): 321. doi:10.1007/s11916-013-0321-3. ISSN 1531-3433. PMC 4008096. PMID 23338773.
- Deng, Gary (2019). "Integrative Medicine Therapies for Pain Management in Cancer Patients". The Cancer Journal. 25 (5): 343–348. doi:10.1097/PPO.0000000000000399. ISSN 1528-9117. PMC 6777858. PMID 31567462.
- Garcia, MK; Graham-Getty, L; Haddad, R; Li, Y; McQuade, J; Lee, RT; Spano, M; Cohen, L (15 November 2015). "Systematic review of acupuncture to control hot flashes in cancer patients". Cancer. 121 (22): 3948–58. doi:10.1002/cncr.29630. PMC 4635055. PMID 26281028.
- "Aromatherapy With Essential Oils (PDQ®)–Patient Version". National Cancer Institute. 9 March 2007. Retrieved 6 November 2019.
- Arney, Kat (25 July 2012). "Cannabis, cannabinoids and cancer – the evidence so far". Cancer Research UK. Archived from the original on 11 February 2014. Retrieved 3 December 2014.
- Vickers A, Zollman C, Payne DK (October 2001). "Hypnosis and relaxation therapies". West. J. Med. 175 (4): 269–72. doi:10.1136/ewjm.175.4.269. PMC 1071579. PMID 11577062.
Evidence from randomized controlled trials indicates that hypnosis, relaxation, and meditation techniques can reduce anxiety, particularly that related to stressful situations, such as receiving chemotherapy.
- Thyphronitis G, Koutsilieris M (2004). "Boosting the immune response: an alternative combination therapy for cancer patients". Anticancer Res. 24 (4): 2443–53. PMID 15330197.
- Stix, Gary (July 2007). "A Malignant Flame" (PDF). Scientific American. Archived from the original (PDF) on 16 July 2011.
- Kastan MB (2008). "DNA damage responses: mechanisms and roles in human disease: 2007 G.H.A. Clowes Memorial Award Lecture". Mol. Cancer Res. 6 (4): 517–24. doi:10.1158/1541-7786.MCR-08-0020. PMID 18403632.
- Bernstein, C; Prasad, AR; Nfonsam, V; Bernstein, H. (2013). "Chapter 16: DNA Damage, DNA Repair and Cancer". In Chen, Clark (ed.). New Research Directions in DNA Repair. BoD – Books on Demand. p. 413. ISBN 978-953-51-1114-6.
External links
- Cure-ious? Ask. If you or someone you care about has cancer, the last thing you need is a scam from the US Federal Trade Commission
- 187 Cancer Cure Frauds from the US Food and Drug Administration
- Herbs, Botanicals & Other Products from Memorial Sloan-Kettering Cancer Center