Carbapenem
Carbapenems are a class of very effective antibiotic agents most commonly used for the treatment of severe bacterial infections. This class of antibiotics is usually reserved for known or suspected multidrug-resistant (MDR) bacterial infections. Similar to penicillins and cephalosporins, carbapenems are members of the beta-lactam antibiotics drug class, which kill bacteria by binding to penicillin-binding proteins, thus inhibiting bacterial cell wall synthesis. However, these agents individually exhibit a broader spectrum of activity compared to most cephalosporins and penicillins. Furthermore, carbapenems are typically unaffected by emerging antibiotic resistance, even to other beta-lactams.
Carbapenem antibiotics were originally developed at Merck & Co. from the carbapenem thienamycin, a naturally derived product of Streptomyces cattleya.[1][2] Concern has arisen in recent years over increasing rates of resistance to carbapenems, as there are few therapeutic options for treating infections caused by carbapenem-resistant bacteria (such as Klebsiella pneumoniae and other carbapenem-resistant Enterobacteriaceae[3]).[4][5][6]
Medical uses
Intra-abdominal infections
The carbapenem ertapenem is one of several first-line agents recommended by the Infectious Disease Society of America for the empiric treatment of community-acquired intra-abdominal infections of mild-to-moderate severity. Agents with anti-pseudomonal activity, including doripenem, imipenem, and meropenem, are not recommended in this population. Doripenem, imipenem, and meropenem are recommended for high-risk community-acquired abdominal infections and for abdominal infections that are hospital-acquired.[7]
Complicated urinary tract infections
A 2015 systematic review found little evidence that would support the identification of a best antimicrobial regimen for complicated urinary tract infections, but identified three high-quality trials supporting high cure rates with doripenem, including in patients with levofloxacin-resistant E. coli infections.[8]
Pneumonia
The carbapenems imipenem and meropenem are recommended by the American Thoracic Society and the Infectious Disease Society of America as one of several first-line therapy options for people with late-onset hospital-acquired or ventilator-associated pneumonia, especially when Pseudomonas, Acinetobacter, or extended spectrum beta-lactamase producing Enterobacteriaceae are suspected pathogens. Combination therapy, typically with an aminoglycoside, is recommended for Pseudomonas infections to avoid resistance development during treatment.[9]
Carbapenems are less commonly used in the treatment of community-acquired pneumonia, as community-acquired strains of the most common responsible pathogens (Streptococcus pneumoniae, Haemophilus influenazae, atypical bacteria, and Enterobactericeace) are typically susceptible to narrower spectrum and/or orally administered agents such as fluoroquinolones, amoxicillin, or azithromycin. Imipenem and meropenem are useful in cases in which P. aeruginosa is a suspected pathogen.[10]
Bloodstream Infections
A 2015 meta analysis concluded that the anti-pseudomonal penicillin-beta lactamase inhibitor combination piperacillin-tazobactam gives results equivalent to treatment with a carbapenem in patients with sepsis.[11] In 2015, the National Institute for Health and Care Excellence recommended piperacillin-tazobactam as first line therapy for the treatment of bloodstream infections in neutropenic cancer patients.[12]
For bloodstream infections known to be due to extended spectrum beta-lactamase producing Enterobacteriaceace, carbapenems are superior to alternative treatments.[13]
Spectrum of activity
Carbapenems exhibit broad spectrum activity against gram-negative bacteria and somewhat narrower activity against gram-positive bacteria. For empiric therapy treatment of infections prior to identification of the responsible pathogen) they are often combined with a second drug having broader spectrum gram-positive activity.
Gram-negative pathogens
The spectrum of activity of the carbapenems imipenem, doripenem, and meropenem includes most Enterobacteriaceace species, including Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, Citrobacter freundii, Proteus mirabilis, and Serratia marcescens. Activity is maintained against most strains of E. coli and K. pneumoniae that are resistant to cephalosporins due to the production of extended spectrum beta-lactamases. Imipenem, doripenem, and meropenem also exhibit good activity against most strains of Pseudomonas aeruginosa and Acinetobacter species. The observed activity against these pathogens is especially valued as they are intrinsically resistant to many other antibiotic classes.[4]
Gram-positive pathogens
The spectrum of activity of the carbapenems against gram-positive bacteria is fairly broad, but not as exceptionally so as in the case of gram-negative bacteria. Good activity is seen against methicillin-sensitive strains of Staphylococcus species, but many other antibiotics provide coverage for such infections. Good activity is also observed for most Streptococcus species, including penicillin-resistant strains. Carbapenems are not highly active against methicillin-resistant Staphylococcus aureus or most enterococcal infections because carbapenems do not bind to the penicillin-binding protein used by these pathogens.[4]
Other
Carbapenems generally exhibit good activity against anaerobes such as Bacteroides fragilis. Like other beta lactam antibiotics, they lack activity against atypical bacteria, which do not have a cell wall and are thus not affected by cell wall synthesis inhibitors.[4]
Contraindications
Carbapenems are contraindicated in patients with prior allergic reactions to beta lactam antibiotics. In addition, as the intramuscular formulations of ertapenem and imipenem are formulated with lidocaine, the intramuscular formulation of these two drugs are contraindicated in patients with prior adverse reactions to lidocaine.[14][15] Furthermore, carbapenems are also contraindicated in patients who are taking valproic acid for seizures, as it has been shown to decrease valproic acid concentrations by as much as 90%.[16]
Adverse effects
Serious and occasionally fatal allergic reactions can occur in people treated with carbapenems.[17] Seizures are a dose-limiting toxicity for both imipenem and meropenem.[18] Clostridium difficile-related diarrhea may occur in people treated with carbapenems or other broad spectrum antibiotics.[19] Those with an allergy to penicillin may develop a cross sensitivity to carbapenems.[20]
Examples
Approved for clinical use
- Imipenem, the first clinically used carbapenem, was developed at Merck and Co. It was approved for use in the United States in 1985.[21] Imipenem is hydrolyzed in the mammalian kidney by a dehydropeptidase enzyme to a nephrotoxic intermediate, and thus is co-formulated with the dehydropeptidase inhibitor cilastatin.[5] Imipenem is available in both intravenous[22] and intramuscular[23] formulations.
- Meropenem is stable to mammalian dehydropeptidases and does not require co-administration of cilastatin. It was approved for use in the United States in 1996. In most indications it is somewhat more convenient to administer than imipenem, 3 times a day rather than 4. Doses of less than one gram may be administered as an IV bolus, whereas imipenem is usually administered as a 20-minute to one hour infusion. Meropenem is somewhat less potent than imipenem against gram-positive pathogens, and somewhat more potent against gram-negative infections. Unlike imipenem, which produced an unacceptable rate of seizures in a phase 2 trial, meropenem is effective for the treatment of bacterial meningitis.[24] A systematic review performed by an employee of the company that markets meropenem concluded that it provides a higher bacterial response and lower adverse event rates than imipenem in people with severe infections, but no difference in mortality rate.[25]
- Ertapenem is administered once daily as an intravenous infusion or intramuscular injection. It lacks useful activity against the P. aeruginosa and Acinetobacter species, both of which are important causes of hospital-acquired infections.[26]
- Doripenem has a spectrum of activity very similar to that of meropenem. Its greater stability in solution allows the use of prolonged infusions and it is somewhat less likely to produce seizures than other carbapenems.[27]
- Panipenem/betamipron (Japanese approval 1993)
- Biapenem (Japanese approval 2001) exhibits similar efficacy and adverse event rates as other carbapenems.[28]
- Tebipenem (Japanese approval 2015) is the first carbapenem whose prodrug form, the pivalyl ester, is orally available.[29]
Unapproved/experimental
- Razupenem (PZ-601)
- PZ-601 is a carbapenem antibiotic currently being tested as having a broad spectrum of activity including strains resistant to other carbapenems. Despite early Phase II promise, Novartis (who acquired PZ-601 in a merger deal with Protez Pharmaceuticals) recently dropped PZ-601, citing a high rate of adverse events in testing.[30]
- Lenapenem
- Sulopenem is in clinical trials for drug resistant urinary tract infections
- Tomopenem
- Thienamycin (thienpenem) the first discovered carbapenem
Bacterial resistance
Enterobacteriaceae
Enterobacteriaceae are common pathogens responsible for urinary tract infections,[31][32] abdominal infections,[33] and hospital-acquired pneumonia.[9] Beta lactam resistance in these pathogens is most commonly due to the expression of beta lactamase enzymes.[34]
Between 2007 and 2011, the percentage of Escherichia coli isolates from Canadian hospitals that produce extended spectrum beta lactamases (ESBL) increased from 3.4% to 4.1%; among Klebsiella pneumoniae isolates ESBL producers increased from 1.5% to 4.0%. These strains are resistant to third generation cephalosporins that were developed for the treatment of beta lactamase-producing Enterobacteriaceae and carbapenems are generally regarded as the treatment of choice.[35] More recently, many countries have experienced a dramatic upswing in the prevalence of Enterobacteriaceae that produce both ESBLs and carbapenemases such as the Klebsiella pneumoniae carbapenemase (KPC). As of 2013, 70% of Greek Klebsiella pneumoniae isolates are resistant to third generation cephalosporins and 60% are resistant to carbapenems.[36] The growing prevalence and difficulty of treating such multi-drug resistant Enterobacteriaceae has led to a renaissance of the use of antibiotics such as colistin, which was discovered in the 1950s but rarely used until recently due to unattractive levels of toxicity.[37]
Prevalence of carbapenem-resistant Enterobacteriaceae in paediatric intensive care units (Cairo, Egypt) was 24% and various genes of carbapenemases were detected in 80% of carbapenem-resistant Enterobacteriaceae with dominance of blaOXA-48.[38]
Pseudomonas aeruginosa and Acinetobacter baumannii
Infections caused by the non-fermenting gram-negative bacteria Pseudomonas aeruginosa and Acinetobacter baumanni are most commonly encountered in hospitalized people. These bacteria exhibit an unusually high level of intrinsic resistance to antibiotics due to their expression of a wide range of resistance mechanisms. Antibiotics cross the outer membrane of Pseudomonas and Acinetobacter approximately 100 times more slowly than they cross the outer membrane of Enterobacteriaceae, due in part to their use of porins that can adopt a conformation having a very restricted entry channel. Further, the porin levels may be down-regulated in response to antibiotic exposure. Antibiotic molecules that successfully traverse the porin channels may be removed by efflux pumps. Downregulation of the porin OprD2 is an important contributor to imipenem resistance.[39]
Like the Enterobacteriaceae, Pseudomonas and Acinetobacter can express a wide range of antibiotic-deactivitating enzymes, including beta lactamases. Pseudomonas produces an inducible broad spectrum beta lactamase, AmpC, that is produced in response to beta lactam exposure. The combination of inducible AmpC expression, poor membrane permeability, and efflux pumps make Pseudomonas resistant to most beta lactams. The clinical efficacy of carbapenems in Pseudomonas infection arises in part because, while they are strong inducers of AmpC, they are poor substrates. The identification of Pseudomonas strains that produce beta lactamases capable of cleaving carbapenems, such as the New Delhi metallo beta lactamase has raised increasing concern regarding the potential for an era of untreatable Pseudomonas infections.[40]
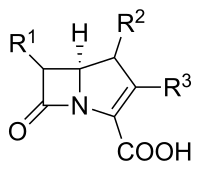
Structure
In terms of structure, the carbapenems are very similar to the penicillins (penams), but the sulfur atom in position 1 of the structure has been replaced with a carbon atom, and an unsaturation has been introduced—hence the name of the group, the carbapenems.
Groups
Carbapenems are further broken down into groups with ertapenem being the lone member of group 1. Group 2 carbapenems (imipenem, meropenem, and doripenem) are identified by their efficacy with respect to multiresistant gram-negative (MDRGN) bacteria such as Pseudomonas and Acinetobacter species. [41]
Biosynthesis
The carbapenems are thought to share their early biosynthetic steps in which the core ring system is formed. Malonyl-CoA is condensed with glutamate-5-semialdehyde with concurrent formation of the five-membered ring. Next, a β-lactam synthetase uses ATP to form the β-lactam and the saturated carbapenam core. Further oxidation and ring inversion provides the basic carbapenem .
Administration
Due to their expanded spectra, the desire to avoid generation of resistance and the fact that, in general, they have poor oral bioavailability, they are administered intravenously in hospital settings for more serious infections. However, research is underway to develop an effective oral carbapenem.[42]
See also
- Faropenem is closely related, but it is a penem, not a carbapenem.[43]
- Antimicrobial resistance
- NDM-1 is an enzyme that introduces bacterial resistance to carbapenem antibiotics via hydrolysis of the carbapenem backbone, thereby inactivating its ability to inhibit cell wall synthesis.
References
- Sneader, Walter (2006). Drug Discovery-A History. Wiley. p. 310. ISBN 978-0-471-89980-8.
- Birnbaum J, Kahan FM, Kropp H, MacDonald JS (June 1985). "Carbapenems, a new class of beta-lactam antibiotics. Discovery and development of imipenem/cilastatin". American Journal of Medicine. 78 (6A): 3–21. doi:10.1016/0002-9343(85)90097-X. ISSN 0002-9343. PMID 3859213.
- "Brazil: Klebsiella pneumoniae carbapenemase prompts closing of hospital ICU - Outbreak News Today". 2015-07-26.
- Breilh D, Texier-Maugein J, Allaouchiche B, Saux MC, Boselli E (2013). "Carbapenems". J Chemother. 25 (1): 1–17. doi:10.1179/1973947812Y.0000000032. PMID 23433439. S2CID 218660238.
- Papp-Wallace KM, Endimiani A, Taracila MA, Bonomo RA (2011). "Carbapenems: past, present, and future". Antimicrob. Agents Chemother. 55 (11): 4943–60. doi:10.1128/AAC.00296-11. PMC 3195018. PMID 21859938.
- Livermore DM, Woodford N (October 2000). "Carbapenemases: a problem in waiting?". Current Opinion in Microbiology. 3 (5): 489–95. doi:10.1016/S1369-5274(00)00128-4. ISSN 1369-5274. PMID 11050448.
- Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O'Neill PJ, Chow AW, Dellinger EP, Eachempati SR, Gorbach S, Hilfiker M, May AK, Nathens AB, Sawyer RG, Bartlett JG (2010). "Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America". Clin. Infect. Dis. 50 (2): 133–64. doi:10.1086/649554. PMID 20034345.
- Golan Y (2015). "Empiric therapy for hospital-acquired, gram-negative complicated intra-abdominal infection and complicated urinary tract infections: a systematic literature review of current and emerging treatment options". BMC Infect. Dis. 15: 313. doi:10.1186/s12879-015-1054-1. PMC 4526420. PMID 26243291.
- Infectious Diseases Society of America (2005). "Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia". Am. J. Respir. Crit. Care Med. 171 (4): 388–416. doi:10.1164/rccm.200405-644ST. PMID 15699079.
- Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Read R, Verheij TJ (2011). "Guidelines for the management of adult lower respiratory tract infections--full version". Clin. Microbiol. Infect. 17 (Suppl 6): E1–59. doi:10.1111/j.1469-0691.2011.03672.x. PMC 7128977. PMID 21951385.
- Shiber S, Yahav D, Avni T, Leibovici L, Paul M (2015). "β-Lactam/β-lactamase inhibitors versus carbapenems for the treatment of sepsis: systematic review and meta-analysis of randomized controlled trials". J. Antimicrob. Chemother. 70 (1): 41–7. doi:10.1093/jac/dku351. PMID 25261419.
- National Collaborating Centre for Cancer (UK) (2012). Neutropenic Sepsis: Prevention and Management of Neutropenic Sepsis in Cancer Patients - National Library of Medicine - PubMed Health. National Institute for Health and Care Excellence: Guidance. National Institute for Health and Clinical Excellence (UK). PMID 26065059.
- Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME (2012). "Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum β-lactamases: a systematic review and meta-analysis". J. Antimicrob. Chemother. 67 (12): 2793–803. doi:10.1093/jac/dks301. PMID 22915465.
- "www.accessdata.fda.gov" (PDF).
- "www.accessdata.fda.gov" (PDF).M
- Herrero, Miranda (2015). "Pharmacological interaction between valproic acid and carbapenem: what about levels in pediatrics?". European Journal of Paediatric Neurology. 19 (2): 155–61. doi:10.1016/j.ejpn.2014.12.010. PMID 25578527.
- Torres MJ, Blanca M (2010). "The complex clinical picture of beta-lactam hypersensitivity: penicillins, cephalosporins, monobactams, carbapenems, and clavams". Med. Clin. North Am. 94 (4): 805–20, xii. doi:10.1016/j.mcna.2010.04.006. PMID 20609864.
- Slama TG (2008). "Clinical review: balancing the therapeutic, safety, and economic issues underlying effective antipseudomonal carbapenem use". Crit Care. 12 (5): 233. doi:10.1186/cc6994. PMC 2592734. PMID 18983709.
- Slimings C, Riley TV (2014). "Antibiotics and hospital-acquired Clostridium difficile infection: update of systematic review and meta-analysis". J. Antimicrob. Chemother. 69 (4): 881–91. doi:10.1093/jac/dkt477. PMID 24324224.
- "Pharmaceutical Sciences CSU Parenteral Antibiotic Allergy cross-sensitivity chart" (PDF). Vancouver Acute Pharmaceutical Sciences, Vancouver Hospital & Health Sciences Centre. 2016. Archived from the original (PDF) on April 17, 2016. Retrieved May 19, 2017.
- PRIMAXIN (Brand Name Drug) FDA Application No. (NDA) 050587 Drug Details, Drugs@FDA
- "www.accessdata.fda.gov" (PDF).
- "www.accessdata.fda.gov" (PDF).
- Zhanel GG, Simor AE, Vercaigne L, Mandell L (1998). "Imipenem and meropenem: Comparison of in vitro activity, pharmacokinetics, clinical trials and adverse effects". Can J Infect Dis. 9 (4): 215–28. doi:10.1155/1998/831425. PMC 3250889. PMID 22346545.
- Edwards SJ, Emmas CE, Campbell HE (2005). "Systematic review comparing meropenem with imipenem plus cilastatin in the treatment of severe infections". Curr Med Res Opin. 21 (5): 785–94. doi:10.1185/030079905X46223. PMID 15969878. S2CID 7654496.
- "www.accessdata.fda.gov" (PDF).
- Chahine EB, Ferrill MJ, Poulakos MN (2010). "Doripenem: a new carbapenem antibiotic". Am J Health Syst Pharm. 67 (23): 2015–24. doi:10.2146/ajhp090672. PMID 21098373.
- Pei G, Yin W, Zhang Y, Wang T, Mao Y, Sun Y (2014). "Efficacy and safety of biapenem in treatment of infectious disease: a meta-analysis of randomized controlled trials". J Chemother. 28 (1): 28–36. doi:10.1179/1973947814Y.0000000226. PMID 25407221. S2CID 36170846.
- Hazra, Saugata; Xu, Hua; Blanchard, John (Jun 2014). "Tebipenem, a New Carbapenem Antibiotic is a Slow Substrate that Inhibits the β-Lactamase from Mycobacterium tuberculosis". Biochemistry. 53 (22): 3671–8. doi:10.1021/bi500339j. PMC 4053071. PMID 24846409.
- George, John (21 September 2010). "Novartis shutters Protez". BioValley.
- Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE (2011). "International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases". Clin. Infect. Dis. 52 (5): e103–20. doi:10.1093/cid/ciq257. PMID 21292654.
- Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, Saint S, Schaeffer AJ, Tambayh PA, Tenke P, Nicolle LE (2010). "Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America". Clin. Infect. Dis. 50 (5): 625–63. doi:10.1086/650482. PMID 20175247.
- Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O'Neill PJ, Chow AW, Dellinger EP, Eachempati SR, Gorbach S, Hilfiker M, May AK, Nathens AB, Sawyer RG, Bartlett JG (2010). "Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America". Surg Infect (Larchmt). 11 (1): 79–109. doi:10.1089/sur.2009.9930. PMID 20163262.
- Delgado-Valverde M, Sojo-Dorado J, Pascual A, Rodríguez-Baño J (2013). "Clinical management of infections caused by multidrug-resistant Enterobacteriaceae". Ther Adv Infect Dis. 1 (2): 49–69. doi:10.1177/2049936113476284. PMC 4040721. PMID 25165544.
- Denisuik AJ, Lagacé-Wiens PR, Pitout JD, Mulvey MR, Simner PJ, Tailor F, Karlowsky JA, Hoban DJ, Adam HJ, Zhanel GG (2013). "Molecular epidemiology of extended-spectrum β-lactamase-, AmpC β-lactamase- and carbapenemase-producing Escherichia coli and Klebsiella pneumoniae isolated from Canadian hospitals over a 5 year period: CANWARD 2007-11". J. Antimicrob. Chemother. 68 (Suppl 1): i57–65. doi:10.1093/jac/dkt027. PMID 23587779.
- "Antimicrobial Resistance in Europe 2013" (PDF). ecdc.europa.eu. European Centre for Disease Prevention and Control. 2013. p. 21. Retrieved 7 April 2022.
- Giske CG (2015). "Contemporary resistance trends and mechanisms for the old antibiotics colistin, temocillin, fosfomycin, mecillinam and nitrofurantoin". Clin. Microbiol. Infect. 21 (10): 899–905. doi:10.1016/j.cmi.2015.05.022. PMID 26027916.
- Ghaith, Doaa M.; Mohamed, Zeinat K.; Farahat, Mohamed G.; Aboulkasem Shahin, Walaa; Mohamed, Hadeel O. (2019-03-01). "Colonization of intestinal microbiota with carbapenemase-producing Enterobacteriaceae in paediatric intensive care units in Cairo, Egypt". Arab Journal of Gastroenterology. 20 (1): 19–22. doi:10.1016/j.ajg.2019.01.002. ISSN 1687-1979. PMID 30733176. S2CID 73444389.
- Rice LB (2006). "Challenges in identifying new antimicrobial agents effective for treating infections with Acinetobacter baumannii and Pseudomonas aeruginosa". Clin. Infect. Dis. 43 (Suppl 2): S100–5. doi:10.1086/504487. PMID 16894511.
- Morita Y, Tomida J, Kawamura Y (2014). "Responses of Pseudomonas aeruginosa to antimicrobials". Front Microbiol. 4: 422. doi:10.3389/fmicb.2013.00422. PMC 3884212. PMID 24409175.
- {{Yoon YK, Yang KS, Lee SE, Kim HJ, Sohn JW, Kim MJ. Effects of Group 1 versus Group 2 carbapenems on the susceptibility of Acinetobacter baumannii to carbapenems: a before and after intervention study of carbapenem-use stewardship. PLoS One. 2014;9(6):e99101. Published 2014 Jun 9. doi:10.1371/journal.pone.0099101}}
- Kumagai T, Tamai S, Abe T, Hikda M (January 2002). "Current status of oral carbapenem development". Current Medicinal Chemistry. 1 (1): 1–14. doi:10.2174/1568012023355018. ISSN 1568-0126.
- Hamilton-Miller, JM (November 2003). "Chemical and Microbiologic Aspects of Penems, a Distinct Class of β-Lactams: Focus on Faropenem". Pharmacotherapy. 23 (11): 1497–507. doi:10.1592/phco.23.14.1497.31937. PMID 14620395. S2CID 43705118.
External links
- Structure Activity Relationships "Antibacterial Agents; Structure Activity Relationships," André Bryskier MD; beginning at pp131
- Page 2: Ertapenem vs. Meropenem: Equivalency of Clinical and Microbiological Outcomes. 2010