Cervical artery dissection
Cervical artery dissection is dissection of one of the layers that compose the carotid and vertebral artery in the neck (cervix).[1][2] They include:[1]
- Carotid artery dissection, a separation of the layers of the artery wall supplying oxygen-bearing blood to the head and brain.[3]
- Vertebral artery dissection, a flap-like tear of the inner lining of the vertebral artery that supply blood to the brain and spinal cord.[4]
| Cervical artery dissection | |
|---|---|
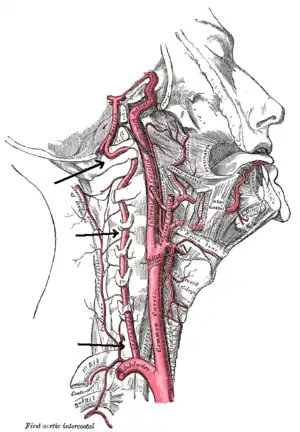 | |
| Arteries of the neck. | |
| Types | Carotid artery dissection, vertebral artery dissection[1] |
Cervical dissections can be broadly classified as either "spontaneous" or traumatic. Cervical artery dissections are a significant cause of strokes in young adults.[5]
A dissection typically results in a tear in one of the layers of the arterial wall.[2] The result of this tear is often an intramural hematoma and/or aneurysmal dilation[2][6] in the arteries leading to the intracranial area.[2][7]
Signs and symptoms of a cervical artery dissection are often non-specific and can be localized or generalized.[1][2] There is no specific treatment, although most patients are either given an anti-platelet or anti-coagulation agent to prevent or treat strokes.[2]
Epidemiology
Cervical artery dissection has been noted to be a common cause of young adult strokes, with some sources indicating a prevalence of up to 20% in this young adult population with annual incidence rates between 2.6 and 2.9 per 100,000, although these incidences may be misleading with true incidences being higher because clinical presentations can vary, many being minor or self-limited, and thus these dissections can go undiagnosed.[5] In population-based studies, the peak age of presentation is approximately 45 years with a slight gender predisposition towards males (53-57%).[8][9]
Cervical arteries, as mentioned above, consist of two pairs of arteries: vertebral and carotid. As such, cervical artery dissection can be further categorized based on the involvement of artery: carotid vs. vertebral, and the location of the dissection: intracranial vs. extracranial.[10][11]
Causes
The two main causes of cervical artery dissection can be broadly categorized as either spontaneous or traumatic.[2] Arterial walls are composed of three layers: an intima (the innermost layer), media (the middle muscular layer), and adventitia (the outermost layer).[12] A tear in one of the layers of the arterial walls can result in blood collecting within a pocket between the layers of the artery, which can result in an intramural hematoma and/or aneurysmal dilation.[2][6][10] At the moment, there is no definitive location for the dissection, with some believing dissection initially occurs within the connective tissue and vasa vasorum of the media while others believe dissection begins with an intimal tear.[10][13]
Spontaneous
Spontaneous cervical artery dissections are dissections that occur without any trauma to the neck.[2] More specifically, this can include potential causes such as hereditary connective tissue diseases, family history of strokes, infections and other miscellaneous causes such as smoking, hypertension, migraines and contraceptive use.[10][14] Hereditary connective tissue diseases include autosomal polycystic kidney disease, Ehlers-Danlos syndrome, Marfan syndrome, fibromuscular dysplasia, and osteogenesis imperfecta type 1 although studies have shown that the link between hereditary connective tissue diseases and cervical artery dissection is low, ranging from 0-0.6% in one study and 5-18% in another study.[15]
Traumatic
Traumatic cervical artery dissections are dissections that occur after any sort of trauma to the neck, ranging from minor trauma such as nose-blowing or sneezing to severe trauma such as roadside accidents.[2][10] Most traumatic dissections are secondary to some form of rapid decelerations injuries resulting in hyperextension or hyperflexion with rotational injury of the neck.[6]
Pathophysiology
Cervical artery dissections begin initially with a small tear in the innermost layer of the arterial wall, the tunica intima, or rupture of the vasa vasorum with bleeding within the media. As the arterial wall begins to tear, blood begins to enter this newly formed false lumen and the resulting hematoma formation can either narrow (stenosis) or occlude the artery, decreasing or completely blocking blood flow through the artery. A complete occlusion of the artery can result in cerebral ischemia as the brain is depleted of oxygen-rich blood.[16] Because the brain has a pair of carotid and vertebral arteries on each side of the neck, a unilateral occlusion can be asymptomatic, as the bilateral circulation continues perfusing the brain.[17] Thrombus formation is the natural physiologic response to the vascular injury to prevent significant blood loss.[18] However, parts of the thrombus can break apart and result in emboli that can lodge themselves in distal cerebral arteries causing ischemic stroke, otherwise known as a cerebral infarction.[19][20]
Signs and symptoms
The signs and symptoms of cervical artery dissection are often non-specific or generalized and can either develop acutely or over several days.
Imaging
Various imaging modalities can be used for the diagnosis of cervical artery dissection. The diagnosis of cervical artery dissection can be confirmed with the presence of a mural hematoma on ultrasound (US) or magnetic resonance imaging (MRI) and will also guide therapeutic decision making.[7] MRI, with a fat-suppressed T1 sequence, is often first-line imaging.[7] However, other modalities exist with helical computed topographic angiography (CTA) becoming the new gold-standard. Magnetic resonance angiography (MRA) and doppler US can also be utilized as additional non-invasive imaging techniques.[2] The purpose of these imaging techniques is often multi-functional. These imaging modalities can detect the direction and changes of blood flow within the arteries and whether the dissection has resulted in any damage to brain tissue.[2][7]
Treatment
The primary goal of treatment in cervical artery dissection is preventing or treating a stroke. Treatment guidelines also depend on the presence of underlying connective tissue disorders, dissection secondary to trauma, and underlying medical conditions. Management is often using either antiplatelet agents (i.e. aspirin) or anti-coagulation to prevent development of thrombus. Antiplatelet drugs can be given as individual drugs, or in combination (i.e. aspirin alone, or aspiring and clopidogrel). Anticoagulation such as heparin, intravenously (IV) or injectable (shot) can be given while inpatient and followed by heparin.[2] A recent trial in 2015, the Cervical Artery Dissection in Stroke Study (CADISS), examined the efficacy of antiplatelet and anticoagulation treatment with the primary endpoint of ipsilateral stroke or death in individuals with symptomatic dissections. The CADISS trial revealed no significant difference in efficacy of antiplatelet and anticoagulant drugs in preventing strokes or death, but did note that strokes were rare in either group, and rarer than what has been reported in observational studies.[21]
References
- "When a pain in the neck is serious". Harvard Health. Harvard Publishing. August 2017. Retrieved 8 January 2020.
- "Cervical (Carotid or Vertebral) Artery Dissection". Cleveland Clinic. 2019-05-24. Archived from the original on 2019-11-29. Retrieved 2021-11-03.
- Jasmin L. "Carotid Dissection". Cedars-Sinai. Archived from the original on 2019-09-02. Retrieved 2021-11-03.
- "Vertebral Artery: What Is It, Location, Anatomy and Function". Cleveland Clinic. 2021-07-23. Archived from the original on 2021-11-06. Retrieved 2021-11-03.
- Lee VH, Brown RD, Mandrekar JN, Mokri B (November 2006). "Incidence and outcome of cervical artery dissection: a population-based study". Neurology. 67 (10): 1809–1812. doi:10.1212/01.wnl.0000244486.30455.71. PMID 17130413. S2CID 72123054.
- Chaibi A, Russell MB (March 2019). "A risk-benefit assessment strategy to exclude cervical artery dissection in spinal manual-therapy: a comprehensive review". Annals of Medicine. 51 (2): 118–127. doi:10.1080/07853890.2019.1590627. PMC 7857472. PMID 30889367.
- Ben Hassen W, Machet A, Edjlali-Goujon M, Legrand L, Ladoux A, Mellerio C, et al. (December 2014). "Imaging of cervical artery dissection". Diagnostic and Interventional Imaging. FMC: Cerebrovascular diseases. 95 (12): 1151–1161. doi:10.1016/j.diii.2014.10.003. PMID 25632417.
- Arnold M, Kappeler L, Georgiadis D, Berthet K, Keserue B, Bousser MG, Baumgartner RW (September 2006). "Gender differences in spontaneous cervical artery dissection". Neurology. 67 (6): 1050–1052. doi:10.1212/01.wnl.0000237341.30854.6a. PMID 17000975. S2CID 12969343.
- Touzé E, Gauvrit JY, Moulin T, Meder JF, Bracard S, Mas JL (November 2003). "Risk of stroke and recurrent dissection after a cervical artery dissection: a multicenter study". Neurology. 61 (10): 1347–1351. doi:10.1212/01.wnl.0000094325.95097.86. PMID 14638953. S2CID 9715826.
- Thanvi B, Munshi SK, Dawson SL, Robinson TG (June 2005). "Carotid and vertebral artery dissection syndromes". Postgraduate Medical Journal. 81 (956): 383–388. doi:10.1136/pgmj.2003.016774. PMC 1743284. PMID 15937204.
- Kwon JY, Kim NY, Suh DC, Kang DW, Kwon SU, Kim JS (November 2015). "Intracranial and extracranial arterial dissection presenting with ischemic stroke: Lesion location and stroke mechanism". Journal of the Neurological Sciences. 358 (1–2): 371–376. doi:10.1016/j.jns.2015.09.368. PMID 26434614. S2CID 206289781.
- Tucker WD, Arora Y, Mahajan K (2021). "Anatomy, Blood Vessels". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29262226. Retrieved 2021-11-03.
- Schievink WI (March 2001). "Spontaneous dissection of the carotid and vertebral arteries". The New England Journal of Medicine. 344 (12): 898–906. doi:10.1056/NEJM200103223441206. PMID 11259724.
- Campos-Herrera CR, Scaff M, Yamamoto FI, Conforto AB (December 2008). "Spontaneous cervical artery dissection: an update on clinical and diagnostic aspects". Arquivos de Neuro-Psiquiatria. 66 (4): 922–927. doi:10.1590/s0004-282x2008000600036. PMID 19099146.
- de Bray JM, Baumgartner RW (July 2005). "History of spontaneous dissection of the cervical carotid artery". Archives of Neurology. 62 (7): 1168–1170. doi:10.1001/archneur.62.7.1168. PMID 16009782.
- DeSai C, Hays Shapshak A (2021). "Cerebral Ischemia". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32809345. Retrieved 2021-11-05.
- Liebeskind DS (September 2003). "Collateral circulation". Stroke. 34 (9): 2279–2284. doi:10.1161/01.STR.0000086465.41263.06. PMID 12881609.
- Yazdani A, Li H, Bersi MR, Di Achille P, Insley J, Humphrey JD, Karniadakis GE (February 2018). "Data-driven Modeling of Hemodynamics and its Role on Thrombus Size and Shape in Aortic Dissections". Scientific Reports. 8 (1): 2515. Bibcode:2018NatSR...8.2515Y. doi:10.1038/s41598-018-20603-x. PMC 5802786. PMID 29410467.
- Ibrahim F, Murr N (2021). "Embolic Stroke". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 33232021. Retrieved 2021-11-05.
- Lucas C, Moulin T, Deplanque D, Tatu L, Chavot D (December 1998). "Stroke patterns of internal carotid artery dissection in 40 patients". Stroke. 29 (12): 2646–2648. doi:10.1161/01.STR.29.12.2646. PMID 9836779. S2CID 9500008.
- Markus HS, Hayter E, Levi C, Feldman A, Venables G, Norris J (April 2015). "Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial". The Lancet. Neurology. 14 (4): 361–367. doi:10.1016/S1474-4422(15)70018-9. hdl:2440/102964. PMID 25684164. S2CID 6985697.