Cryopyrin-associated periodic syndrome
Cryopyrin-associated periodic syndrome (CAPS) is a group of rare, heterogeneous autoinflammatory disease characterized by interleukin 1β-mediated systemic inflammation and clinical symptoms involving skin, joints, central nervous system, and eyes. It encompasses a spectrum of three clinically overlapping autoinflammatory syndromes including familial cold autoinflammatory syndrome (FCAS, formerly termed familial cold-induced urticaria), the Muckle–Wells syndrome (MWS), and neonatal-onset multisystem inflammatory disease (NOMID, also called chronic infantile neurologic cutaneous and articular syndrome or CINCA) that were originally thought to be distinct entities, but in fact share a single genetic mutation and pathogenic pathway, and keratoendotheliitis fugax hereditaria in which the autoinflammatory symptoms affect only the anterior segment of the eye.
| Cryopyrin-associated periodic syndrome | |
|---|---|
| Other names | CAPS[1] |
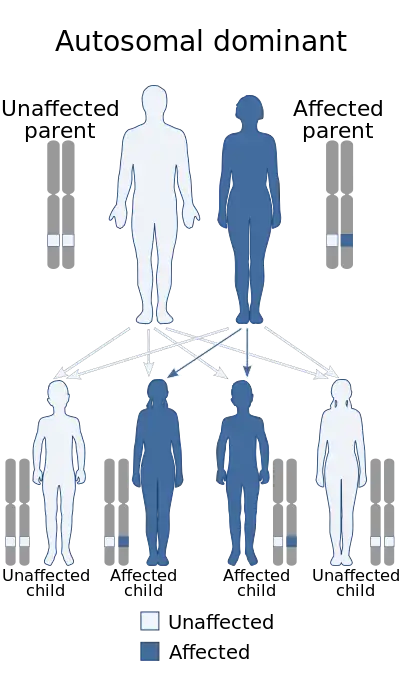 | |
| Cryopyrin-associated periodic syndrome is autosomal dominant in inheritance | |
| Specialty | Dermatology, medical genetics |
Signs and symptoms
The syndromes within CAPS overlap clinically, and patients may have features of more than one disorder. In a retrospective cohort of 136 CAPS patients with systemic involvement from 16 countries,[2] the most prevalent clinical features were fever (84% of cases, often with concurrent constitutional symptoms such as fatigue, malaise, mood disorders or failure to thrive), skin rash (either urticarial or maculopapular rash; 97% of cases) especially after cold exposure, and musculoskeletal involvement (myalgia, arthralgia, and/or arthritis, or less commonly joint contracture, patellar overgrowth, bone deformity, bone erosion and/or osteolytic lesion; 86% of cases). Less common features included ophthalmological involvement (conjunctivitis and/or uveitis, or less commonly optic nerve atrophy, cataract, glaucoma or impaired vision; 71% of cases), neurosensory hearing loss (42% of cases), neurological involvement (morning headache, papilloedema, and/or meningitis, or less commonly seizure, hydrocephalus or intellectual disability; 40% of cases), and AA amyloidosis (4% of cases).
In keratoendotheliitis fugax hereditaria, systemic symptoms are not reported whereas the patients experience periodical transient inflammation of the corneal endothelium and stroma, leading to short term blurring of vision and, after repeated attacks, to central corneal stromal opacities in some patients.[3]
Age of onset is typically in infancy or early childhood. In 57% of cases, CAPS had a chronic phenotype with symptoms present almost daily, whereas the remaining 43% of patients experienced only acute episodes. Up to 56% of patients reported a family history of CAPS. Previous studies confirm these symptoms, although the exact reported rates vary.[4][5]
Pathogenesis
Cryopyrin-associated periodic syndromes are associated with a gain-of-function missense mutation in exon 3 of NLRP3, the gene encoding cryopyrin, a major component of the interleukin 1 inflammasome.[2][6] In keratoendotheliitis fugax hereditaria, the mutation occurs in exon 1.[3] Intracellular formation of the interleukin 1 inflammasome leads to the activation of the potent pro-inflammatory cytokines interleukin 1β and interleukin-18 through a cascade involving caspase 1. The IL-1 inflammasome may also be released from activated macrophages, amplifying the cytokine production cascade.[7] The mutation in NLRP3 leads to aberrant formation of this inflammasome and subsequent unregulated production of interleukin 1β.
Up to 170 heterogenous mutations in NLRP3 have been identified. Some reports suggest rare mutations are more frequently associated with a severe phenotype,[8] and some mutations are associated with distinct phenotypes, probably reflecting the differential impact of the mutation on the activity of the inflammasome in the context of individual genetic background.[2][3] Inheritance of these disorders is autosomal dominant with variable penetrance.
Diagnosis
Because CAPS is extremely rare and has a broad clinical presentation, it is difficult to diagnose, and a significant delay exists between symptom onset and definitive diagnosis.[9] There are currently no clinical or diagnostic criteria for CAPS based solely on clinical presentation. Instead, diagnosis is made by genetic testing for NLRP3 mutations. Acute phase reactants and white blood cell count are usually persistently elevated, but this is aspecific for CAPS.
Treatment
Since interleukin 1β plays a central role in the pathogenesis of the disease, therapy typically targets this cytokine in the form of monoclonal antibodies (such as canakinumab[10][11]), binding proteins/traps (such as rilonacept[12]), or interleukin 1 receptor antagonists (such as anakinra[13][14][15][16]). These therapies are generally effective in alleviating symptoms and substantially reducing levels of inflammatory indices. Case reports suggest that thalidomide[17] and the anti-IL-6 receptor antibody tocilizumab[18] may also be effective.
References
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Cryopyrin associated periodic syndrome". www.orpha.net. Retrieved 27 April 2019.
- Levy, R.; Gérard, L.; Kuemmerle-Deschner, J.; Lachmann, H. J.; Koné-Paut, I.; Cantarini, L.; Woo, P.; Naselli, A.; Bader-Meunier, B. (2015-11-01). "Phenotypic and genotypic characteristics of cryopyrin-associated periodic syndrome: a series of 136 patients from the Eurofever Registry". Annals of the Rheumatic Diseases. 74 (11): 2043–2049. doi:10.1136/annrheumdis-2013-204991. hdl:11365/976415. ISSN 1468-2060. PMID 25038238. S2CID 206850668.
- Turunen JA, Wedenoja J, Repo P, Järvinen RS, Jäntti JE, Mörtenhumer S, Riikonen AS, Lehesjoki AE, Majander A, Kivelä TT (Jan 2018). "Keratoendotheliitis Fugax Hereditaria: A Novel Cryopyrin-Associated Periodic Syndrome Caused by a Mutation in the Nucleotide-Binding Domain, Leucine-Rich Repeat Family, Pyrin Domain-Containing 3 (NLRP3) Gene". American Journal of Ophthalmology. 184: 41–50. doi:10.1016/j.ajo.2018.01.017. PMID 29366613.
- Cuisset, L.; Drenth, J. P.; Berthelot, J. M.; Meyrier, A.; Vaudour, G.; Watts, R. A.; Scott, D. G.; Nicholls, A.; Pavek, S. (1999-10-01). "Genetic linkage of the Muckle-Wells syndrome to chromosome 1q44". American Journal of Human Genetics. 65 (4): 1054–1059. doi:10.1086/302589. ISSN 0002-9297. PMC 1288238. PMID 10486324.
- Darisipudi, Murthy Narayana; Thomasova, Dana; Mulay, Shrikant R.; Brech, Dorothee; Noessner, Elfriede; Liapis, Helen; Anders, Hans-Joachim (2016-10-21). "Uromodulin Triggers IL-1β–Dependent Innate Immunity via the NLRP3 Inflammasome". Journal of the American Society of Nephrology. 23 (11): 1783–1789. doi:10.1681/ASN.2012040338. ISSN 1046-6673. PMC 3482735. PMID 22997256.
- Hoffman, H. M.; Mueller, J. L.; Broide, D. H.; Wanderer, A. A.; Kolodner, R. D. (2001-11-01). "Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome". Nature Genetics. 29 (3): 301–305. doi:10.1038/ng756. ISSN 1061-4036. PMC 4322000. PMID 11687797.
- Neven, Bénédicte; Prieur, Anne-Marie; Quartier dit Maire, Pierre (2008-09-01). "Cryopyrinopathies: update on pathogenesis and treatment". Nature Clinical Practice Rheumatology. 4 (9): 481–489. doi:10.1038/ncprheum0874. ISSN 1745-8390. PMID 18665151. S2CID 13022253.
- "Infevers". fmf.igh.cnrs.fr. Archived from the original on 2016-10-21. Retrieved 2016-10-21.
- Toplak, Natasa; Frenkel, Joost; Ozen, Seza; Lachmann, Helen J.; Woo, Patricia; Koné-Paut, Isabelle; De Benedetti, Fabrizio; Neven, Benedicte; Hofer, Michael (2012-07-01). "An international registry on autoinflammatory diseases: the Eurofever experience". Annals of the Rheumatic Diseases. 71 (7): 1177–1182. doi:10.1136/annrheumdis-2011-200549. ISSN 1468-2060. PMID 22377804. S2CID 6670512.
- Lachmann, Helen J.; Kone-Paut, Isabelle; Kuemmerle-Deschner, Jasmin B.; Leslie, Kieron S.; Hachulla, Eric; Quartier, Pierre; Gitton, Xavier; Widmer, Albert; Patel, Neha (2009-06-04). "Use of canakinumab in the cryopyrin-associated periodic syndrome". The New England Journal of Medicine. 360 (23): 2416–2425. doi:10.1056/NEJMoa0810787. ISSN 1533-4406. PMID 19494217. S2CID 28667263.
- Sibley, Cailin H.; Chioato, Andrea; Felix, Sandra; Colin, Laurence; Chakraborty, Abhijit; Plass, Nikki; Rodriguez-Smith, Jackeline; Brewer, Carmen; King, Kelly (2015-09-01). "A 24-month open-label study of canakinumab in neonatal-onset multisystem inflammatory disease". Annals of the Rheumatic Diseases. 74 (9): 1714–1719. doi:10.1136/annrheumdis-2013-204877. ISSN 1468-2060. PMC 4258169. PMID 24906637.
- Hoffman, Hal M.; Throne, Martin L.; Amar, N. J.; Sebai, Mohamed; Kivitz, Alan J.; Kavanaugh, Arthur; Weinstein, Steven P.; Belomestnov, Pavel; Yancopoulos, George D. (2008-08-01). "Efficacy and safety of rilonacept (interleukin-1 Trap) in patients with cryopyrin-associated periodic syndromes: results from two sequential placebo-controlled studies". Arthritis and Rheumatism. 58 (8): 2443–2452. doi:10.1002/art.23687. ISSN 0004-3591. PMID 18668535.
- Ross, J. Barrie; Finlayson, Laura A.; Klotz, P. Jennifer; Langley, Richard G.; Gaudet, Roxanne; Thompson, Kara; Churchman, Sarah M.; McDermott, Michael F.; Hawkins, Philip N. (2017-02-01). "Use of anakinra (Kineret) in the treatment of familial cold autoinflammatory syndrome with a 16-month follow-up". Journal of Cutaneous Medicine and Surgery. 12 (1): 8–16. doi:10.2310/7750.2008.07050. ISSN 1203-4754. PMID 18258152. S2CID 34516905.
- Hoffman, Hal M.; Rosengren, Sanna; Boyle, David L.; Cho, Jae Y.; Nayar, Jyothi; Mueller, James L.; Anderson, Justin P.; Wanderer, Alan A.; Firestein, Gary S. (2016-11-13). "Prevention of cold-associated acute inflammation in familial cold autoinflammatory syndrome by interleukin-1 receptor antagonist". Lancet. 364 (9447): 1779–1785. doi:10.1016/S0140-6736(04)17401-1. ISSN 1474-547X. PMC 4321997. PMID 15541451.
- Goldbach-Mansky, Raphaela; Dailey, Natalie J.; Canna, Scott W.; Gelabert, Ana; Jones, Janet; Rubin, Benjamin I.; Kim, H. Jeffrey; Brewer, Carmen; Zalewski, Christopher (2006-08-10). "Neonatal-onset multisystem inflammatory disease responsive to interleukin-1beta inhibition". The New England Journal of Medicine. 355 (6): 581–592. doi:10.1056/NEJMoa055137. ISSN 1533-4406. PMC 4178954. PMID 16899778.
- Seitz, M.; Kamgang, R. K.; Simon, H. U.; Villiger, P. M. (2005-12-01). "Therapeutic interleukin (IL) 1 blockade normalises increased IL1 beta and decreased tumour necrosis factor alpha and IL10 production in blood mononuclear cells of a patient with CINCA syndrome". Annals of the Rheumatic Diseases. 64 (12): 1802–1803. doi:10.1136/ard.2005.036749. ISSN 0003-4967. PMC 1755296. PMID 16284353.
- Kallinich, T.; Hoffman, H. M.; Roth, J.; Keitzer, R. (2016-06-01). "The clinical course of a child with CINCA/NOMID syndrome improved during and after treatment with thalidomide". Scandinavian Journal of Rheumatology. 34 (3): 246–249. doi:10.1080/03009740410010236. ISSN 0300-9742. PMID 16134734. S2CID 30354429.
- Matsubara, Tomoyo; Hasegawa, Masanari; Shiraishi, Masahiro; Hoffman, Hal M.; Ichiyama, Takashi; Tanaka, Takeo; Ueda, Haruo; Ishihara, Tokuhiro; Furukawa, Susumu (2006-07-01). "A severe case of chronic infantile neurologic, cutaneous, articular syndrome treated with biologic agents". Arthritis and Rheumatism. 54 (7): 2314–2320. doi:10.1002/art.21965. ISSN 0004-3591. PMID 16802372.
- Kubota T, Koike R. Cryopyrin-associated periodic syndromes: background and therapeutics. Mod Rheumatol. 2010 Jun;20(3):213-21
- Autoinflammatory Alliance CAPS Guidebook