Depression (mood)
Depression is a mental state of low mood and aversion to activity.[3] It affects more than 280 million people of all ages (about 3.5% of the global population).[4] Depression affects a person's thoughts, behavior, feelings, and sense of well-being.[5] Depressed people often experience loss of motivation or interest in, or reduced pleasure or joy from, experiences that would normally bring them pleasure or joy.[6] Depressed mood is a symptom of some mood disorders such as major depressive disorder and dysthymia;[7] it is a normal temporary reaction to life events, such as the loss of a loved one; and it is also a symptom of some physical diseases and a side effect of some drugs and medical treatments. It may feature sadness, difficulty in thinking and concentration and a significant increase or decrease in appetite and time spent sleeping. People experiencing depression may have feelings of dejection or hopelessness and may experience suicidal thoughts. It can either be short term or long term.
| Depression | |
|---|---|
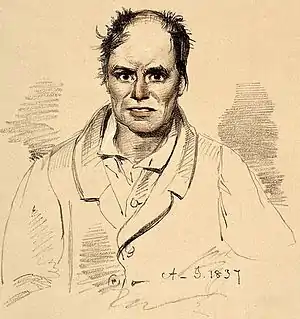 | |
| Lithograph of a person diagnosed with melancholia and strong suicidal tendency in 1892 | |
| Specialty | Psychiatry, psychology |
| Symptoms | Low mood, aversion to activity, loss of interest, loss of feeling pleasure |
| Causes | Brain chemistry, genetics, life events, medical conditions, personality[1] |
| Risk factors | Stigma of mental health disorder[2] |
| Diagnostic method | Patient Health Questionnaire, Beck Depression Inventory |
| Differential diagnosis | Anxiety, bipolar disorder, borderline personality disorder |
| Prevention | Social connections, physical activity |
| Treatment | Psychotherapy, psychopharmacology |
| Part of a series on |
| Emotions |
|---|
  |
Contributing factors

Life events
Adversity in childhood, such as bereavement, neglect, mental abuse, physical abuse, sexual abuse, or unequal parental treatment of siblings can contribute to depression in adulthood.[8][9] Childhood physical or sexual abuse in particular significantly correlates with the likelihood of experiencing depression over the survivor's lifetime.[10]
Life events and changes that may cause depressed mood include (but are not limited to): childbirth, menopause, financial difficulties, unemployment, stress (such as from work, education, military service, family, living conditions, marriage, etc.), a medical diagnosis (cancer, HIV, diabetes, etc.), bullying, loss of a loved one, natural disasters, social isolation, rape, relationship troubles, jealousy, separation, or catastrophic injury.[11][12][13][14][15] Adolescents may be especially prone to experiencing a depressed mood following social rejection, peer pressure, or bullying.[16]
Childhood and adolescence
Depression in childhood and adolescence is similar to adult major depressive disorder, although young sufferers may exhibit increased irritability or behavioral dyscontrol instead of the more common sad, empty, or hopeless feelings seen with adults.[17] Children who are under stress, experiencing loss, or have other underlying disorders are at a higher risk for depression. Childhood depression is often comorbid with mental disorders outside of other mood disorders; most commonly anxiety disorder and conduct disorder. Depression also tends to run in families.[18]
Personality
Depression is associated with low extraversion,[19] and people who have high levels of neuroticism are more likely to experience depressive symptoms and are more likely to receive a diagnosis of a depressive disorder.[20]
Side effect of medical treatment
It is possible that some early-generation beta-blockers induce depression in some patients, though the evidence for this is weak and conflicting. There is strong evidence for a link between alpha interferon therapy and depression. One study found that a third of alpha interferon-treated patients had developed depression after three months of treatment. (Beta interferon therapy appears to have no effect on rates of depression.) There is moderately strong evidence that finasteride when used in the treatment of alopecia increases depressive symptoms in some patients. Evidence linking isotretinoin, an acne treatment, to depression is strong.[21] Other medicines that seem to increase the risk of depression include anticonvulsants, antimigraine drugs, antipsychotics and hormonal agents such as gonadotropin-releasing hormone agonist.[22]
Substance-induced
Several drugs of abuse can cause or exacerbate depression, whether in intoxication, withdrawal, and from chronic use. These include alcohol, sedatives (including prescription benzodiazepines), opioids (including prescription pain killers and illicit drugs such as heroin), stimulants (such as cocaine and amphetamines), hallucinogens, and inhalants.[23]
Non-psychiatric illnesses
Depressed mood can be the result of a number of infectious diseases, nutritional deficiencies, neurological conditions,[24] and physiological problems, including hypoandrogenism (in men), Addison's disease, Cushing's syndrome, pernicious anemia, hypothyroidism, hyperparathyroidism, Lyme disease, multiple sclerosis, Parkinson's disease, chronic pain, stroke,[25] diabetes,[26] cancer,[27] and HIV.
Psychiatric syndromes
A number of psychiatric syndromes feature depressed mood as a main symptom. The mood disorders are a group of disorders considered to be primary disturbances of mood. These include major depressive disorder (commonly called major depression or clinical depression) where a person has at least two weeks of depressed mood or a loss of interest or pleasure in nearly all activities; and dysthymia, a state of chronic depressed mood, the symptoms of which do not meet the severity of a major depressive episode. Another mood disorder, bipolar disorder, features one or more episodes of abnormally elevated mood, cognition, and energy levels, but may also involve one or more episodes of depression.[28] When the course of depressive episodes follows a seasonal pattern, the disorder (major depressive disorder, bipolar disorder, etc.) may be described as a seasonal affective disorder.
Outside the mood disorders: borderline personality disorder often features an extremely intense depressive mood; adjustment disorder with depressed mood is a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode;[29] and posttraumatic stress disorder, a mental disorder that sometimes follows trauma, is commonly accompanied by depressed mood.[30]
Inflammation
There is evidence for a link between inflammation and depression.[31] Inflammatory processes can be triggered by negative cognitions or their consequences, such as stress, violence, or deprivation. Thus, negative cognitions can cause inflammation that can, in turn, lead to depression.[32][33] In addition, there is increasing evidence that inflammation can cause depression because of the increase of cytokines, setting the brain into a "sickness mode".[34] Classical symptoms of being physically sick, such as lethargy, show a large overlap in behaviors that characterize depression. Levels of cytokines tend to increase sharply during the depressive episodes of people with bipolar disorder and drop off during remission.[35] Furthermore, it has been shown in clinical trials that anti-inflammatory medicines taken in addition to antidepressants not only significantly improves symptoms but also increases the proportion of subjects positively responding to treatment.[36]
Inflammations that lead to serious depression could be caused by common infections such as those caused by a virus, bacteria or even parasites.[37]Measures
Measures of depression include, but are not limited to: Beck Depression Inventory-11 and the 9-item depression scale in the Patient Health Questionnaire (PHQ-9).[40] Both of these measures are psychological tests that ask personal questions of the participant, and have mostly been used to measure the severity of depression. The Beck Depression Inventory is a self-report scale that helps a therapist identify the patterns of depression symptoms and monitor recovery. The responses on this scale can be discussed in therapy to devise interventions for the most distressing symptoms of depression.[6]
Theories
Schools of depression theories include:
Management
Depressed mood may not require professional treatment, and may be a normal temporary reaction to life events, a symptom of some medical condition, or a side effect of some drugs or medical treatments. A prolonged depressed mood, especially in combination with other symptoms, may lead to a diagnosis of a psychiatric or medical condition which may benefit from treatment.
The UK National Institute for Health and Care Excellence (NICE) 2009 guidelines indicate that antidepressants should not be routinely used for the initial treatment of mild depression, because the risk-benefit ratio is poor.[41]
Physical activity has a protective effect against the emergence of depression in some people.[42]
There is limited evidence suggesting yoga may help some people with depressive disorders or elevated levels of depression, but more research is needed.[43][44]
Reminiscence of old and fond memories is another alternative form of treatment, especially for the elderly who have lived longer and have more experiences in life. It is a method that causes a person to recollect memories of their own life, leading to a process of self-recognition and identifying familiar stimuli. By maintaining one's personal past and identity, it is a technique that stimulates people to view their lives in a more objective and balanced way, causing them to pay attention to positive information in their life stories, which would successfully reduce depressive mood levels.[45]
There is limited evidence that continuing antidepressant medication for one year reduces the risk of depression recurrence with no additional harm.[46] Recommendations for psychological treatments or combination treatments in preventing recurrence are not clear.[46]
Epidemiology
Depression is the leading cause of disability worldwide, the United Nations (UN) health agency reported, estimating that it affects more than 300 million people worldwide – the majority of them women, young people and the elderly. An estimated 4.4 percent of the global population has depression, according to a report released by the UN World Health Organization (WHO), which shows an 18 percent increase in the number of people living with depression between 2005 and 2015.[47][48][49]
Depression is a major mental-health cause of disease burden. Its consequences further lead to significant burden in public health, including a higher risk of dementia, premature mortality arising from physical disorders, and maternal depression impacts on child growth and development.[50] Approximately 76% to 85% of depressed people in low- and middle-income countries do not receive treatment;[51] barriers to treatment include: inaccurate assessment, lack of trained health-care providers, social stigma and lack of resources.[4]
The stigma comes from misguided societal views that people with mental illness are different from everyone else, and they can choose to get better only if they wanted to.[52] Due to this more than half of the people with depression do not receive help with their disorders. The stigma leads to a strong preference for privacy.
The World Health Organization has constructed guidelines – known as The Mental Health Gap Action Programme (mhGAP) – aiming to increase services for people with mental, neurological and substance-use disorders.[4] Depression is listed as one of conditions prioritized by the programme. Trials conducted show possibilities for the implementation of the programme in low-resource primary-care settings dependent on primary-care practitioners and lay health-workers.[53] Examples of mhGAP-endorsed therapies targeting depression include Group Interpersonal Therapy as group treatment for depression and "Thinking Health", which utilizes cognitive behavioral therapy to tackle perinatal depression.[4] Furthermore, effective screening in primary care is crucial for the access of treatments. The mhGAP adopted its approach of improving detection rates of depression by training general practitioners. However, there is still weak evidence supporting this training.[50]
As of 2021, Iranians were one of the most depressed peoples on Earth, with the government reporting a 70% depression rate.[54][55][56][57][58][59]
History
The term depression was derived from the Latin verb deprimere, "to press down".[60] From the 14th century, "to depress" meant to subjugate or to bring down in spirits. It was used in 1665 in English author Richard Baker's Chronicle to refer to someone having "a great depression of spirit", and by English author Samuel Johnson in a similar sense in 1753.[61]
In Ancient Greece, disease was thought due to an imbalance in the four basic bodily fluids, or humors. Personality types were similarly thought to be determined by the dominant humor in a particular person. Derived from the Ancient Greek melas, "black", and kholé, "bile",[62] melancholia was described as a distinct disease with particular mental and physical symptoms by Hippocrates in his Aphorisms, where he characterized all "fears and despondencies, if they last a long time" as being symptomatic of the ailment.[63]
During the 18th century, the humoral theory of melancholia was increasingly being challenged by mechanical and electrical explanations; references to dark and gloomy states gave way to ideas of slowed circulation and depleted energy.[64] German physician Johann Christian Heinroth, however, argued melancholia was a disturbance of the soul due to moral conflict within the patient.
In the 20th century, the German psychiatrist Emil Kraepelin distinguished manic depression. The influential system put forward by Kraepelin unified nearly all types of mood disorder into manic–depressive insanity. Kraepelin worked from an assumption of underlying brain pathology, but also promoted a distinction between endogenous (internally caused) and exogenous (externally caused) types.[65]
Other psycho-dynamic theories were proposed. Existential and humanistic theories represented a forceful affirmation of individualism.[66] Austrian existential psychiatrist Viktor Frankl connected depression to feelings of futility and meaninglessness.[67] Frankl's logotherapy addressed the filling of an "existential vacuum" associated with such feelings, and may be particularly useful for depressed adolescents.[68][69]
Researchers theorized that depression was caused by a chemical imbalance in neurotransmitters in the brain, a theory based on observations made in the 1950s of the effects of reserpine and isoniazid in altering monoamine neurotransmitter levels and affecting depressive symptoms.[70] During the 1960s and 70s, manic-depression came to refer to just one type of mood disorder (now most commonly known as bipolar disorder) which was distinguished from (unipolar) depression. The terms unipolar and bipolar had been coined by German psychiatrist Karl Kleist.[65]
In July 2022, British psychiatrist Joanna Moncrieff, also psychiatrist Mark Horowtiz and others proposed in a study on academic journal Molecular Psychiatry that depression is not caused by a serotonin imbalance in the human body, unlike what most of the psychiatry community points to, and that therefore anti-depressants do not work against the illness.[71][72] However, such study was met with criticism from some psychiatrists, who argued the study's methodology used an indirect trace of serotonin, instead of taking direct measurements of the molecule.[73] Moncrieff said that, despite her study's conclusions, no one should interrupt their treatment if they are taking any anti-depressant.[73]
See also
- Alain Ehrenberg, French sociologist, author of Weariness of the Self: Diagnosing the History of Depression in the Contemporary Age
- Attribution (psychology) – The process by which individuals explain the causes of behavior and events
- Biopsychosocial model – Explanatory model emphasizing the interplay among causal forces
- Depression in childhood and adolescence – Pediatric depressive disorders
- Diathesis–stress model – Psychological theory
- Existential crisis – Inner conflict due to meaninglessness
- Feeling – Conscious subjective experience of emotion
- Locus of control – Concept in psychology
- Melancholia – Historical view of extreme depression
- Mixed anxiety–depressive disorder – Diagnostic category in the ICD-10
References
- "Depression". Cleveland Clinic. 2022. Retrieved 9 June 2022.
- Shrivastava A, Bureau Y, Rewari N, Johnston M (April 2013). "Clinical risk of stigma and discrimination of mental illnesses: Need for objective assessment and quantification". Indian Journal of Psychiatry. 55 (2): 178–82. doi:10.4103/0019-5545.111459. PMC 3696244. PMID 23825855.
- "NIMH » Depression Basics". www.nimh.nih.gov. 2016. Archived from the original on 11 June 2013. Retrieved 22 October 2020.
- "Depression". www.who.int. Archived from the original on 26 December 2020. Retrieved 7 April 2021.
- de Zwart PL, Jeronimus BF, de Jonge P (October 2019). "Empirical evidence for definitions of episode, remission, recovery, relapse and recurrence in depression: a systematic review". Epidemiology and Psychiatric Sciences. 28 (5): 544–562. doi:10.1017/S2045796018000227. PMC 7032752. PMID 29769159.
- Gilbert P (2007). Psychotherapy and counselling for depression (3rd ed.). Los Angeles: Sage. ISBN 978-1849203494. OCLC 436076587.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association.
- Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB (July 2008). "The link between childhood trauma and depression: insights from HPA axis studies in humans". Psychoneuroendocrinology. 33 (6): 693–710. doi:10.1016/j.psyneuen.2008.03.008. PMID 18602762. S2CID 2629673.
- Pillemer K, Suitor JJ, Pardo S, Henderson C (April 2010). "Mothers' Differentiation and Depressive Symptoms among Adult Children". Journal of Marriage and the Family. 72 (2): 333–345. doi:10.1111/j.1741-3737.2010.00703.x. PMC 2894713. PMID 20607119.
- Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG (April 2014). "Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis". International Journal of Public Health. 59 (2): 359–72. doi:10.1007/s00038-013-0519-5. PMID 24122075. S2CID 24138761.
- Schmidt PJ (December 2005). "Mood, depression, and reproductive hormones in the menopausal transition". The American Journal of Medicine. 118 (12B): 54–8. doi:10.1016/j.amjmed.2005.09.033. PMID 16414327.
- Rashid T, Haider I (31 January 2008). "Life Events and Depression". Annals of Punjab Medical College. 2 (1): 11–16. ISSN 2077-9143. Archived from the original on 1 November 2020. Retrieved 18 February 2022.
- Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, Sen S (December 2015). "Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis". JAMA. 314 (22): 2373–83. doi:10.1001/jama.2015.15845. PMC 4866499. PMID 26647259.
- "NIMH » Perinatal Depression". www.nimh.nih.gov. Archived from the original on 27 March 2020. Retrieved 29 October 2020.
- "Postpartum Depression". medlineplus.gov. Archived from the original on 27 July 2016. Retrieved 29 October 2020.
- Davey CG, Yücel M, Allen NB (2008). "The emergence of depression in adolescence: development of the prefrontal cortex and the representation of reward". Neuroscience and Biobehavioral Reviews. 32 (1): 1–19. doi:10.1016/j.neubiorev.2007.04.016. PMID 17570526. S2CID 20800688.
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, et al. (November 1996). "Childhood and adolescent depression: a review of the past 10 years. Part I". Journal of the American Academy of Child and Adolescent Psychiatry. 35 (11): 1427–1439. doi:10.1097/00004583-199611000-00011. PMID 8936909. S2CID 11623499.
- American Academy of Child & Adolescent Psychiatry. The Depressed Child, "Facts for Families," No. 4 (5/08)
- Kotov R, Gamez W, Schmidt F, Watson D (September 2010). "Linking "big" personality traits to anxiety, depressive, and substance use disorders: a meta-analysis". Psychological Bulletin. 136 (5): 768–821. doi:10.1037/a0020327. PMID 20804236.
- Jeronimus BF, Kotov R, Riese H, Ormel J (October 2016). "Neuroticism's prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants". Psychological Medicine. 46 (14): 2883–2906. doi:10.1017/S0033291716001653. PMID 27523506. S2CID 23548727. Archived from the original on 29 December 2019. Retrieved 5 July 2019.
- Rogers D, Pies R (December 2008). "General Medical Drugs Associated with Depression". Psychiatry. 5 (12): 28–41. PMC 2729620. PMID 19724774.
- Botts S, Ryan M. Drug-Induced Diseases Section IV: Drug-Induced Psychiatric Diseases Chapter 18: Depression. pp. 1–23. Archived from the original on 23 December 2010. Retrieved 14 January 2017.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA: American Psychiatric Association.
- Murray ED, Buttner N, Price BH. (2012) Depression and Psychosis in Neurological Practice. In: Neurology in Clinical Practice, 6th Edition. Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.) Butterworth Heinemann ISBN 978-1437704341
- Saravane D, Feve B, Frances Y, Corruble E, Lancon C, Chanson P, et al. (September 2009). "[Drawing up guidelines for the attendance of physical health of patients with severe mental illness]". L'Encéphale. 35 (4): 330–9. doi:10.1016/j.encep.2008.10.014. PMID 19748369.
- Rustad JK, Musselman DL, Nemeroff CB (October 2011). "The relationship of depression and diabetes: pathophysiological and treatment implications". Psychoneuroendocrinology. 36 (9): 1276–86. doi:10.1016/j.psyneuen.2011.03.005. PMID 21474250. S2CID 32439196.
- Li M, Fitzgerald P, Rodin G (April 2012). "Evidence-based treatment of depression in patients with cancer". Journal of Clinical Oncology. 30 (11): 1187–96. doi:10.1200/JCO.2011.39.7372. PMID 22412144.
- Gabbard G. Treatment of Psychiatric Disorders. Vol. 2 (3rd ed.). Washington, DC: American Psychiatric Publishing. p. 1296.
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision: DSM-IV-TR. Washington, DC: American Psychiatric Publishing, Inc. p. 355. ISBN 978-0890420256.
- Vieweg WV, Julius DA, Fernandez A, Beatty-Brooks M, Hettema JM, Pandurangi AK (May 2006). "Posttraumatic stress disorder: clinical features, pathophysiology, and treatment". The American Journal of Medicine. 119 (5): 383–90. doi:10.1016/j.amjmed.2005.09.027. PMID 16651048.
- Berk M, Williams LJ, Jacka FN, O'Neil A, Pasco JA, Moylan S, et al. (September 2013). "So depression is an inflammatory disease, but where does the inflammation come from?". BMC Medicine. 11: 200. doi:10.1186/1741-7015-11-200. PMC 3846682. PMID 24228900.
- Cox WT, Abramson LY, Devine PG, Hollon SD (September 2012). "Stereotypes, Prejudice, and Depression: The Integrated Perspective". Perspectives on Psychological Science. 7 (5): 427–49. doi:10.1177/1745691612455204. PMID 26168502. S2CID 1512121.
- Kiecolt-Glaser JK, Derry HM, Fagundes CP (November 2015). "Inflammation: depression fans the flames and feasts on the heat". The American Journal of Psychiatry. 172 (11): 1075–91. doi:10.1176/appi.ajp.2015.15020152. PMC 6511978. PMID 26357876.
- Williams C (4 January 2015). "Is depression a kind of allergic reaction?". The Guardian. Archived from the original on 21 October 2022. Retrieved 11 December 2016.
- Brietzke E, Stertz L, Fernandes BS, Kauer-Sant'anna M, Mascarenhas M, Escosteguy Vargas A, et al. (August 2009). "Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder". Journal of Affective Disorders. 116 (3): 214–7. doi:10.1016/j.jad.2008.12.001. PMID 19251324.
- Müller N, Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, et al. (July 2006). "The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine". Molecular Psychiatry. 11 (7): 680–4. doi:10.1038/sj.mp.4001805. PMID 16491133.
- Canli T (2014). "Reconceptualizing major depressive disorder as an infectious disease". Biology of Mood & Anxiety Disorders. 4: 10. doi:10.1186/2045-5380-4-10. PMC 4215336. PMID 25364500.
- Cvetkovich A (2012). Depression: A Public Feeling. Durham, NC: Duke University Press Books. ISBN 978-0822352389.
- Cox WT, Abramson LY, Devine PG, Hollon SD (September 2012). "Stereotypes, Prejudice, and Depression: The Integrated Perspective". Perspectives on Psychological Science. 7 (5): 427–49. doi:10.1177/1745691612455204. PMID 26168502. S2CID 1512121.
- Kroenke K, Spitzer RL, Williams JB (September 2001). "The PHQ-9: validity of a brief depression severity measure". Journal of General Internal Medicine. 16 (9): 606–13. doi:10.1046/j.1525-1497.2001.016009606.x. PMC 1495268. PMID 11556941.
- NICE guidelines, published October 2009 Archived 21 January 2021 at the Wayback Machine. Nice.org.uk. Retrieved on 2015-11-24.
- Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. (July 2018). "Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies" (PDF). The American Journal of Psychiatry. 175 (7): 631–648. doi:10.1176/appi.ajp.2018.17111194. PMID 29690792. Archived (PDF) from the original on 24 July 2019. Retrieved 5 July 2019.
- Cramer H, Lauche R, Langhorst J, Dobos G (November 2013). "Yoga for depression: a systematic review and meta-analysis". Depression and Anxiety. 30 (11): 1068–83. doi:10.1002/da.22166. PMID 23922209. S2CID 8892132.
- Grensman A, Acharya BD, Wändell P, Nilsson GH, Falkenberg T, Sundin Ö, Werner S (March 2018). "Effect of traditional yoga, mindfulness-based cognitive therapy, and cognitive behavioral therapy, on health related quality of life: a randomized controlled trial on patients on sick leave because of burnout". BMC Complementary and Alternative Medicine. 18 (1): 80. doi:10.1186/s12906-018-2141-9. PMC 5839058. PMID 29510704.
- Viguer P, Satorres E, Fortuna FB, Meléndez JC (November 2017). "A Follow-Up Study of a Reminiscence Intervention and Its Effects on Depressed Mood, Life Satisfaction, and Well-Being in the Elderly". The Journal of Psychology. 151 (8): 789–803. doi:10.1080/00223980.2017.1393379. PMID 29166223. S2CID 21839684.
- Wilkinson P, Izmeth Z (September 2016). "Continuation and maintenance treatments for depression in older people". The Cochrane Database of Systematic Reviews. 2016 (9): CD006727. doi:10.1002/14651858.cd006727.pub3. PMC 6457610. PMID 27609183. Archived from the original on 18 February 2022. Retrieved 3 August 2021.
- "UN health agency reports depression now 'leading cause of disability worldwide'". UN News. 23 February 2017. Archived from the original on 27 June 2019. Retrieved 27 June 2019.
- Solomon A (17 November 2006). "Opinion | Our Great Depression". The New York Times. ISSN 0362-4331. Archived from the original on 27 June 2019. Retrieved 27 June 2019.
- Agence France-Presse (31 March 2017). "Depression is leading cause of disability worldwide, says WHO study". The Guardian. ISSN 0261-3077. Archived from the original on 27 June 2019. Retrieved 27 June 2019.
- Reynolds CF, Patel V (October 2017). "Screening for depression: the global mental health context". World Psychiatry. 16 (3): 316–317. doi:10.1002/wps.20459. PMC 5608832. PMID 28941110.
- Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. (September 2007). "Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys". Lancet. 370 (9590): 841–50. doi:10.1016/s0140-6736(07)61414-7. PMC 2847360. PMID 17826169.
- "Stigma and Discrimination". www.psychiatry.org. Archived from the original on 1 May 2021. Retrieved 1 May 2021.
- Patel V, Weobong B, Nadkarni A, Weiss HA, Anand A, Naik S, et al. (April 2014). "The effectiveness and cost-effectiveness of lay counsellor-delivered psychological treatments for harmful and dependent drinking and moderate to severe depression in primary care in India: PREMIUM study protocol for randomized controlled trials". Trials. 15 (1): 101. doi:10.1186/1745-6215-15-101. PMC 4230277. PMID 24690184.
- "شیوع ۶۷ درصدی افسردگی در جامعه ایرانی! – همشهری آنلاین". www.hamshahrionline.ir.
- "هشدار کارشناسان درباره اختلالات روان در جامعه فقیر و افسرده؛ ایران دچار ترومای جمعی شده". اعتمادآنلاین. 12 July 2023.
- "رتبه جدید ایران در فهرست غمگینترین کشورهای جهان | به آخر جدول نزدیک شدیم! – همشهری آنلاین". www.hamshahrionline.ir.
- "'اعلان خطر' وزیر بهداشت ایران درباره شیوع افسردگی و مشکلات روانی". BBC News فارسی. 22 December 2019.
- "شیوع افسردگی در ایران؛ انتقاد وزیر بهداشت از کمبود نشاط – DW – ۱۳۹۸/۱۰/۱". dw.com.
- "افزایش افسردگی و خودکشی میان ایرانیان". www.radiofarda.com.
- depress. (n.d.). Online Etymology Dictionary. Retrieved June 30, 2008, from dictionary.com
- Wolpert, L. "Malignant Sadness: The Anatomy of Depression". The New York Times. Retrieved 30 October 2008.
- Liddell, Henry; Robert Scott (1980). A Greek-English Lexicon (Abridged ed.). United Kingdom: Oxford University Press. ISBN 0-19-910207-4.
- Hippocrates, Aphorisms, Section 6.23
- Jackson SW (July 1983). "Melancholia and mechanical explanation in eighteenth-century medicine". Journal of the History of Medicine and Allied Sciences. 38 (3): 298–319. doi:10.1093/jhmas/38.3.298. PMID 6350428.
- Davison K (2006). "Historical aspects of mood disorders". Psychiatry. 5 (4): 115–18. doi:10.1383/psyt.2006.5.4.115.
- A. Freeman; N. Epstein; K.M. Simon (1987), Depression in the family, New York: Haworth Press, pp. 64, 66
- Frankl VE (2000). Man's search for ultimate meaning. New York, NY, USA: Basic Books. pp. 139–40. ISBN 0-7382-0354-8.
- Seidner, Stanley S. (June 10, 2009) "A Trojan Horse: Logotherapeutic Transcendence and its Secular Implications for Theology" Archived 1 May 2011 at the Wayback Machine. Mater Dei Institute. pp 14–15.
- Blair RG (October 2004). "Helping older adolescents search for meaning in depression". Journal of Mental Health Counseling. 26 (4): 333–347. doi:10.17744/mehc.26.4.w8u9h6uf5ybhapyl.
- Schildkraut JJ (1965). "The catecholamine hypothesis of affective disorders: A review of supporting evidence". American Journal of Psychiatry. 122 (5): 509–22. doi:10.1176/ajp.122.5.509. PMID 5319766.
- Moncrieff, Joanna; Cooper, Ruth E.; Stockmann, Tom; Amendola, Simone; Hengartner, Michael P.; Horowitz, Mark A. (20 July 2022). "The serotonin theory of depression: a systematic umbrella review of the evidence". Molecular Psychiatry: 1–14. doi:10.1038/s41380-022-01661-0. ISSN 1476-5578. PMID 35854107. S2CID 250646781.
- Moncrieff, Joanna; Horowitz, Mark (20 July 2022). "Depression is probably not caused by a chemical imbalance in the brain – new study". The Conversation. Retrieved 11 August 2022.
- "Study on serotonin and depression sparks fierce debate". France 24. 11 August 2022. Retrieved 11 August 2022.
External links
 Media related to Depression (mood) at Wikimedia Commons
Media related to Depression (mood) at Wikimedia Commons