Didanosine
Didanosine (ddI, DDI), sold under the brand name Videx, is a medication used to treat HIV/AIDS.[1] It is used in combination with other medications as part of highly active antiretroviral therapy (HAART). It is of the reverse-transcriptase inhibitor class.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Videx |
| Other names | 2′,3′-dideoxyinosine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a691006 |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 30 to 54% |
| Protein binding | Less than 5% |
| Elimination half-life | 1.5 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.129.182 |
| Chemical and physical data | |
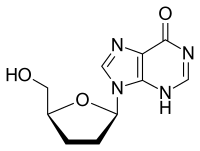
| Formula | C10H12N4O3 |
| Molar mass | 236.231 g·mol−1 |
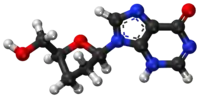
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Didanosine was first described in 1975 and approved for use in the United States in 1991.[2]
Adverse effects
The most common adverse events with didanosine are diarrhea, nausea, vomiting, abdominal pain, fever, headache, and rash.[3] Peripheral neuropathy occurred in 21-26% of participants in key didanosine trials.[4]
Pancreatitis is rarely observed but has caused occasional fatalities, and has black box warning status.[5] Other reported serious adverse events are retinal changes, optic neuritis and alterations of liver functions. The risk of some of these serious adverse events is increased by drinking alcohol.
In February 2010, the United States Food and Drug Administration issued a statement that patients using didanosine (Videx) are at risk for a rare but potentially fatal liver disorder, non-cirrhotic portal hypertension.[6]
Drug interactions
- A significant interaction has also been recorded with allopurinol, and administration of these drugs together should be avoided.[4]
- Reduction in indinavir and delavirdine plasma levels have been shown to occur when administered simultaneously with didanosine; these drugs should be administered at different times.[4]
- Ketoconazole, itraconazole, ciprofloxacin should be administered at a different time from didanosine due to interactions with the buffering agent.[4]
- Administration with drugs with overlapping toxicity, such as zalcitabine and stavudine, is not recommended.[7]
- Alcohol can exacerbate didanosine's toxicity, and avoiding drinking alcohol while taking didanosine is recommended.[4]
Resistance
Drug resistance to didanosine does develop, though slower than to zidovudine (ZDV). The most common mutation observed in vivo is L74V in the viral pol gene, which confers cross-resistance to zalcitabine; other mutations observed include K65R and M184V .[4][8]
Mechanism of action
Didanosine (ddI) is a nucleoside analogue of adenosine.[9] It differs from other nucleoside analogues, because it does not have any of the regular bases, instead it has hypoxanthine attached to the sugar ring. Within the cell, ddI is phosphorylated to the active metabolite of dideoxyadenosine triphosphate, ddATP, by cellular enzymes. Like other anti-HIV nucleoside analogs, it acts as a chain terminator by incorporation and inhibits viral reverse transcriptase by competing with natural dATP.
Pharmacokinetics
Oral absorption of didanosine is fairly low (42%)[4] but rapid. Food substantially reduces didanosine bioavailability, and the drug should be administered on an empty stomach.[4] The half-life in plasma is only 1.5 hours,[4] but in the intracellular environment more than 12 hours. An enteric-coated formulation is now marketed as well. Elimination is predominantly renal; the kidneys actively secrete didanosine, the amount being 20% of the oral dose.
History
The related pro-drug of didanosine, 2′,3′-dideoxyadenosine (ddA), was initially synthesized by Morris J. Robins (professor of Organic Chemistry at Brigham Young University) and R.K. Robins in 1964. Subsequently, Samuel Broder, Hiroaki Mitsuya, and Robert Yarchoan in the National Cancer Institute (NCI) found that ddA and ddI could inhibit HIV replication in the test tube and conducted initial clinical trials showing that didanosine had activity in patients infected with HIV. On behalf of the NCI, they were awarded patents on these activities. Since the NCI does not market products directly, the National Institutes of Health (NIH) awarded a ten-year exclusive license to Bristol-Myers Squibb Co. (BMS) to market and sell ddI as Videx tablets.
Didanosine became the second drug approved for the treatment of HIV infection in many other countries, including in the United States by the Food and Drug Administration (FDA) on October 9, 1991. Its FDA approval helped bring down the price of zidovudine (ZDV), the initial anti-HIV drug. [Source needed on pricing effect.]
Didanosine has weak acid stability and is easily damaged by stomach acid. Therefore, the original formula approved by the FDA used chewable tablets that included an antacid buffering compound to neutralize stomach acid. The chewable tablets were not only large and fragile, they also were foul-tasting and the buffering compound would cause diarrhea. Although the FDA had not approved the original formulation for once-a-day dosing it was possible for some people to take it that way.
At the end of its ten-year license, BMS re-formulated Videx as Videx EC and patented that, which reformulation the FDA approved in 2000. The new formulation is a smaller capsule containing coated microspheres instead of using a buffering compound. It is approved by the FDA for once-a-day dosing. Also at the end of that ten-year period, the NIH licensed didanosine to Barr Laboratories under a non-exclusive license, and didanosine became the first generic anti-HIV drug marketed in the United States.
One of the patents for ddI expired in the United States on August 29, 2006, but other patents extend beyond that time.
Sources
- "didanosine, Videx, Videx EC: Drug Facts, Side Effects and Dosing". MedicineNet. Retrieved 2018-08-08.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 505. ISBN 9783527607495.
- "Didanosine Side Effects in Detail - Drugs.com". Drugs.com. Retrieved 2018-08-08.
- "VIDEX (didanosine): chewable/dispersible buffered tablets; buffered powder for oral solution; pediatric powder for oral solution". U.S. Food and Drug Administration. July 2000.
- "Didanosine Videx - Treatment - National HIV Curriculum". www.hiv.uw.edu. Retrieved 2018-08-08.
- "Serious liver disorder associated with the use of Videx/Videx EC (didanosine)". FDA Drug Safety Communication. U.S. Food and Drug Administration. 19 January 2010.
- DHHS Panel (May 4, 2006). "Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents". AIDSInfo. U.S. Department of Health and Human Services. Archived from the original on 2006-05-06.
- Moyle GJ (August 1996). "Use of viral resistance patterns to antiretroviral drugs in optimising selection of drug combinations and sequences". Drugs. 52 (2): 168–85. doi:10.2165/00003495-199652020-00002. PMID 8841736. S2CID 27709969.
- Pruvost A, Negredo E, Benech H, Theodoro F, Puig J, Grau E, et al. (May 2005). "Measurement of intracellular didanosine and tenofovir phosphorylated metabolites and possible interaction of the two drugs in human immunodeficiency virus-infected patients". Antimicrobial Agents and Chemotherapy. 49 (5): 1907–14. doi:10.1128/AAC.49.5.1907-1914.2005. PMC 1087635. PMID 15855513.
Further reading
- Robins MJ, McCarthy JR, Robins RK (January 1966). "Purine nucleosides. XII. The preparation of 2',3'-dideoxyadenosine, 2',5'-dideoxyadenosine, and 2',3',5'-trideoxyadenosine from 2'-deoxyadenosine". Biochemistry. 5 (1): 224–31. doi:10.1021/bi00865a029. PMID 5938940.
- Yarchoan R, Mitsuya H, Broder S (October 1988). "AIDS therapies". Scientific American. 259 (4): 110–9. Bibcode:1988SciAm.259d.110Y. doi:10.1038/scientificamerican1088-110. PMID 3072667.
- Männistö PT, Tuominen RK (1996). Koulu M, Tuomisto J, Paasonen MK (eds.). Farmakologia ja Toksikologia (5th ed.). Medicina.
- Rang HP, Dale MM, Ritter JM (1995). Pharmacology (3rd ed.). Pearson Professional Ltd.
- Watson JD, Hopkins NH, Roberts JW, Steitz JA, Weiner AM (1987). Molecular Biology of the Gene (4th ed.). Benjamin/Cummings. ISBN 978-0-8053-9612-6.
- Mitsuya H, Yarchoan R, Broder S (September 1990). "Molecular targets for AIDS therapy". Science. 249 (4976): 1533–44. Bibcode:1990Sci...249.1533M. doi:10.1126/science.1699273. PMID 1699273.
- Yarchoan R, Mitsuya H, Thomas RV, Pluda JM, Hartman NR, Perno CF, et al. (July 1989). "In vivo activity against HIV and favorable toxicity profile of 2',3'-dideoxyinosine". Science. 245 (4916): 412–5. Bibcode:1989Sci...245..412Y. doi:10.1126/science.2502840. PMID 2502840.
- "NIH Oral History of Samuel Broder describing development of AIDS drugs". Office of NIH History. February 2, 1997.
- "NIH Oral History of Robert Yarchoan describing development of AIDS drugs". Office of NIH History. April 3, 1998.
- "Report on Development and Licensing of ddI" (PDF). National Institutes of Health Office of Technology Transfer. September 2003. Archived from the original (PDF) on 2006-09-30.
External links
- "Didanosine". Drug Information Portal. U.S. National Library of Medicine.