Epidermis
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and hypodermis.[1] The epidermis layer provides a barrier to infection from environmental pathogens[2] and regulates the amount of water released from the body into the atmosphere through transepidermal water loss.[3]
| Epidermis | |
|---|---|
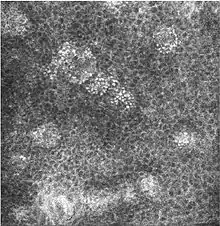
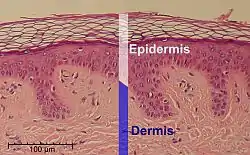 Microscopic image of the epidermis, which constitutes the outer layer of skin, shown here by the white bar | |
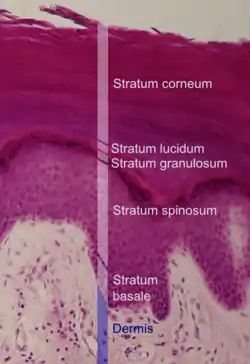 Microscopic image showing the layers of the epidermis. The stratum corneum appears more compact in this image than above because of different sample preparation. | |
| Details | |
| Part of | Skin |
| System | Integumentary system |
| Identifiers | |
| Latin | Epidermis |
| MeSH | D004817 |
| TA98 | A16.0.00.009 |
| TA2 | 7046 |
| TH | H3.12.00.1.01001 |
| FMA | 70596 |
| Anatomical terms of microanatomy | |
The epidermis is composed of multiple layers of flattened cells[4] that overlie a base layer (stratum basale) composed of columnar cells arranged perpendicularly. The layers of cells develop from stem cells in the basal layer. The human epidermis is a familiar example of epithelium, particularly a stratified squamous epithelium.
The word epidermis is derived through Latin from Ancient Greek epidermis, itself from Ancient Greek epi 'over, upon' and from Ancient Greek derma 'skin'. Something related to or part of the epidermis is termed epidermal.
Structure
Cellular components
The epidermis primarily consists of keratinocytes[4] (proliferating basal and differentiated suprabasal), which comprise 90% of its cells, but also contains melanocytes, Langerhans cells, Merkel cells,[5]: 2–3 and inflammatory cells. Epidermal thickenings called Rete ridges (or rete pegs) extend downward between dermal papillae.[6] Blood capillaries are found beneath the epidermis, and are linked to an arteriole and a venule. The epidermis itself has no blood supply and is nourished almost exclusively by diffused oxygen from the surrounding air.[7] Cellular mechanisms for regulating water and sodium levels (ENaCs) are found in all layers of the epidermis.[8]
Cell junctions
Epidermal cells are tightly interconnected to serve as a tight barrier against the exterior environment. The junctions between the epidermal cells are of the adherens junction type, formed by transmembrane proteins called cadherins. Inside the cell, the cadherins are linked to actin filaments. In immunofluorescence microscopy, the actin filament network appears as a thick border surrounding the cells,[8] although the actin filaments are actually located inside the cell and run parallel to the cell membrane. Because of the proximity of the neighboring cells and tightness of the junctions, the actin immunofluorescence appears as a border between cells.[8]
Layers
The epidermis is composed of 4 or 5 layers, depending on the region of skin being considered.[9] Those layers from outermost to innermost are:[2]
- cornified layer (stratum corneum)
- Composed of 10 to 30 layers of polyhedral, anucleated corneocytes (final step of keratinocyte differentiation), with the palms and soles having the most layers. Corneocytes contain a protein envelope (cornified envelope proteins) underneath the plasma membrane, are filled with water-retaining keratin proteins, attached together through corneodesmosomes and surrounded in the extracellular space by stacked layers of lipids.[10] Most of the barrier functions of the epidermis localize to this layer.[11]
 Confocal image of the stratum corneum
Confocal image of the stratum corneum - clear/translucent layer (stratum lucidum, only in palms and soles)
- This narrow layer is found only on the palms and soles. The epidermis of these two areas is known as "thick skin" because with this extra layer, the skin has 5 epidermal layers instead of 4.
- granular layer (stratum granulosum)
- Keratinocytes lose their nuclei and their cytoplasm appears granular. Lipids, contained into those keratinocytes within lamellar bodies, are released into the extracellular space through exocytosis to form a lipid barrier that prevents water loss from the body as well as entry of foreign substances. Those polar lipids are then converted into non-polar lipids and arranged parallel to the cell surface. For example glycosphingolipids become ceramides and phospholipids become free fatty acids.[10]
 Confocal image of the stratum granulosum
Confocal image of the stratum granulosum - spinous layer (stratum spinosum)
- Keratinocytes become connected through desmosomes and produce lamellar bodies, from within the Golgi, enriched in polar lipids, glycosphingolipids, free sterols, phospholipids and catabolic enzymes.[3] Langerhans cells, immunologically active cells, are located in the middle of this layer.[10]
 Confocal image of the stratum spinosum already showing some clusters of basal cells
Confocal image of the stratum spinosum already showing some clusters of basal cells - basal/germinal layer (stratum basale/germinativum)
- Composed mainly of proliferating and non-proliferating keratinocytes, attached to the basement membrane by hemidesmosomes. Melanocytes are present, connected to numerous keratinocytes in this and other strata through dendrites. Merkel cells are also found in the stratum basale with large numbers in touch-sensitive sites such as the fingertips and lips. They are closely associated with cutaneous nerves and seem to be involved in light touch sensation.[10]
 Confocal image of the stratum basale already showing some papillae
Confocal image of the stratum basale already showing some papillae - Malpighian layer (stratum malpighii)
- This is usually defined as both the stratum basale and stratum spinosum.[4]
The epidermis is separated from the dermis, its underlying tissue, by a basement membrane.
Cell division
As a stratified squamous epithelium, the epidermis is maintained by cell division within the stratum basale. Differentiating cells delaminate from the basement membrane and are displaced outward through the epidermal layers, undergoing multiple stages of differentiation until, in the stratum corneum, losing their nucleus and fusing to squamous sheets, which are eventually shed from the surface (desquamation). Differentiated keratinocytes secrete keratin proteins, which contribute to the formation of an extracellular matrix that is an integral part of the skin barrier function. In normal skin, the rate of keratinocyte production equals the rate of loss,[4] taking about two weeks for a cell to journey from the stratum basale to the top of the stratum granulosum, and an additional four weeks to cross the stratum corneum.[2] The entire epidermis is replaced by new cell growth over a period of about 48 days.[12]
Calcium concentration
Keratinocyte differentiation throughout the epidermis is in part mediated by a calcium gradient, increasing from the stratum basale until the outer stratum granulosum, where it reaches its maximum, and decreasing in the stratum corneum. Calcium concentration in the stratum corneum is very low in part because those relatively dry cells are not able to dissolve the ions. This calcium gradient parallels keratinocyte differentiation and as such is considered a key regulator in the formation of the epidermal layers.[3]
Elevation of extracellular calcium concentrations induces an increase in intracellular free calcium concentrations.[13] Part of that intracellular increase comes from calcium released from intracellular stores[14] and another part comes from transmembrane calcium influx,[15] through both calcium-sensitive chloride channels[16] and voltage-independent cation channels permeable to calcium.[17] Moreover, it has been suggested that an extracellular calcium-sensing receptor (CaSR) also contributes to the rise in intracellular calcium concentration.[18]
Development
Epidermal organogenesis, the formation of the epidermis, begins in the cells covering the embryo after neurulation, the formation of the central nervous system. In most vertebrates, this original one-layered structure quickly transforms into a two-layered tissue; a temporary outer layer, the periderm, which is disposed once the inner basal layer or stratum germinativum has formed.[19]
This inner layer is a germinal epithelium that gives rise to all epidermal cells. It divides to form the outer spinous layer (stratum spinosum). The cells of these two layers, together called the Malpighian layer(s) after Marcello Malpighi, divide to form the superficial granular layer (Stratum granulosum) of the epidermis.[19]
The cells in the stratum granulosum do not divide, but instead form skin cells called keratinocytes from the granules of keratin. These skin cells finally become the cornified layer (stratum corneum), the outermost epidermal layer, where the cells become flattened sacks with their nuclei located at one end of the cell. After birth these outermost cells are replaced by new cells from the stratum granulosum and throughout life they are shed at a rate of 30 - 90 milligrams of skin flakes every hour, or 0.720 - 2.16 grams per day.[20]
Epidermal development is a product of several growth factors, two of which are:[19]
- Transforming growth factor Alpha (TGFα) is an autocrine growth factor by which basal cells stimulate their own division.
- Keratinocyte growth factor (KGF or FGF7) is a paracrine growth factor produced by the underlying dermal fibroblasts in which the proliferation of basal cells is regulated.
Function
Barrier
The epidermis serves as a barrier to protect the body against microbial pathogens, oxidant stress (UV light), and chemical compounds, and provides mechanical resistance to minor injury. Most of this barrier role is played by the stratum corneum.[11]
- Characteristics
- Physical barrier: Epidermal keratinocytes are tightly linked by cell–cell junctions associated to cytoskeletal proteins, giving the epidermis its mechanical strength.[3]
- Chemical barrier: Highly organized lipids, acids, hydrolytic enzymes, and antimicrobial peptides[3] inhibit passage of external chemicals and pathogens into the body.
- Immunologically active barrier: The humoral and cellular constituents of the immune system[3] found in the epidermis actively combat infection.
- Water content of the stratum corneum drops towards the surface, creating hostile conditions for pathogenic microorganism growth.[11]
- An acidic pH (around 5.0) and low amounts of water make the epidermis hostile to many microorganic pathogens.[11]
- Non-pathogenic microorganisms on the surface of the epidermis help defend against pathogens by competing for food, limiting its availability, and producing chemical secretions that inhibit the growth of pathogenic microbiota.[11]
- Permeability
- Psychological stress, through an increase in glucocorticoids, compromises the stratum corneum and thus the barrier function.[21]
- Sudden and large shifts in humidity alter stratum corneum hydration in a way that could allow entry of pathogenic microorganisms.[22]
Skin hydration
The ability of the skin to hold water is primarily due to the stratum corneum and is critical for maintaining healthy skin.[23] Skin hydration is quantified using corneometry.[24] Lipids arranged through a gradient and in an organized manner between the cells of the stratum corneum form a barrier to transepidermal water loss.[25][26]
Skin color
The amount and distribution of melanin pigment in the epidermis is the main reason for variation in skin color in Homo sapiens. Melanin is found in the small melanosomes, particles formed in melanocytes from where they are transferred to the surrounding keratinocytes. The size, number, and arrangement of the melanosomes vary between racial groups, but while the number of melanocytes can vary between different body regions, their numbers remain the same in individual body regions in all human beings. In white and Asian skin the melanosomes are packed in "aggregates", but in black skin they are larger and distributed more evenly. The number of melanosomes in the keratinocytes increases with UV radiation exposure, while their distribution remain largely unaffected.[27]
Touch
The skin contains specialized epidermal touch receptor cells called Merkel cells. Historically, the role of Merkel cells in sensing touch has been thought to be indirect, due their close association with nerve endings. However, recent work in mice and other model organisms demonstrates that Merkel cells intrinsically transform touch into electrical signals that are transmitted to the nervous system.[28]
Clinical significance
Laboratory culture of keratinocytes to form a 3D structure (artificial skin) recapitulating most of the properties of the epidermis is routinely used as a tool for drug development and testing.
Hyperplasia
Epidermal hyperplasia (thickening resulting from cell proliferation) has various forms:
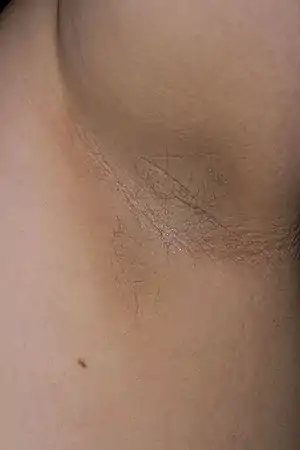
- Acanthosis is diffuse epidermal hyperplasia (thickening of the skin, and not to be confused with acanthocytes).[29] It implies increased thickness of the Malpighian layer (stratum basale and stratum spinosum).[30] Acanthosis nigricans is a black, poorly defined, velvety hyperpigmented acanthosis, usually observed in the back of neck, axilla, and other folded regions of the skin.
- Focal epithelial hyperplasia (Heck's disease) is an asymptomatic, benign neoplastic condition characterized by multiple white to pinkish papules that occur diffusely in the oral cavity.[31][5]: 411
- Pseudoepitheliomatous hyperplasia (PEH) is a benign condition characterized by hyperplasia of the epidermis and epithelium of skin appendages,[32] with irregular squamous strands extending down into the dermis,[33] and closely simulating squamous cell carcinoma (SCC).[32]

 Pseudoepitheliomatous hyperplasia (PEH), low magnification, with acanthotic squamous epithelium with irregular thick finger-like downgrowths into the underlying dermis.
Pseudoepitheliomatous hyperplasia (PEH), low magnification, with acanthotic squamous epithelium with irregular thick finger-like downgrowths into the underlying dermis.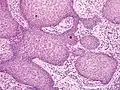 PEH, high magnification, with reactive-appearing squamous downgrowths with no significant cytologic atypia.
PEH, high magnification, with reactive-appearing squamous downgrowths with no significant cytologic atypia.
In contract, hyperkeratosis is a thickening of the stratum corneum, and is not necessarily due to hyperplasia.
Additional images
 Epidermis and dermis of human skin
Epidermis and dermis of human skin Cross-section of all skin layers
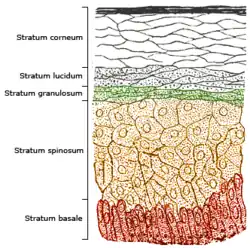
Cross-section of all skin layers Illustration of epidermal layers
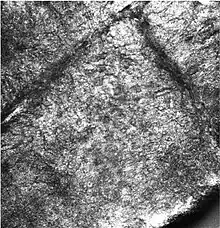
Illustration of epidermal layers Optical coherence tomography of fingertip
Optical coherence tomography of fingertip
References
- Young B (2014). Wheater's functional histology a text and colour atlas. Elsevier. pp. 160 & 175. ISBN 9780702047473.
- Marks JG, Miller J (2006). Lookingbill and Marks' Principles of Dermatology (4th ed.). Elsevier. pp. 1–7. ISBN 978-1-4160-3185-7.
- Proksch E, Brandner JM, Jensen JM (December 2008). "The skin: an indispensable barrier". Experimental Dermatology. 17 (12): 1063–1072. doi:10.1111/j.1600-0625.2008.00786.x. PMID 19043850. S2CID 31353914.
- McGrath JA, Eady RA, Pope FM (2004). Rook's Textbook of Dermatology (7th ed.). Blackwell Publishing. pp. 3.1–3.6. ISBN 978-0-632-06429-8.
- James WD, Berger TG, Elston DM, Aydemir EH, Odom RB (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- TheFreeDictionary > rete ridge Citing: The American Heritage Medical Dictionary Copyright 2007, 2004
- Stücker M, Struk A, Altmeyer P, Herde M, Baumgärtl H, Lübbers DW (February 2002). "The cutaneous uptake of atmospheric oxygen contributes significantly to the oxygen supply of human dermis and epidermis". The Journal of Physiology. 538 (Pt 3): 985–994. doi:10.1113/jphysiol.2001.013067. PMC 2290093. PMID 11826181.
- Hanukoglu I, Boggula VR, Vaknine H, Sharma S, Kleyman T, Hanukoglu A (June 2017). "Expression of epithelial sodium channel (ENaC) and CFTR in the human epidermis and epidermal appendages". Histochemistry and Cell Biology. 147 (6): 733–748. doi:10.1007/s00418-016-1535-3. PMID 28130590. S2CID 8504408.
- Betts JG, et al. (2022). Anatomy and Physiology (2nd ed.). OpenStax. p. 164. ISBN 978-1-711494-06-7.
- "Skin structure and function" (PDF). Archived from the original (PDF) on 2010-12-14. Retrieved 2015-01-07.
- Elias PM (April 2007). "The skin barrier as an innate immune element". Seminars in Immunopathology. 29 (1): 3–14. doi:10.1007/s00281-007-0060-9. PMID 17621950. S2CID 20311780.
- Iizuka H (December 1994). "Epidermal turnover time". Journal of Dermatological Science. 8 (3): 215–217. doi:10.1016/0923-1811(94)90057-4. PMID 7865480.
- Hennings H, Kruszewski FH, Yuspa SH, Tucker RW (April 1989). "Intracellular calcium alterations in response to increased external calcium in normal and neoplastic keratinocytes". Carcinogenesis. 10 (4): 777–780. doi:10.1093/carcin/10.4.777. PMID 2702726.
- Pillai S, Bikle DD (January 1991). "Role of intracellular-free calcium in the cornified envelope formation of keratinocytes: differences in the mode of action of extracellular calcium and 1,25 dihydroxyvitamin D3". Journal of Cellular Physiology. 146 (1): 94–100. doi:10.1002/jcp.1041460113. PMID 1990023. S2CID 21264605.
- Reiss M, Lipsey LR, Zhou ZL (May 1991). "Extracellular calcium-dependent regulation of transmembrane calcium fluxes in murine keratinocytes". Journal of Cellular Physiology. 147 (2): 281–291. doi:10.1002/jcp.1041470213. PMID 1645742. S2CID 25858560.
- Mauro TM, Pappone PA, Isseroff RR (April 1990). "Extracellular calcium affects the membrane currents of cultured human keratinocytes". Journal of Cellular Physiology. 143 (1): 13–20. doi:10.1002/jcp.1041430103. PMID 1690740. S2CID 8072916.
- Mauro TM, Isseroff RR, Lasarow R, Pappone PA (March 1993). "Ion channels are linked to differentiation in keratinocytes". The Journal of Membrane Biology. 132 (3): 201–209. doi:10.1007/BF00235738. PMID 7684087. S2CID 13063458.
- Tu CL, Oda Y, Bikle DD (September 1999). "Effects of a calcium receptor activator on the cellular response to calcium in human keratinocytes". The Journal of Investigative Dermatology. 113 (3): 340–345. doi:10.1046/j.1523-1747.1999.00698.x. PMID 10469331.
- Gilbert SF (2000). "The Epidermis and the Origin of Cutaneous Structures". Developmental Biology. Sinauer Associates. ISBN 978-0-87893-243-6.
- Weschler CJ, Langer S, Fischer A, Bekö G, Toftum J, Clausen G (May 2011). "Squalene and cholesterol in dust from danish homes and daycare centers" (PDF). Environmental Science & Technology. 45 (9): 3872–3879. Bibcode:2011EnST...45.3872W. doi:10.1021/es103894r. PMID 21476540. S2CID 1468347.
- Denda M, Tsuchiya T, Elias PM, Feingold KR (February 2000). "Stress alters cutaneous permeability barrier homeostasis". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 278 (2): R367–R372. doi:10.1152/ajpregu.2000.278.2.R367. PMID 10666137. S2CID 558526.
- Tsai JC, Guy RH, Thornfeldt CR, Gao WN, Feingold KR, Elias PM (June 1996). "Metabolic approaches to enhance transdermal drug delivery. 1. Effect of lipid synthesis inhibitors". Journal of Pharmaceutical Sciences. 85 (6): 643–648. doi:10.1021/js950219p. PMID 8773963.
- Blank IH (June 1952). "Factors which influence the water content of the stratum corneum". The Journal of Investigative Dermatology. 18 (6): 433–440. doi:10.1038/jid.1952.52. PMID 14938659.
- Blichmann CW, Serup J (1988). "Assessment of skin moisture. Measurement of electrical conductance, capacitance and transepidermal water loss". Acta Dermato-venereologica. 68 (4): 284–90. doi:10.2340/0001555568284290 (inactive 1 August 2023). PMID 2459872.
{{cite journal}}: CS1 maint: DOI inactive as of August 2023 (link) - Downing DT, Stewart ME, Wertz PW, Colton SW, Abraham W, Strauss JS (March 1987). "Skin lipids: an update". The Journal of Investigative Dermatology. 88 (3 Suppl): 2s–6s. doi:10.1111/1523-1747.ep12468850. PMID 2950180.
- Bonté F, Saunois A, Pinguet P, Meybeck A (January 1997). "Existence of a lipid gradient in the upper stratum corneum and its possible biological significance". Archives of Dermatological Research. 289 (2): 78–82. doi:10.1007/s004030050158. PMID 9049040. S2CID 10787600.
- Montagna W, Prota G, Kenney JA (1993). Black skin: structure and function. Gulf Professional Publishing. p. 69. ISBN 978-0-12-505260-3.
- Moehring F, Halder P, Seal RP, Stucky CL (October 2018). "Uncovering the Cells and Circuits of Touch in Normal and Pathological Settings". Neuron. 100 (2): 349–360. doi:10.1016/j.neuron.2018.10.019. PMC 6708582. PMID 30359601.
- Kumar V, Fausto N, Abbas A (2004). Robbins & Cotran Pathologic Basis of Disease (7th ed.). Saunders. p. 1230. ISBN 0-7216-0187-1.
- Stone MS, Ray TL (September 1995). "Acanthosis". DermPathTutor. Department of Dermatology, University of Iowa. Archived from the original on 29 May 2012. Retrieved 17 May 2012.
- Tenore G, Palaia G, Del Vecchio A, Galanakis A, Romeo U (2013-10-24). "Focal epithelial hyperplasia (Heck's disease)". Annali di Stomatologia. 4 (Suppl 2): 43. PMC 3860189. PMID 24353818.
- Chakrabarti S, Chakrabarti PR, Agrawal D, Somanath S (2014). "Pseudoepitheliomatous hyperplasia: a clinical entity mistaken for squamous cell carcinoma". Journal of Cutaneous and Aesthetic Surgery. 7 (4): 232–234. doi:10.4103/0974-2077.150787. PMC 4338470. PMID 25722605.
- Lynch JM (2004). "Understanding Pseudoepitheliomatous Hyperplasia". Pathology Case Reviews. 9 (2): 36–45. doi:10.1097/01.pcr.0000117275.18471.5f. ISSN 1082-9784. S2CID 71497554.