Lymphoma in animals
Lymphoma (lymphosarcoma) in animals is a type of cancer defined by a proliferation of malignant lymphocytes within solid organs such as the lymph nodes, bone marrow, liver and spleen. The disease also may occur in the eye, skin, and gastrointestinal tract.

Lymphoma in dogs
Lymphoma is one of the most common malignant tumors to occur in dogs. The cause is genetic, but there are also suspected environmental factors involved,[1] including in one study an increased risk with the use of the herbicide 2,4-D.[2] This risk was not confirmed in another study.[3]
Breeds that are commonly affected include Boxer, Scottish Terrier, Basset Hound, Airedale Terrier, Chow Chow, German Shepherd, Poodle, St. Bernard, Bulldog, Beagle, Rottweiler[1] and Golden Retriever. The Golden Retriever is especially susceptible to developing lymphoma, with a lifetime risk of 1:8.[4]
Classification
The cancer is classified into low and high grade types. Classification is also based on location. The four location types are multicentric, mediastinal, gastrointestinal, and extranodal (involving the kidney, central nervous system, skin, heart, or eye). Multicentric lymphoma, the most common type (by greater than 80 percent),[5] is found in the lymph nodes, with or without involvement in the liver, spleen, or bone marrow. Mediastinal lymphoma occurs in the lymph nodes in the thorax and possibly the thymus. Gastrointestinal lymphoma occurs as either a solitary tumor or diffuse invasion of the stomach or intestines, with or without involvement in the surrounding lymph nodes, liver or spleen.[6] Classification is further based on involvement of B-lymphocytes or T-lymphocytes. Approximately 70 percent are B-cell lymphoma.[7] Cutaneous lymphoma can be classified as epitheliotropic (closely conforming to the epidermis) or non-epitheliotropic. The epitheliotropic form is typically of T-cell origin and is also called mycosis fungoides. The non-epitheliotropic form is typically of B-cell origin.[8]
Signs and symptoms
General signs and symptoms include depression, fever, weight loss, loss of appetite, loss of hair or fur and vomiting. Lymphoma is the most common cancerous cause of hypercalcemia (high blood calcium levels) in dogs.[9] It can lead to the above signs and symptoms plus increased water drinking, increased urination, and cardiac arrhythmias. Hypercalcemia in these cases is caused by secretion of parathyroid hormone-related protein.
Multicentric lymphoma presents as painless enlargement of the peripheral lymph nodes. This is seen in areas such as under the jaw, the armpits, the groin, and behind the knees. Enlargement of the liver and spleen causes the abdomen to distend. Mediastinal lymphoma can cause fluid to collect around the lungs, leading to coughing and difficulty breathing. Hypercalcemia is most commonly associated with this type.[10]
Gastrointestinal lymphoma causes vomiting, diarrhea, and melena (digested blood in the stool). Low serum albumin levels and hypercalcemia can also occur.[6]
Lymphoma of the skin is an uncommon occurrence. The epitheliotropic form typically appears as itchy inflammation of the skin progressing to nodules and plaques. The non-epitheliotropic form can have a wide variety of appearances, from a single lump to large areas of bruised, ulcerated, hairless skin.[8] The epitheliotropic form must be differentiated from similar appearing conditions such as pemphigus vulgaris, bullous pemphigoid, mycosis fungoides, and lupus erythematosus.[11]
Signs for lymphoma in other sites depend on the location. Central nervous system involvement can cause seizures or paralysis. Eye involvement, seen in 20 to 25 percent of cases,[12] can lead to glaucoma, uveitis, bleeding within the eye, retinal detachment, and blindness. Lymphoma in the bone marrow causes anemia, low platelet count, and low white blood cell count.
Diagnosis
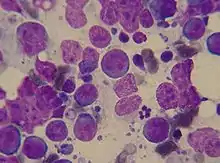
Biopsy of affected lymph nodes or organs confirms the diagnosis, although a needle aspiration of an affected lymph node can increase suspicion of the disease. X-rays, ultrasound and bone marrow biopsy reveal other locations of the cancer. There are now a range of blood tests that can be utilised to aid in the diagnosis of lymphoma. Flow cytometry detects antibodies linked to tumour cell surface antigens in fluid samples or cell suspensions.[13] Polymerase chain reaction (PCR) for antigen receptor rearrangements (PARR) identifies circulating tumour cells based on unique genetic sequences.[14] The canine Lymphoma Blood Test (cLBT) measures multiple circulating biomarkers and utilises a complex algorithm to diagnose lymphoma.[15] This test utilises the acute phase proteins (C-Reactive Protein and Haptoglobin). In combination with basic clinical symptoms, it gives in differential diagnosis the sensitivity 83.5% and specificity 77%.[16] The TK canine cancer panel is an indicator of general neoplastic disease.[17] The stage of the disease is important to treatment and prognosis. Certain blood tests have also been shown to be prognostic.
The stage of the disease is important to treatment and prognosis.
- Stage I - only one lymph node or lymphoid tissue in one organ involved.
- Stage II - lymph nodes in only one area of the body involved.
- Stage III - generalized lymph node involvement.
- Stage IV - any of the above with liver or spleen involvement.
- Stage V - any of the above with blood or bone marrow involvement.[1]
Each stage is divided into either substage a, those without systemic symptoms; or substage b, those with systemic symptoms such as fever, loss of appetite, weight loss, and fatigue.
Treatment
Due to the high risk of recurrence and ensuing problems, close monitoring of dogs undergoing chemotherapy is important. The same is true for dogs that have entered remission and ceased treatment. Monitoring for disease and remission/recurrence is usually performed by palpation of peripheral lymph nodes. This procedure detects gross changes in peripheral lymph nodes. Some of the blood tests used in diagnosing lymphoma also offer greater objectivity and provide an earlier warning of an animal coming out of remission.[15]
Complete cure is rare with lymphoma and treatment tends to be palliative, but long remission times are possible with chemotherapy. With effective protocols, average first remission times are 6 to 8 months. Second remissions are shorter and harder to accomplish. Average survival is 9 to 12 months. The most common treatment is a combination of cyclophosphamide, vincristine, prednisone, L-asparaginase, and doxorubicin.[1][18] Other chemotherapy drugs such as chlorambucil, lomustine (CCNU), cytosine arabinoside, and mitoxantrone are sometimes used in the treatment of lymphoma by themselves or in substitution for other drugs. In most cases, appropriate treatment protocols cause few side effects, but white blood cell counts must be monitored.
Allogeneic and autologous stem cell transplantations (as is commonly done in humans) have recently been shown to be a possible treatment option for dogs.[19] Most of the basic research on transplantation biology was generated in dogs. Current cure rates using stem cell therapy in dogs approximates that achieved in humans, 40-50%.
When cost is a factor, prednisone used alone can improve the symptoms dramatically, but it does not significantly affect the survival rate. The average survival times of dogs treated with prednisone and untreated dogs are both one to two months.[1] Using prednisone alone can cause the cancer to become resistant to other chemotherapy agents, so it should only be used if more aggressive treatment is not an option.
Isotretinoin can be used to treat cutaneous lymphoma.[8]
Prognosis
Untreated dogs have an average survival time of 60 days.[20] Lymphoma with a histologic high grade generally respond better to treatment but have shorter survival times than dogs with low grade lymphoma.[6] Dogs with B-lymphocyte tumors have a longer survival time than T-lymphocyte tumors.[1] Mediastinal lymphoma has a poorer prognosis than other types, especially those with hypercalcemia.[12] Clinical stage and substage have some prognostic value, with poorer prognosis associated with Stage V disease, and with substage b (clinical illness at time of presentation).[21]
Lymphoma in cats
Lymphoma is the most common malignancy diagnosed in cats.[22] Lymphoma in young cats occurs most frequently following infection with feline leukemia virus (FeLV) or to a lesser degree feline immunodeficiency virus (FIV). These cats tend to have involvement of lymph nodes, spine, or mediastinum. Cats with FeLV are 62 times more likely to develop lymphoma, and cats with both FeLV and FIV are 77 times more likely.[23] Younger cats tend to have T-cell lymphoma and older cats tend to have B-cell lymphoma.[24] Older cats tend to have gastrointestinal lymphoma without FeLV infection,[25] although tests more sensitive to low level FeLV infections and replication-defective FeLV have found that many of these cats have been previously exposed.[26] The same forms of lymphoma that are found in dogs also occur in cats, but gastrointestinal is the most common type. Lymphoma of the kidney is the most common kidney tumor in cats, and lymphoma is also the most common heart tumor.[1]
Classification
Gastrointestinal lymphoma is classified into low grade, intermediate grade, and high grade. Low grade types include lymphocytic and small cell lymphoma. High grade types include lymphoblastic, immunoblastic, and large cell lymphoma. Low grade lymphoma is only found in the small intestine, while high grade can commonly be found in the stomach.[27] The feline hepatic lymphoma is still poorly characterized, and it may be confused with lymphocytic portal hepatitis.[28]
Symptoms
Cats that develop lymphoma are much more likely to develop more severe symptoms than dogs. Whereas dogs often appear healthy initially except for swollen lymph nodes, cats will often be physically ill. The symptoms correspond closely to the location of the lymphoma. The most common sites for alimentary (gastrointestinal) lymphoma are, in decreasing frequency, the small intestine, the stomach, the junction of the ileum, cecum, and colon. Cats with the alimentary form of lymphoma often present with weight loss, rough hair coat, loss of appetite, vomiting and diarrhea, although vomiting and diarrhea are commonly absent as symptoms.[29] The tumor can also cause life-threatening blockage of the intestine. Cats with the mediastinal form often have respiratory distress and fluid in the thoracic cavity. If lymphoma develops in the kidney, the cat may have increased water consumption and increased urination. Lymphoma of the kidney presents as bilateral kidney enlargement and failure. If the lymphoma is located in the nose, the cat may have discharge from the nose and facial swelling. Lymphoma of the heart causes congestive heart failure, pericardial effusion, and cardiac arrhythmias. Ocular lymphoma in cats often presents as anterior uveitis (inflammation of the inside of the eye).[30] Cats who are also infected with FeLV often present with pale mucous membranes due to anemia. Anemia is a common problem in all cats with lymphoma, but hypercalcemia is rare.
Diagnosis is similar to dogs, except cats should be tested for FeLV and FIV. It is important to differentiate the alimentary form of lymphoma from inflammatory bowel disease because the signs are so similar in cats. A biopsy is necessary to do this.[31] One approach to differentiate inflammatory bowel disease from is to test the infiltrating lymphocytes for their monoclonal origin in lymphomas.[32]
Treatment and prognosis
Chemotherapy is the mainstay of treatment for lymphoma in cats. Most of the drugs used in dogs are used in cats, but the most common protocol uses cyclophosphamide, vincristine, and prednisone.[22] Gastrointestinal lymphoma has also commonly been treated with a combination of prednisolone and high dose pulse chlorambucil with success.[27] The white blood cell count must be monitored. Remission and survival times are comparable to dogs. Lower stage lymphoma has a better prognosis. Multicentric lymphoma has a better response to treatment than the gastrointestinal form, but infection with FeLV worsens the prognosis.[1]
About 75% of cats treated with chemotherapy for lymphoma go into remission. Unfortunately, after an initial remission, most cats experience a relapse, after which they have a median survival of 6 months. However, about one-third of cats treated with chemotherapy will survive more than 2 years after diagnosis; a small number of these cats may be cured of their disease. Untreated, most cats with lymphoma die within 4–6 weeks. Most cats tolerate their chemotherapy well, and fewer than 5% have severe side effects. Cats do not lose their fur from chemotherapy, though loss of whiskers is possible. Other side effects include low white blood cell count, vomiting, loss of appetite, diarrhea, or fatigue. These can typically be controlled well, and most cats have a good quality of life during treatment. If a cat relapses after attaining remission, the cat can be treated with different chemotherapy drugs to try for a second remission. The chances of a second remission are much lower than the chances of obtaining a first, and the second remission is often shorter than the first.
Lymphoma in ferrets
Lymphoma is common in ferrets and is the most common cancer in young ferrets. There is some evidence that a retrovirus may play a role in the development of lymphoma like in cats.[33] The most commonly affected tissues are the lymph nodes, spleen, liver, intestine, mediastinum, bone marrow, lung, and kidney.
In young ferrets, the disease progresses rapidly. The most common symptom is difficulty breathing caused by enlargement of the thymus.[34] Other symptoms include loss of appetite, weight loss, weakness, depression, and coughing. It can also masquerade as a chronic disease such as an upper respiratory infection or gastrointestinal disease. In older ferrets, lymphoma is usually chronic and can exhibit no symptoms for years.[35] Symptoms seen are the same as in young ferrets, plus splenomegaly, abdominal masses, and peripheral lymph node enlargement.
Diagnosis is through biopsy and X-rays. There may also be an increased lymphocyte count. Treatment includes surgery for solitary tumors, splenectomy (when the spleen is very large), and chemotherapy. The most common protocol uses prednisone, vincristine, and cyclophosphamide.[36] Doxorubicin is used in some cases. Chemotherapy in relatively healthy ferrets is tolerated very well, but possible side effects include loss of appetite, depression, weakness, vomiting, and loss of whiskers. The white blood cell count must be monitored. Prednisone used alone can work very well for weeks to months, but it may cause resistance to other chemotherapy agents. Alternative treatments include vitamin C and Pau d'Arco (a bark extract).[36]
The prognosis for lymphoma in ferrets depends on their health and the location of the cancer. Lymphoma in the mediastinum, spleen, skin, and peripheral lymph nodes has the best prognosis, while lymphoma in the intestine, liver, abdominal lymph nodes, and bone marrow has the worst.[36]
See also
References
- Morrison WB (1998). Cancer in Dogs and Cats (1st ed.). Williams and Wilkins. ISBN 0-683-06105-4.
- Zahm SH, Blair A (October 1992). "Pesticides and non-Hodgkin's lymphoma". Cancer Research. 52 (19 Suppl): 5485s–5488s. PMID 1394159.
- Kaneene JB, Miller R (June 1999). "Re-analysis of 2,4-D use and the occurrence of canine malignant lymphoma". Veterinary and Human Toxicology. 41 (3): 164–170. PMID 10349709.
- Modiano JF, Breen M, Burnett RC, Parker HG, Inusah S, Thomas R, et al. (July 2005). "Distinct B-cell and T-cell lymphoproliferative disease prevalence among dog breeds indicates heritable risk". Cancer Research. 65 (13): 5654–5661. doi:10.1158/0008-5472.CAN-04-4613. PMID 15994938.
- "Canine Malignant Lymphoma: Introduction". The Merck Veterinary Manual. 2006. Retrieved 2007-01-28.
- Lowe AD (July 2004). "Alimentary lymphosarcoma in a 4-year-old Labrador retriever". The Canadian Veterinary Journal. 45 (7): 610–612. PMC 548643. PMID 15317395.
- Simon D (2006). "Malignant lymphoma in the dog: Short and long term chemotherapy" (PDF). Proceedings of the North American Veterinary Conference. Archived from the original (PDF) on 2007-09-29. Retrieved 2007-01-28.
- Hoskins JD (May 2006). "Cutaneous paraneoplastic disease". DVM. Advanstar Communications: 6S–7S.
- Lucas P, Lacoste H, de Lorimier LP, Fan TM (May 2007). "Treating paraneoplastic hypercalcemia in dogs and cats". Veterinary Medicine. Advanstar Communications. 102 (5): 314–331.
- "Hypercalcemia of Malignancy". The Merck Veterinary Manual. 2006. Archived from the original on 24 May 2007. Retrieved 2007-01-28.
- Bhang DH, Choi US, Kim MK, Choi EH, Kang MS, Hwang CY, et al. (March 2006). "Epitheliotropic cutaneous lymphoma (mycosis fungoides) in a dog". Journal of Veterinary Science. 7 (1): 97–99. doi:10.4142/jvs.2006.7.1.97. PMC 3242097. PMID 16434861.
- Ogilvie GK (2004). "Canine Lymphoma: Protocols For 2004". Proceedings of the 29th World Congress of the World Small Animal Veterinary Association. Retrieved 2006-08-20.
- Reggeti F, Bienzle D (January 2011). "Flow cytometry in veterinary oncology". Veterinary Pathology. 48 (1): 223–35. doi:10.1177/0300985810379435. PMID 20826845. S2CID 8437347.
- Lana SE, Jackson TL, Burnett RC, Morley PS, Avery AC (2006). "Utility of polymerase chain reaction for analysis of antigen receptor rearrangement in staging and predicting prognosis in dogs with lymphoma". Journal of Veterinary Internal Medicine. 20 (2): 329–34. doi:10.1892/0891-6640(2006)20[329:uopcrf]2.0.co;2. PMID 16594590.
- Alexandrakis I, Tuli R, Ractliffe SC, Tappin SW, Foale RD, Roos A, Slater KJ (March 2017). "Utility of a multiple serum biomarker test to monitor remission status and relapse in dogs with lymphoma undergoing treatment with chemotherapy". Veterinary and Comparative Oncology. 15 (1): 6–17. doi:10.1111/vco.12123. PMID 25319380. S2CID 206346140.
- Mirkes EM, Alexandrakis I, Slater K, Tuli R, Gorban AN (October 2014). "Computational diagnosis and risk evaluation for canine lymphoma". Computers in Biology and Medicine. 53: 279–290. arXiv:1305.4942. doi:10.1016/j.compbiomed.2014.08.006. PMID 25194257. S2CID 6029946.
- Selting KA, Sharp CR, Ringold R, Knouse J (December 2015). "Serum thymidine kinase 1 and C-reactive protein as biomarkers for screening clinically healthy dogs for occult disease". Veterinary and Comparative Oncology. 13 (4): 373–84. doi:10.1111/vco.12052. PMID 23859156.
- "5 Tips for Treating and Beating Canine Lymphoma | petMD". www.petmd.com. Retrieved 2019-05-29.
- Lupu M, Sullivan EW, Westfall TE, Little MT, Weigler BJ, Moore PF, et al. (March 2006). "Use of multigeneration-family molecular dog leukocyte antigen typing to select a hematopoietic cell transplant donor for a dog with T-cell lymphoma". Journal of the American Veterinary Medical Association. 228 (5): 728–732. doi:10.2460/javma.228.5.728. PMID 16506937.
- Siedlecki CT, Kass PH, Jakubiak MJ, Dank G, Lyons J, Kent MS (January 2006). "Evaluation of an actinomycin-D-containing combination chemotherapy protocol with extended maintenance therapy for canine lymphoma". The Canadian Veterinary Journal. 47 (1): 52–59. PMC 1316122. PMID 16536229.
- Withrow,2001
- "Feline Leukemia Virus and Related Diseases: Introduction". The Merck Veterinary Manual. 2006. Retrieved 2007-01-28.
- Ettinger SJ, Feldman EC (1995). Textbook of Veterinary Internal Medicine (4th ed.). W.B. Saunders Company. ISBN 0-7216-6795-3.
- Seo KW, Choi US, Bae BK, Park MS, Hwang CY, Kim DY, Youn HY (June 2006). "Mediastinal lymphoma in a young Turkish Angora cat". Journal of Veterinary Science. 7 (2): 199–201. doi:10.4142/jvs.2006.7.2.199. PMC 3242115. PMID 16645348.
- "Gastrointestinal Neoplasia". The Merck Veterinary Manual. 2006. Retrieved 2007-01-28.
- Richter KP (2006). "Feline gastrointestinal lymphoma" (PDF). Proceedings of the North American Veterinary Conference. Archived from the original (PDF) on 2007-09-29. Retrieved 2007-01-28.
- Matz ME (January 2007). "Chronic Vomiting in a Cat". Clinician's Brief. North American Veterinary Conference. 5 (1): 29–31.
- Sebastian K, Smedley RC, Bartel A, Kiupel M (February 2023). "Patterns of Lymphocytic Infiltrates Can Differentiate Feline Hepatic Lymphoma from Lymphocytic Portal Hepatitis". Veterinary Sciences. 10 (2): 127. doi:10.3390/vetsci10020127. PMC 9960306. PMID 36851431.
- Gaschen F (2006). "Small Intestinal Diarrhea: Causes and Treatment" (PDF). Proceedings of the 31st World Congress of the World Small Animal Veterinary Association. Retrieved 2007-01-28.
- van der Woerdt A (June 2007). "Iris Nodule in a Cat". Clinician's Brief. North American Veterinary Conference. 5 (6): 7–8.
- Evans SE, Bonczynski JJ, Broussard JD, Han E, Baer KE (November 2006). "Comparison of endoscopic and full-thickness biopsy specimens for diagnosis of inflammatory bowel disease and alimentary tract lymphoma in cats". Journal of the American Veterinary Medical Association. 229 (9): 1447–1450. doi:10.2460/javma.229.9.1447. PMID 17078807.
- Weiss AT, Klopfleisch R, Gruber AD (2010). "T-cell receptor γ chain variable and joining region genes of subgroup 1 are clonally rearranged in feline B- and T-cell lymphoma". Journal of Comparative Pathology. 144 (2–3): 123–134. doi:10.1016/j.jcpa.2010.08.001. PMID 20846665.
- Hernández-Divers SM (2005). "Ferret Diseases". Proceedings of the 30th World Congress of the World Small Animal Veterinary Association. Retrieved 2007-01-28.
- Mayer J (2006). "Update on ferret lymphoma" (PDF). Proceedings of the North American Veterinary Conference. Retrieved 2007-01-28.
- "Ferret Neoplasia". The Merck Veterinary Manual. 2006. Retrieved 2007-01-01.
- Hillyer EV, Quesenberry KE (1997). Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery (1st ed.). W.B. Saunders Company. ISBN 0-7216-4023-0.