HLA-DRB1
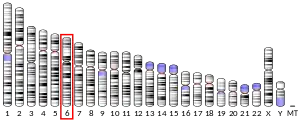
HLA class II histocompatibility antigen, DRB1 beta chain is a protein that in humans is encoded by the HLA-DRB1 gene.[3] DRB1 encodes the most prevalent beta subunit of HLA-DR. DRB1 alleles, especially those encoding amino acid sequence changes at positions 11 and 13, are associated risk of rheumatoid arthritis.[4][5]
Function
The protein encoded by this gene belongs to the HLA class II beta chain paralogues. The class II molecule is a heterodimer consisting of an alpha (DRA) and a beta chain (DRB), both anchored in the membrane. It plays a central role in the immune system by presenting peptides derived from extracellular proteins to T helper cells. Class II molecules are constitutively expressed in professional antigen-presenting cells (APC: B lymphocytes, dendritic cells, macrophages),[3] and could be induced in non-professional APCs.
There is evidence it is associated with reduced severity of COVID-19 disease.[6]
Gene structure and polymorphisms
The beta chain is approximately 26-28 kDa. It is encoded by 6 exons, exon one encodes the leader peptide, exons 2 and 3 encode the two extracellular domains, exon 4 encodes the transmembrane domain and exon 5 encodes the cytoplasmic tail. Within the DR molecule the beta chain contains all the polymorphisms specifying the peptide binding specificities. Hundreds of DRB1 alleles have been described and typing for these polymorphisms is routinely done for bone marrow and kidney transplantation.[3]
Gene expression
DRB1 is expressed at a level five times higher than its paralogues DRB3, DRB4 and DRB5. DRB1 is present in all individuals. Allelic variants of DRB1 are linked with either none or one of the genes DRB3, DRB4 and DRB5. There are 5 related pseudogenes: DRB2, DRB6, DRB7, DRB8 and DRB9.[3]
Prevalence of the HLA-DRB1*10:01 allele was greatly increased in people with anti-IgLON5 disease.[7]
See also
References
- ENSG00000206240, ENSG00000229074, ENSG00000196126, ENSG00000206306, ENSG00000228080 GRCh38: Ensembl release 89: ENSG00000236884, ENSG00000206240, ENSG00000229074, ENSG00000196126, ENSG00000206306, ENSG00000228080 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Entrez Gene: HLA-DRB1 major histocompatibility complex, class II, DR beta 1".
- Gregersen PK, Silver J, Winchester RJ (November 1987). "The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis". Arthritis and Rheumatism. 30 (11): 1205–13. doi:10.1002/art.1780301102. PMID 2446635.
- Raychaudhuri, S; Sandor, C; Stahl, EA; Freudenberg, J; Lee, HS; Jia, X; Alfredsson, L; Padyukov, L; Klareskog, L; Worthington, J; Siminovitch, KA; Bae, SC; Plenge, RM; Gregersen, PK; de Bakker, PI (29 January 2012). "Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis". Nature Genetics. 44 (3): 291–6. doi:10.1038/ng.1076. PMC 3288335. PMID 22286218.
- Langton, David J.; Bourke, Stephen C.; Lie, Benedicte A.; Reiff, Gabrielle; Natu, Shonali; Darlay, Rebecca; Burn, John; Echevarria, Carlos (2021-05-04). "The influence of HLA genotype on the severity of COVID‐19 infection". HLA. 98 (1): 14–22. doi:10.1111/tan.14284. ISSN 2059-2302. PMC 8251294. PMID 33896121.
- Gaig C, Graus F, Compta Y, Högl B, Bataller L, Brüggemann N, Giordana C, Heidbreder A, Kotschet K, Lewerenz J, Macher S, Martí MJ, Montojo T, Pérez-Pérez J, Puertas I, Seitz C, Simabukuro M, Téllez N, Wandinger KP, Iranzo A, Ercilla G, Sabater L, Santamaría J, Dalmau J (May 2017). "Clinical manifestations of the anti-IgLON5 disease". Neurology. 88 (18): 1736–1743. doi:10.1212/WNL.0000000000003887. PMC 5409845. PMID 28381508.
Further reading
- Turesson C, Matteson EL (January 2006). "Genetics of rheumatoid arthritis". Mayo Clinic Proceedings. 81 (1): 94–101. doi:10.4065/81.1.94. PMID 16438485.
- Ahmad T, Marshall SE, Jewell D (June 2006). "Genetics of inflammatory bowel disease: the role of the HLA complex". World Journal of Gastroenterology. 12 (23): 3628–35. doi:10.3748/wjg.v12.i23.3628. PMC 4087453. PMID 16773677.
- Schmidt H, Williamson D, Ashley-Koch A (May 2007). "HLA-DR15 haplotype and multiple sclerosis: a HuGE review". American Journal of Epidemiology. 165 (10): 1097–109. doi:10.1093/aje/kwk118. PMID 17329717.

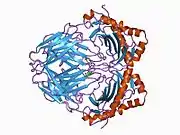



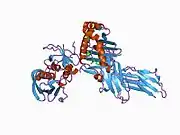
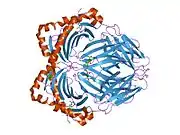
















![2ipk: Crystal Structure of the MHC Class II Molecule HLA-DR1 in Complex with the Fluorogenic Peptide, AcPKXVKQNTLKLAT (X=3-[5-(dimethylamino)-1,3-dioxo-1,3-dihydro-2H-isoindol-2-yl]-L-alanine) and the Superantigen, SEC3 Variant 3B2](../I/PDB_2ipk_EBI.jpg.webp)