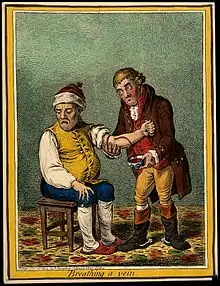
Heroic medicine
Heroic medicine, also referred to as heroic depletion theory, was a therapeutic method advocating for rigorous treatment of bloodletting, purging, and sweating to shock the body back to health after an illness caused by a humoral imbalance. Rising to the front of orthodox medical practice in the "Age of Heroic Medicine" (1780–1850),[2] it fell out of favor in the mid-19th century as gentler treatments were shown to be more effective and the idea of palliative treatment began to develop.[3]
History
Pockets of medical methodology that can be classified as "heroic" appear in the early 17th century with Parisian physician Guy Patin and French anatomist Jean Riolan the Younger. Patin, nicknamed "Le Grand Saigneur" (the Grand Bloodletter), was infamous for his rigorous procedure plans, which included intensive courses of bloodletting and application of senna. Because heroic medicine used popular techniques, it is difficult to absolutely classify a healer's therapeutic epistemology as heroic. Intensive bloodletting treatments can be identified throughout American history, with William Douglass in Massachusetts advocating for a heroic treatment plan in the early 18th century.[4] While there were practitioners here and there who were particularly eager to perform aggressive treatment, heroic medicine did not become a concentrated school of thought until later in the 18th century.
Many associate Benjamin Rush with an abrupt acceptance of heroic techniques into the realm of mainstream medicine, especially in America. Founding father, creator of University of Pennsylvania’s medical school, and known as the "American Hippocrates," Rush was well respected and revered in the medical field. The Philadelphia Yellow Fever outbreak in 1793 is looked upon as a major event in the merging of heroic medicine into the course of best practices in the medical profession.[5] Much of the city was left incapacitated by the rampant epidemic. As healers fled the city, Rush bravely remained to treat people, and ultimately himself, with drastic regimens of intensive bloodlettings and purgatives. He taught many students who then carried the tradition to other parts of the United States. Varied in its influence, heroic medicine was particularly concentrated around Pennsylvania and spread into other locations. The term "heroic medicine" was coined later in the mid-19th century to describe extreme treatment.[4]
Heroic medicine was used to treat George Washington on his deathbed in 1799. He was bled repeatedly and given Mercury(I) chloride (calomel) and several blisters of cantharidin to induce sweating. Washington died shortly after receiving this rigorous heroic treatment.[6][7][8][9][10]
Heroic medicine was very much in the hands of the professional, as the invasive interventions involved were beyond the capabilities of rustic practitioners. Symptoms were not regarded as the body's attempt to fight the disease, but were considered a complication that would exacerbate the patient's condition and do further harm. Practitioners believed that a fever should be suppressed and any drugs used should be powerful and given in large dosages. Under this onslaught, domestic medicine dwindled in importance; even treatments that had been found effective in the past were relegated to the realms of old-fashioned folk medicine.[11]
Barbara Ehrenreich and Deirdre English write that heroic medicine was created to justify medical billing. Traditional healing techniques were mostly practiced by women within a non-commercial family or village setting. As male doctors suppressed these techniques, they found it difficult to quantify various "amounts" of healing to charge for, and difficult to convince patients to pay for it. Heroic medicine helped convince patients the doctor had something obvious and tangible to sell.[12]
Practices
Heroic medicine does not have a definitive start date, as its treatments themselves were not new to the field of medicine. Bloodletting, purging, and sweating are cemented firmly in medical tradition back to the advent of humoral theory in the time of Hippocrates and Galen.[13] With hopes of rebalancing the body's delicate homeostasis of four humors – black bile, yellow bile, phlegm, and blood – the careful manipulation of bodily discharge, like bleeding and evacuation, was believed to nudge the body back to its healthy, natural state. The physician's role was always to monitor the path of the body's humoral levels back to normal.[5]
Heroic medicine takes this methodology to the extreme, draining significant volumes of blood and ordering intensive regimens of evacuation. It was not uncommon for physicians to strive to drain up to 80 percent of a patient's blood volume.[5] Likewise, dramatic evacuations, both by pharmacological emetics and laxatives, induced the forceful removal of bodily fluid. Commonly used emetics include senna and tartar emetic. General intestinal cleansing was instigated by massive doses of calomel, to the point of acute mercury poisoning. Sweating was also induced using blisters of cantharidin and diaphoretic.[4]
Fall of heroic medicine
Heroic medicine became less favoured with the rise of safer treatment methods such as hydrotherapy and homeopathy. Even during its heyday, heroic medicine faced criticism from physicians and alternative medicine healers, who pushed for more natural cures.[14]
While it is easy to discuss and question the ethical implications of such a severe course of treatment, it is important to remember that in that time period physicians were operating under their best understanding of the body and its physiology. There were dissenting voices at the time, but heroic medicine remained an important, legitimate part of the medical tradition in that era.[4]
See also
References
- "English Caricature: Heroic Medicine--Bloodletting, Emetics, and Laxatives". exhibits.hsl.virginia.edi. Retrieved December 22, 2022.
- Singh, Simon; Ernst, Edzard (2008). Trick Or Treatment: The Undeniable Facts about Alternative Medicine. W. W. Norton & Company. p. 108. ISBN 978-0-393-06661-6.
- Flint, August (1874) Essays on Conservative Medicine
- Sullivan, R. B. (1994). "Sanguine practices: A historical and historiographic reconsideration of heroic therapy in the age of Rush". Bulletin of the History of Medicine. 68 (2): 211–34. PMID 8049598.
- Lindemann, Mary (2010). Medicine and Society in Early Modern Europe. Cambridge: Cambridge. p. 117. ISBN 978-0-521-73256-7.
- Stavrakis, P (1997). "Heroic medicine, bloodletting, and the sad fate of George Washington". Maryland Medical Journal. 46 (10): 539–40. PMID 9392943.
- Cohen, Ben (2005). "The Death of George Washington (1732–99) and the History of Cynanche". Journal of Medical Biography. 13 (4): 225–31. doi:10.1177/096777200501300410. PMID 16244717. S2CID 2766668.
- Schmidt, P. J. (2002). "Transfuse George Washington!". Transfusion. 42 (2): 275–7. doi:10.1046/j.1537-2995.2002.00033.x. PMID 11896346. S2CID 37897549.
- Howard Markel. "Dec. 14, 1799: The excruciating final hours of President George Washington". www.pbs.org.
- Cheatham, M. L. (2008). "The death of George Washington: An end to the controversy?". The American Surgeon. 74 (8): 770–4. doi:10.1177/000313480807400821. PMID 18705585. S2CID 31457820.
- Lyng, Stephen (1990). Holistic Health and Biomedical Medicine: A Countersystem Analysis. SUNY Press. pp. 175–9. ISBN 978-0-7914-0256-6.
- Ehrenreich, Barbara; English, Deirdre (2005). For her Own Good. Anchor Books. pp. 49–51. ISBN 1400078008.
- Bynum, W. E. (1996). Scientific Practice of Medicine in the Nineteenth Century. Cambridge: Cambridge University Press. p. 18. ISBN 0-521-25109-5.
- Whorton, James (2002). Nature Cures: The History of Alternative Medicine in America. Oxford University Press.