Lower respiratory tract infection
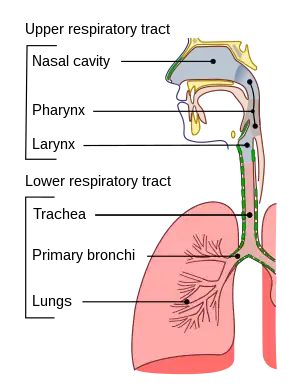
Lower respiratory tract infection (LRTI) is a term often used as a synonym for pneumonia but can also be applied to other types of infection including lung abscess and acute bronchitis. Symptoms include shortness of breath, weakness, fever, coughing and fatigue.[3] A routine chest X-ray is not always necessary for people who have symptoms of a lower respiratory tract infection.[4]
| Lower respiratory tract infection | |
|---|---|
 | |
| Conducting passages | |
| Specialty | Pulmonology |
| Frequency | 291 million (2015)[1] |
| Deaths | 2.74 million (2015)[2] |
Influenza affects both the upper and lower respiratory tracts.
Antibiotics are the first line treatment for pneumonia; however, they are neither effective nor indicated for parasitic or viral infections. Acute bronchitis typically resolves on its own with time.
In 2015 there were about 291 million cases.[1] These resulted in 2.74 million deaths down from 3.4 million deaths in 1990.[5][2] This was 4.8% of all deaths in 2013.[5]
Bronchitis
Bronchitis describes the swelling or inflammation of the[6] bronchial tubes. Additionally, bronchitis is described as either acute or chronic depending on its presentation and is also further described by the causative agent. Acute bronchitis can be defined as acute bacterial or viral infection of the larger airways in healthy patients with no history of recurrent disease.[7] It affects over 40 adults per 1000 each year and consists of transient inflammation of the major bronchi and trachea.[8] Most often it is caused by viral infection and hence antibiotic therapy is not indicated in immunocompetent individuals.[9][6] Viral bronchitis can sometimes be treated using antiviral medications depending on the virus causing the infection, and medications such as anti-inflammatory drugs and expectorants can help mitigate the symptoms.[10][6] Treatment of acute bronchitis with antibiotics is common but controversial as their use has only moderate benefit weighted against potential side effects (nausea and vomiting), increased resistance, and cost of treatment in a self-limiting condition.[8][11] Beta2 agonists are sometimes used to relieve the cough associated with acute bronchitis. In a recent systematic review it was found there was no evidence to support their use.[6]
Acute exacerbations of chronic bronchitis (AECB) are frequently due to non-infective causes along with viral ones. 50% of patients are colonised with Haemophilus influenzae, Streptococcus pneumoniae, or Moraxella catarrhalis.[7] Antibiotics have only been shown to be effective if all three of the following symptoms are present: increased dyspnea, increased sputum volume, and purulence. In these cases, 500 mg of amoxicillin orally, every 8 hours for 5 days or 100 mg doxycycline orally for 5 days should be used.[7]
Pneumonia
Pneumonia occurs in a variety of situations and treatment must vary according to the situation.[10] It is classified as either community or hospital acquired depending on where the patient contracted the infection. It is life-threatening in the elderly or those who are immunocompromised.[12][13] The most common treatment is antibiotics and these vary in their adverse effects and their effectiveness.[12][14] Pneumonia is also the leading cause of death in children less than five years of age in low income countries.[14] The most common cause of pneumonia is pneumococcal bacteria, Streptococcus pneumoniae accounts for 2/3 of bacteremic pneumonias.[15] Invasive pneumococcal pneumonia has a mortality rate of around 20%.[13] For optimal management of a pneumonia patient, the following must be assessed: pneumonia severity (including treatment location, e.g., home, hospital or intensive care), identification of causative organism, analgesia of chest pain, the need for supplemental oxygen, physiotherapy, hydration, bronchodilators and possible complications of emphysema or lung abscess.[16]
Causes


Typical bacterial Infections:
Atypical bacterial Infections:
Prevention
Vaccination helps prevent bronchopneumonia, mostly against influenza viruses, adenoviruses, measles, rubella, streptococcus pneumoniae, haemophilus influenzae, diphtheria, bacillus anthracis, chickenpox, and bordetella pertussis.[18] Specifically for the children with low serum retinol or who are suffering from malnutrition, vitamin A supplements are recommended as a preventive measure against acute LRTI.[19]
Treatment
Antibiotics do not help the many lower respiratory infections which are caused by parasites or viruses. While acute bronchitis often does not require antibiotic therapy, antibiotics can be given to patients with acute exacerbations of chronic bronchitis.[20] The indications for treatment are increased dyspnoea, and an increase in the volume or purulence of the sputum.[21] The treatment of bacterial pneumonia is selected by considering the age of the patient, the severity of the illness and the presence of underlying disease. A systematic review of 32 randomised controlled trials with 6,078 participants with acute respiratory infections compared procalcitonin (a blood marker for bacterial infections) to guide the initiation and duration of antibiotic treatment, against no use of procalcitonin. Among 3,336 people receiving procalcitonin-guided antibiotic therapy, there were 236 deaths, compared to 336 deaths out 3,372 participants who did not. Procalcitonin-guided antibiotic therapy also reduced the antibiotic use duration by 2.4 days, and there were fewer antibiotic side effects. This means that procalcitonin is useful for guiding whether to use antibiotics for acute respiratory infections and the duration of the antibiotic.[22] Amoxicillin and doxycycline are suitable for many of the lower respiratory tract infections seen in general practice.[20] Another cochrane review suggests that new studies are needed to confirm that azithromycin may lead to less treatment failure and lower side effects than amoxycillin.[23] In the other hand, there is no sufficient evidence to consider the antibiotics as a prophylaxis for the high risk children under 12 years.[24]
Oxygen supplementation is often recommended for people with severe lower respiratory tract infections.[25] Oxygen can be provided in a non-invasive manner using nasal prongs, face masks, a head box or hood, a nasal catheter, or a nasopharyngeal catheter.[25] For children younger than 15 years old, nasopharyngel catheters or nasal prongs are recommended over a face mask or head box.[25] A Cochrane review in 2014 presented a summary to identify children complaining of severe LRTI, however; further research is required to determine the effectiveness of supplemental oxygen and the best delivery method.[25]
Epidemiology
Lower respiratory infectious disease is the fifth-leading cause of death and the combined leading infectious cause of death, being responsible for 2.74 million deaths worldwide.[26] This is generally similar to estimates in the 2010 Global Burden of Disease study.[27] This total only accounts for Streptococcus pneumoniae and Haemophilus influenzae infections and does not account for atypical or nosocomial causes of lower respiratory disease, therefore underestimating total disease burden.
Society and culture
Lower respiratory tract infections place a considerable strain on the health budget and are generally more serious than upper respiratory infections.
Workplace burdens arise from the acquisition of a lower respiratory tract infection, with factors such as total per person expenditures and total medical service utilisation demonstrated as greater among individuals experiencing a lower respiratory tract infection.[28]
Pan-national data collection indicates that childhood nutrition plays a significant role in determining the acquisition of a lower respiratory tract infection, with the promotion of the implementation of nutrition program, and policy guidelines in affected countries.[26]
References
- GBD 2015 Disease Injury Incidence Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|author1=has generic name (help) - GBD 2015 Mortality Causes of Death Collaborators (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|author1=has generic name (help) - Antibiotic Expert Group (2014). Therapeutic Guidelines: Antibiotic (15th ed.). Therapeutic Guidelines Limited. ISBN 9780992527211.
- Cao, Amy Millicent Y.; Choy, Joleen P.; Mohanakrishnan, Lakshmi Narayana; Bain, Roger F.; van Driel, Mieke L. (2013-12-26). "Chest radiographs for acute lower respiratory tract infections". Cochrane Database of Systematic Reviews. 2013 (12): CD009119. doi:10.1002/14651858.CD009119.pub2. ISSN 1469-493X. PMC 6464822. PMID 24369343.
- GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013" (PDF). Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. hdl:10379/13075. PMC 4340604. PMID 25530442.
{{cite journal}}:|author1=has generic name (help) - Becker LA, Hom J, Villasis-Keever M, van der Wouden JC (September 2015). "Beta2-agonists for acute cough or a clinical diagnosis of acute bronchitis". The Cochrane Database of Systematic Reviews. 2015 (9): CD001726. doi:10.1002/14651858.CD001726.pub5. PMC 7078572. PMID 26333656.
- Antibiotic Expert Group. Therapeutic guidelines: Antibiotic. 13th ed. North Melbourne: Therapeutic Guidelines; 2006.
- Wark P (July 2015). "Bronchitis (acute)". BMJ Clinical Evidence. 2015. PMC 4505629. PMID 26186368.
- Therapeutic guidelines : respiratory. 2nd ed: North Melbourne : Therapeutic Guidelines Limited, 2000.
- Integrated pharmacology / Clive Page ... [et al.]. 2nd ed: Edinburgh : Mosby, 2002.
- Smith, SM; Fahey, T; Smucny, J; Becker, LA (19 June 2017). "Antibiotics for acute bronchitis". The Cochrane Database of Systematic Reviews. 2017 (6): CD000245. doi:10.1002/14651858.CD000245.pub4. PMC 6481481. PMID 28626858.
- Pakhale S, Mulpuru S, Verheij TJ, Kochen MM, Rohde GG, Bjerre LM (October 2014). "Antibiotics for community-acquired pneumonia in adult outpatients". The Cochrane Database of Systematic Reviews. 2014 (10): CD002109. doi:10.1002/14651858.CD002109.pub4. PMC 7078574. PMID 25300166.
- Moberley S, Holden J, Tatham DP, Andrews RM (January 2013). "Vaccines for preventing pneumococcal infection in adults". The Cochrane Database of Systematic Reviews. 2013 (1): CD000422. doi:10.1002/14651858.CD000422.pub3. PMC 7045867. PMID 23440780.
- Lodha R, Kabra SK, Pandey RM (June 2013). "Antibiotics for community-acquired pneumonia in children". The Cochrane Database of Systematic Reviews. 2013 (6): CD004874. doi:10.1002/14651858.CD004874.pub4. PMC 7017636. PMID 23733365.
- The Merck manual of diagnosis and therapy. 17th ed / Mark H. Beers and Robert Berkow ed: Whitehouse Station, N.J. : Merck Research Laboratories, 1999.
- Kumar Pius, Prince Sree; Alexis, Anitha; P, Suresh Kumar; Ganesan, Manivel (2017). "Diagnosis of Sputum Culture Positive Organisms and Their Antimicrobial Sensitivity Profile in a Tertiary Care Centre- Kanyakumari". Journal of Evidence Based Medicine and Healthcare. 4 (4): 168–171. doi:10.18410/jebmh/2017/33.
- "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Read R, Verheij TJ (November 2011). "Guidelines for the management of adult lower respiratory tract infections--full version". Clinical Microbiology and Infection. 17 (Suppl 6): E1–59. doi:10.1111/j.1469-0691.2011.03672.x. PMC 7128977. PMID 21951385.
- Chen, Hengxi; Zhuo, Qi; Yuan, Wei; Wang, Juan; Wu, Taixiang (23 January 2008). "Vitamin A for preventing acute lower respiratory tract infections in children up to seven years of age". Cochrane Database of Systematic Reviews (1): CD006090. doi:10.1002/14651858.CD006090.pub2. PMID 18254093.
- Ball P, Baquero F, Cars O, File T, Garau J, Klugman K, Low DE, Rubinstein E, Wise R (January 2002). "Antibiotic therapy of community respiratory tract infections: strategies for optimal outcomes and minimized resistance emergence". The Journal of Antimicrobial Chemotherapy. 49 (1): 31–40. doi:10.1093/jac/49.1.31. PMID 11751764.
- Woodhead M, Blasi F, Ewig S, Huchon G, Ieven M, Leven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Verheij TJ (December 2005). "Guidelines for the management of adult lower respiratory tract infections". The European Respiratory Journal. 26 (6): 1138–80. doi:10.1183/09031936.05.00055705. PMID 16319346.
- Schuetz, Philipp; Wirz, Yannick; Sager, Ramon; Christ-Crain, Mirjam; Stolz, Daiana; Tamm, Michael; Bouadma, Lila; Luyt, Charles E; Wolff, Michel; Chastre, Jean; Tubach, Florence; Kristoffersen, Kristina B; Burkhardt, Olaf; Welte, Tobias; Schroeder, Stefan; Nobre, Vandack; Wei, Long; Bucher, Heiner C C; Bhatnagar, Neera; Annane, Djillali; Reinhart, Konrad; Branche, Angela; Damas, Pierre; Nijsten, Maarten; de Lange, Dylan W; Deliberato, Rodrigo O; Lima, Stella SS; Maravić-Stojković, Vera; Verduri, Alessia; Cao, Bin; Shehabi, Yahya; Beishuizen, Albertus; Jensen, Jens-Ulrik S; Corti, Caspar; Van Oers, Jos A; Falsey, Ann R; de Jong, Evelien; Oliveira, Carolina F; Beghe, Bianca; Briel, Matthias; Mueller, Beat (12 October 2017). "Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections". Cochrane Database of Systematic Reviews. 10 (5): CD007498. doi:10.1002/14651858.CD007498.pub3. PMC 6485408. PMID 29025194.
- Laopaiboon, Malinee; Panpanich, Ratana; Swa Mya, Kyaw (8 March 2015). "Azithromycin for acute lower respiratory tract infections". Cochrane Database of Systematic Reviews. 2015 (3): CD001954. doi:10.1002/14651858.CD001954.pub4. PMC 6956663. PMID 25749735.
- Onakpoya, Igho J; Hayward, Gail; Heneghan, Carl J (26 September 2015). "Antibiotics for preventing lower respiratory tract infections in high-risk children aged 12 years and under". Cochrane Database of Systematic Reviews (9): CD011530. doi:10.1002/14651858.CD011530.pub2. PMID 26408070.
- Rojas-Reyes, Maria Ximena; Granados Rugeles, Claudia; Charry-Anzola, Laura Patricia (10 December 2014). "Oxygen therapy for lower respiratory tract infections in children between 3 months and 15 years of age". Cochrane Database of Systematic Reviews. 2014 (12): CD005975. doi:10.1002/14651858.CD005975.pub3. PMC 6464960. PMID 25493690.
- GBD 2015 LRI Collaborators (November 2017). "Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015". The Lancet. Infectious Diseases. 17 (11): 1133–1161. doi:10.1016/S1473-3099(17)30396-1. PMC 5666185. PMID 28843578.
{{cite journal}}:|author1=has generic name (help) - Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- Chen Y, Shan X, Zhao J, Han X, Tian S, Chen F, Su X, Sun Y, Huang L, Grundmann H, Wang H, Han L (November 2017). "Predicting nosocomial lower respiratory tract infections by a risk index based system". Scientific Reports. 7 (1): 15933. Bibcode:2017NatSR...715933C. doi:10.1038/s41598-017-15765-z. PMC 5698311. PMID 29162852.