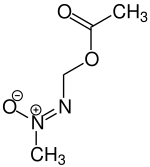
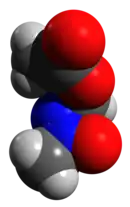
Methylazoxymethanol acetate
Methylazoxymethanol acetate, MAM, is a neurotoxin which reduces DNA synthesis[1] used in making animal models of neurological diseases including schizophrenia[2] and epilepsy.[3] MAM is found in cycad seeds, and causes zamia staggers. It selectively targets neuroblasts in the central nervous system. In rats, administration of MAM affects structures in the brain which are developing most quickly.[2] It is an acetate of methylazoxymethanol.
| |||
| Names | |||
|---|---|---|---|
| IUPAC name
(Z)-acetyloxymethylimino-methyl-oxidoazanium | |||
| Preferred IUPAC name
[(Z)-methyl-ONN-azoxy]methyl acetate | |||
| Other names
MAM | |||
| Identifiers | |||
3D model (JSmol) |
|||
| ChEBI | |||
| ChemSpider | |||
| ECHA InfoCard | 100.008.879 | ||
| EC Number |
| ||
| KEGG | |||
| MeSH | D008746 | ||
PubChem CID |
|||
| UNII | |||
CompTox Dashboard (EPA) |
|||
| |||
| |||
| Properties | |||
| C4H8N2O3 | |||
| Molar mass | 132.11792 | ||
| Hazards | |||
| GHS labelling: | |||
 | |||
| Danger | |||
| H350, H360D | |||
| P201, P202, P281, P308+P313, P405, P501 | |||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
Infobox references | |||
MAM animal models
Schizophrenia
In rat models, the specific effect of MAM on neural development depends on the gestational age of the subject. At the seventeenth gestational day (GD17), administration of MAM produces behavioral and histopathological patterns found in schizophrenia.[2] The molecular mechanism behind this model is not fully known.[4] Methylazoxymethanol acetate administered at GD17 reduces the thickness of the hippocampus and the thalamus. The locomotor effects of amphetamines and the spontaneous firing rate of dopaminergic neurons in the ventral tegmental area are increased. In alternating maze tests, GD17 MAM rats quickly learned the first rule, but took longer to accommodate to alterations to the rule; this is thought to indicate deficits in working spatial memory, which is also impaired in schizophrenia.[2] Another study found that mice whom methylazoxy-methanol acetate was administered on 16th gestational day, but not those whom it was adminitred on GD17 showed decreased parvalbumin expression in hippocampus and prefrontal cortex, and schizophrenia-like characteristics. Mice whom MAM was administered on GD16 also exhibited reduced size of hippocampus and thinning of the prefrontal cortex. PFC-dependent cognitive deficits were shown only in male MAM-treated mice.[5]
Epilepsy
Exposure to MAM before birth increases susceptibility to epileptic seizures caused by flurothyl.[3] Prenatal MAM exposure in rats results in a model of brain malformation. In some MAM animals, video-EEG monitoring has documented the presence of spontaneous electrographic seizure activity [6] In some epilepsy rat models, MAM is administered at the fifteenth gestational day. Previous studies have found impaired cognitive function in GD15 MAM rats, and a reduced seizure threshold.[7] At the cellular level, dysplastic hippocampal neurons in the MAM model were shown to have reduced potassium current function and expression for the Kv4.2 channel subunit [8] These findings may contribute to the spontaneous seizures and reduced seizure thresholds seen in this model.
References
- "Methylazoxymethanol Acetate – Compound Summary". PubChem. National Center for Biotechnology Information. Retrieved 9 June 2012.
- Jones, CA; Watson, DJG; Fone, KCF (1 October 2011). "Animal models of schizophrenia". British Journal of Pharmacology. 164 (4): 1162–1194. doi:10.1111/j.1476-5381.2011.01386.x. PMC 3229756. PMID 21449915.
- Baraban, Scott C.; Schwartzkroin, Philip A. (31 March 1996). "Flurothyl seizure susceptibility in rats following prenatal methylazoxymethanol treatment". Epilepsy Research. 23 (3): 189–194. doi:10.1016/0920-1211(95)00094-1. PMID 8739122. S2CID 21818415.
- Hradetzky, Eva; et al. (28 September 2011). "The Methylazoxymethanol Acetate (MAM-E17) Rat Model: Molecular and Functional Effects in the Hippocampus". Neuropsychopharmacology. 37 (2): 364–377. doi:10.1038/npp.2011.219. PMC 3242314. PMID 21956444.
- Chalkiadaki, Kleanthi; Velli, Aggeliki; Kyriazidis, Evangelos; Stavroulaki, Vasiliky; Vouvoutsis, Vasilis; Chatzaki, Ekaterini; Aivaliotis, Michalis; Sidiropoulou, Kyriaki. "Development of the MAM model of schizophrenia in mice: Sex similarities and differences of prefrontal cortical and hippocampal function" (PDF). bioRxiv.
- Harrington, Emily; et al. (January 2007). "Altered glutamate receptor-transporter and spontaneous seizures in rats exposed to methylazoxymethanol in utero". Epilepsia. 48 (1): 158–168. doi:10.1111/j.1528-1167.2006.00838.x. PMID 17241223. S2CID 23267780.
- Moshé, editors, Asla Pitkänen, Philip A. Schwartzkroin, Solomon L. (2006). Models of seizures and epilepsy. Amsterdam: Elsevier Academic. pp. 305–312. ISBN 0120885549.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - Castro, Peter; et al. (1 September 2001). "AHippocampal heterotopia lack functional Kv4.2 potassium channels in the methylazoxymethanol model of cortical malformations and epilepsy". Journal of Neuroscience. 21 (17): 6626–6634. doi:10.1111/j.1528-1167.2011.03264.x. PMC 3230777. PMID 21933177.