Orthognathic surgery
Orthognathic surgery (/ˌɔːrθəɡˈnæθɪk/), also known as corrective jaw surgery or simply, jaw surgery, is surgery designed to correct conditions of the jaw and lower face related to structure, growth, airway issues including sleep apnea, TMJ disorders, malocclusion problems primarily arising from skeletal disharmonies, and other orthodontic dental bite problems that cannot be treated easily with braces, as well as the broad range of facial imbalances, disharmonies, asymmetries, and malproportions where correction may be considered to improve facial aesthetics [1] and self-esteem.
| Orthognathic surgery | |
|---|---|
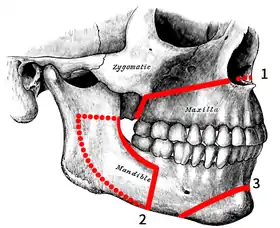 Osteotomies of the jaws:
1. LeFort I 2. Bilateral Sagittal Split 3. Genioplasty 4. IMDO 5. GenioPaully 6. Custom PEEK 7. SARME 8. Custom BIMAX 9. Super BIMAX | |
| ICD-9-CM | 76.6 |
The origins of orthognathic surgery belong in oral surgery, and the basic operations related to the surgical removal of impacted or displaced teeth – especially where indicated by orthodontics to enhance dental treatments of malocclusion and dental crowding. One of the first published cases of orthognathic surgery was the one from Dr. Simon P. Hullihen in 1849.
Originally coined by Harold Hargis, it was more widely popularised first in Germany and then most famously by Hugo Obwegeser who developed the bilateral sagittal split osteotomy (BSSO). This surgery is also used to treat congenital conditions such as cleft palate.[2] Typically surgery is performed via the mouth, where jaw bone is cut, moved, modified, and realigned to correct malocclusion or dentofacial deformity. The word "osteotomy" means the division of bone by means of a surgical cut.
The "jaw osteotomy", either to the upper jaw or lower jaw (and usually both) allows (typically) an oral and maxillofacial surgeon to surgically align an arch of teeth, or the segment of a dental arch with its associated jawbone, relative to other segments of the dental arches. Working with orthodontists, the coordination of dental arches has primarily been directed to create a working occlusion. As such, orthognathic surgery is seen a secondary procedure supporting a more fundamental orthodontic objective.
It is only recently, and especially with the evolution of oral and maxillofacial surgery in establishing itself as a primary medical specialty – as opposed to its long term status as a dental speciality – that orthognathic surgery has increasingly emerged as a primary treatment for obstructive sleep apnoea, as well as for primary facial proportionality or symmetry correction.
The primary use of surgery to correct jaw disproportion or malocclusion is rare in most countries due to private health insurance and public hospital funding and health access issues. A small number of mostly heavily socialist funded countries report that jaw correction procedures occur in some form or other in about 5% of a general population, but this figure would be at the extreme end of service [3][4][5] presenting with dentofacial deformities like maxillary prognathisms, mandibular prognathisms, open bites, difficulty chewing, difficulty swallowing, temporomandibular joint dysfunction pains, excessive wear of the teeth, and receding chins.
Increasingly, as people are more able to self fund surgery, 3D facial diagnostic and design systems have emerged, as well as new operations that enable for a broad range of jaw correction procedures that have become readily accessible; in particularly in private maxillofacial surgical practice. These procedures include IMDO, SARME, GenioPaully, custom BIMAX, and custom PEEK procedures. These procedures are replacing the traditional role of certain orthognathic surgery operations that have for decades served wholly and primarily orthodontic or dental purposes.[6]
Medical uses

It is estimated that nearly 5% of the UK or US population present with dentofacial deformities that are not amenable to orthodontic treatment requiring orthognathic surgery as a part of their definitive treatment.[7][4][5] Orthognathic surgery can be used to correct:
- Gross jaw discrepancies (anteroposterior, vertical, or transverse discrepancies)[8]
- Skeletofacial discrepancies associated with documented sleep apnea, airway defects, and soft tissue discrepancies
- Skeletofacial discrepancies associated with documented temporomandibular joint pathology
A disproportionately grown upper or lower jaw causes dentofacial deformities. Chewing becomes problematic, and may also cause pain due to straining of the jaw muscle and bone. Deformities range from micrognathia, which is when the mandible does not grow far forward enough (over bite), and when the mandible grows too much, causing an under bite; all of which are uncomfortable. Also, a total maxilla osteotomy is used to treat the "long face syndrome", known as the skeptical open bite, idiopathic long face, hyper divergent face, total maxillary alveolar hyperplasia, and vertical maxillary excess. Prior to surgery, surgeons should take x-rays of the patient's jaw to determine the deformity, and to make a plan of procedures.[9] Mandible osteotomies, or corrective jaw surgeries, benefit individuals who have difficulty chewing, swallowing, TMJ pains, excessive wear of the teeth, open bites, overbites, underbites, or a receding chin. The deformities listed above can be perfected by an osteotomy surgery of either the maxilla or mandible (whichever the deformity calls for), which is performed by an oral surgeon who is specialized in the working with both the upper and lower jaws.[10] Orthognathic surgery is also available as a very successful treatment (90–100%) for obstructive sleep apnea.[11]
- Cleft lip and palate
Orthognathic surgery is a well established and widely used treatment option for insufficient growth of the maxilla in patients with an orofacial cleft.[12] There is some debate regarding the timing of orthognathic procedures, to maximise the potential for natural growth of the facial skeleton.[13] Patient reported aesthetic outcomes of orthognathic surgery for cleft lip and palate appear to be of overall satisfaction,[14][15] despite complications that may arise. A potentially significant long-term outcome of orthognathic surgery is impaired maxillary growth, due to scar tissue formation.[16] A 2013 systematic review comparing traditional orthognathic surgery with maxillary distraction osteogenesis found that the evidence was of low quality; it appeared that both procedures might be effective, but suggested distraction osteogenesis might reduce the incidence of long-term relapse.[17] The most common causes of cleft lip and palate are genetic and environmental factors. Clefts are known to occur due to folic acid deficiency, iron and iodine deficiency[18]
Risks
Although infrequent, there can be complications such as bleeding, swelling, infection, nausea and vomiting.[19] Infection rates of up to 7% are reported after orthognathic surgery; antibiotic prophylaxis reduces the risk of surgical site infections when the antibiotics are given during surgery and continued for longer than a day after the operation.[20]
There can also be some post operative facial numbness due to nerve damage.[21] Diagnostics for nerve damage consist of: brush-stroke directional discrimination (BSD), touch detection threshold (TD), warm/cold (W/C) and sharp/blunt discrimination (S/B), electrophysiological tests (mental nerve blink reflex (BR), nerve conduction study (NCS), and cold (CDT) and warm (WDT) detection thresholds.[22] The inferior alveolar nerve, which is a branch of the mandibular nerve, must be identified during surgery and worked around carefully in order to minimize nerve damage. The numbness may be either temporary, or more rarely, permanent.[23] Recovery from the nerve damage typically occurs within three months after repair.
Surgery
Orthognathic surgery is performed by maxillofacial or an oral surgeon or a plastic surgeon in collaboration with an orthodontist. It often includes braces before and after surgery, and retainers after the final removal of braces. Orthognathic surgery is often needed after reconstruction of cleft palate or other major craniofacial anomalies. Careful coordination between the surgeon and orthodontist is essential to ensure that the teeth will fit correctly after the surgery.
Planning
Planning for the surgery usually involves input from a multidisciplinary team, including oral and maxillofacial surgeons, orthodontists, and occasionally a speech and language therapist. Although it depends on the reason for surgery, working with a speech and language therapist in advance can help minimize potential relapse. The surgery usually results in a noticeable change in the patient's face; a psychological assessment is occasionally required to assess patient's need for surgery and its predicted effect on the patient. Radiographs and photographs are taken to help in the planning. There is also advanced software that can predict the shape of the patient's face after surgery,[24][25][26][27][28] which is useful for the planning and also explaining the surgery to the patient and the patient's family.[29] Great care needs to be taken during the planning phase to maximize airway patency.
Orthodontics are a critical component of orthognathic surgery. Traditionally the presurgical orthodontic phase can take as long as one year and undertaken with conventional metal braces.[30] However, these days new approaches and paradigms exist including surgery-first [31] And using clear aligner orthodontia (like Invisalign)[32][33]
Sagittal split osteotomy

This procedure is used to correct mandible retrusion and mandibular prognathism (over and under bite). First, a horizontal cut is made on the inner side of the ramus mandibulae, extending anterally to the anterior portion of the ascending ramus. The cut is then made inferiorly on the ascending ramus to the descending ramus, extending to the lateral border of the mandible in the area between the first and second molar. At this time, a vertical cut is made extending inferior to the body of the mandible, to the inferior border of the mandible. All cuts are made into the middle of the bone, where bone marrow is present. Then, a chisel is inserted into the pre existing cuts and tapped gently in all areas to split the mandible of the left and right side. From here, the mandible can be moved either forwards or backwards. If sliding backwards, the distal segment must be trimmed to provide room in order to slide the mandible backwards. Lastly, the jaw is stabilized using stabilizing screws that are inserted extra-orally. The jaw is then wired shut for approximately 4–5 weeks.[34]

Genioplasty osteotomy (intra-oral)
This procedure is used for the advancement (movement forward) or retraction (movement backwards) of the chin. First, incisions are made from the first bicuspid to the first bicuspid, exposing the mandible. Then, soft tissue of the mandible is detached from the bone; done by stripping attaching tissues. A horizontal incision is then made inferior to the first bicuspids, bilaterally, where bone cuts (osteotomies) are made vertically inferior, extending to the inferior border of the mandible, thereby detaching the bony segments of the mandible. The bony segments are stabilized with titanium plates; no fixation (binding of the jaw) necessary. If advancement is indicated for the chin, there are inert products available to implant onto the mandible, utilizing titanium screws, bypassing bone cuts.[35][36]
GenioPaully
This is a modified box osteotomy of the chin, designed to deliberately grab the paired geniohyoid muscles – which are otherwise missed by the normal genioplasty procedure – in order to deliberately pull the hyoid and epiglottis forward. Use of the GenioPaully is common with IMDO and custom BIMAX procedures in deliberately curing a patient of obstructive sleep apnoea.
Rapid palatal expansion osteotomy
When a patient has a constricted (oval shape) maxilla, but normal mandible, many orthodontists request a rapid palatal expansion. This consists of the surgeon making horizontal cuts on the lateral board of the maxilla, extending anterally to the inferior border of the nasal cavity. At this time, a chisel designed for the nasal septum is utilized to detach the maxilla from the cranial base. Then, a pterygoid chisel, which is a curved chisel, is used on the left and right side of the maxilla to detach the pterygoid palates. Care must be taken as to not injure the inferior palatine artery. Prior to the procedure, the orthodontist has an orthopedic appliance attached to the maxilla teeth, bilaterally, extending over the palate with an attachment so the surgeon may use a hex-like screw to place into the device to push from anterior to posterior to start spreading the bony segments.[34] The expansion of the maxilla may take up to eight weeks with the surgeon advancing the expander hex lock, sideways (← →), once a week.
Post operation
After orthognathic surgery, patients are often required to adhere to an all-liquid diet for a time. Weight loss due to lack of appetite and the liquid diet is common. Normal recovery time can range from a few weeks for minor surgery, to up to a year for more complicated surgery. For some surgeries, pain may be minimal due to minor nerve damage and lack of feeling. Doctors will prescribe pain medication and prophylactic antibiotics to the patient. There is often a large amount of swelling around the jaw area, and in some cases bruising. Most of the swelling will disappear in the first few weeks, but some may remain for a few months.
Recovery
All dentofacial osteotomies require an initial healing time of 2–6 weeks with secondary healing (complete bony union and bone remodeling) taking an additional 2–4 months. The jaw is sometimes immobilized (movement restricted by wires or elastics) for approximately 1–4 weeks. However, the jaw will still require two to three months for proper healing. Lastly, if screws were inserted in the jaw, bone will typically grow over them during the two to three month healing period. Patients also may not drive or operate vehicles or large machinery during the consumption of painkillers, which are typically taken for six to eight days after the surgery, depending on the pain experienced. Immediately after surgery, patients must adhere to certain infection preventing instructions such as daily cleaning, and the consumption of antibiotics. Cleaning of the mouth should always be done regardless of surgery to ensure healthy, strong teeth. Patients are able to return to work 2–6 weeks after the surgery, but must follow the specific rules for recovery for ~8 weeks.[37]
History
Mandible and maxilla osteotomies date to the 1940s. They were used to correct dentofacial deformities like a malocclusion, and a prognathism.[38] Advances have been made in the procedures, and in the anesthesia used. In 1985, mandible and maxilla osteotomies were effectively used to correct more extreme deformities like receding chins, and to relieve pain from temporomandibular joint disorder (TMJ).
Prior to 1991, some patients undergoing a dentofacial osteotomy still had third molars (wisdom teeth), and had them removed during surgery. An extensive study done by Dr. M Lacy and Dr. R Colcleugh, was used to identify threats of combining the two surgeries used 83 patients from the time span of 1987 and 1991. Patients were reviewed, and divided into two groups; those who had, and those who did not have their third molars extracted during the dentofacial Osteotomy. The study showed that 73% of patients developed an infection of the hardware inserted into the jaw when having their third molars removed during an osteotomy. The data indicated that getting the osteotomy and the third molar extraction at the same time highly increases the chances of infection development.[39]
Advances in the surgical techniques allow surgeons to perform the surgery under local anesthesia with assistance from intravenous sedation. Dr. Raffaini introduced this technique in 2002 after a four-year study done with local anesthesia and assistance from intravenous sedation. Prior to this, surgeons would fully sedate patients, hospitalizing them shortly after the surgery for a 2–3 day recovery, specifically from the anesthesia. Advancements allow surgeons to expand the use of an osteotomy on more parts of the jaws with faster recovery time, less pain, and no hospitalization, making the surgery more effective with respect to time and recovery.[40] The procedure, which is strictly used for a mandibular (jaw) deformity and mobilization, has advanced from similar, very effective procedures performed since 1985. The original mandible and maxilla osteotomy procedure still remains almost unchanged, as it is the simplest and still the most effective for dentofacial deformity correction.
References
- Aesthetic orthognathic surgery and rhinoplasty. Derek M. Steinbacher. Hoboken, NJ. 2019. ISBN 978-1-119-18711-0. OCLC 1057242839.
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: others (link) - Bill J, Proff P, Bayerlein T, Blens T, Gedrange T, Reuther J (September 2006). "Orthognathic surgery in cleft patients". J Craniomaxillofac Surg. 34 (Suppl 2): 77–81. doi:10.1016/S1010-5182(06)60017-6. PMID 17071397.
- Posnick, Jeffrey C. (September 2013). Orthognatic Surgery: Principles and Practice. Amsterdam: Elsevier. pp. 61–68. doi:10.1016/B978-1-4557-2698-1.00003-4. ISBN 978-145572698-1.
- Harrington C, Gallagher JR, Borzabadi-Farahani A (April 2015). "A retrospective analysis of dentofacial deformities and orthognathic surgeries using the index of orthognathic functional treatment needs (IOFTN)". Int J Pediatr Otorhinolaryngol. 79 (7): 1063–6. doi:10.1016/j.ijporl.2015.04.027. PMID 25957779.
- Borzabadi-Farahani A, Eslamipour F, Shahmoradi M (2016). "Functional needs of subjects with dentofacial deformities: A study using the index of orthognathic functional treatment need (IOFTN)". J Plast Reconstr Aesthet Surg. 69 (6): 796–801. doi:10.1016/j.bjps.2016.03.008. PMID 27068664.
- Coceancig, Paul (2021). 6Ways To Design A Face: corrective jaw surgery to optimize bite, airway, and facial balance. Batavia: Quintessence Publishing. ISBN 978-086715966-0.
- Posnick, Jeffrey C. (September 2013). Orthognatic Surgery: Principles and Practice. Amsterdam: Elsevier. pp. 61–68. doi:10.1016/B978-1-4557-2698-1.00003-4. ISBN 978-145572698-1.
- "Ortho Criteria". AAOMS.org. American Association of Oral and Maxillofacial Surgeons. Retrieved 2014-11-05.
- Arnet, Gary F., and Linda M. Basehore. "Dentofacial reconstruction." The American Journal of Nursing. 12. 84 (1984): 1488-490.
- William H. Bell; William R. Proffit; Raymond P. White (1980). Surgical correction of dentofacial deformities. Saunders. ISBN 978-0-7216-1675-9.
- Prinsell JR (December 1999). "Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients". Chest. 116 (6): 1519–29. doi:10.1378/chest.116.6.1519. PMID 10593771.
- DeLuke, Dean M; Marchand, Anick; Robles, Elizabeth C; Fox, Patricia (1997). "Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases". Journal of Oral and Maxillofacial Surgery. 55 (7): 694–697. doi:10.1016/s0278-2391(97)90579-6. PMID 9216501.
- Wolford, Larry M.; Stevao, Eber L.L. (2016-11-10). "Correction of jaw deformities in patients with cleft lip and palate". Proceedings (Baylor University. Medical Center). 15 (3): 250–254. doi:10.1080/08998280.2002.11927848. ISSN 0899-8280. PMC 1276618. PMID 16333445.
- Munz, S. M.; Edwards, S. P.; Inglehart, M. R. (2011-08-01). "Oral health-related quality of life, and satisfaction with treatment and treatment outcomes of adolescents/young adults with cleft lip/palate: an exploration". International Journal of Oral and Maxillofacial Surgery. 40 (8): 790–796. doi:10.1016/j.ijom.2011.03.002. PMID 21474288.
- Gkantidis, Nikolaos; Papamanou, Despina A.; Christou, Panagiotis; Topouzelis, Nikolaos (2013). "Aesthetic outcome of cleft lip and palate treatment. Perceptions of patients, families, and health professionals compared to the general public". Journal of Cranio-Maxillofacial Surgery. 41 (7): e105–e110. doi:10.1016/j.jcms.2012.11.034. PMID 23287059.
- Daskalogiannakis, John; Mehta, Manisha (2009-10-05). "The Need for Orthognathic Surgery in Patients With Repaired Complete Unilateral and Complete Bilateral Cleft Lip and Palate". The Cleft Palate-Craniofacial Journal. 46 (5): 498–502. doi:10.1597/08-176.1. PMID 19929100. S2CID 12917010.
- Kloukos, Dimitrios; Fudalej, Piotr; Sequeira-Byron, Patrick; Katsaros, Christos; Kloukos, Dimitrios (2013). Kloukos, Dimitrios (ed.). "Maxillary distraction osteogenesis versus orthognathic surgery for cleft lip and palate patients". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD010403.

- Balaji, SM (8 February 2018). "CLEFT LIP AND PALATE SURGERY".
- Silva AC, O'Ryan F, Poor DB (September 2006). "Postoperative nausea and vomiting (PONV) after orthognathic surgery: a retrospective study and literature review". J. Oral Maxillofac. Surg. 64 (9): 1385–97. doi:10.1016/j.joms.2006.05.024. PMID 16916674.
- Brignardello-Petersen, Romina; Carrasco-Labra, Alonso; Araya, Ignacio; Yanine, Nicolás; Cordova Jara, Luis; Villanueva, Julio (2015-01-05). "Antibiotic prophylaxis for preventing infectious complications in orthognathic surgery". The Cochrane Database of Systematic Reviews. 1 (1): CD010266. doi:10.1002/14651858.CD010266.pub2. ISSN 1469-493X. PMC 9674113. PMID 25561078.

- Panula K, Finne K, Oikarinen K (October 2001). "Incidence of complications and problems related to orthognathic surgery: a review of 655 patients". J. Oral Maxillofac. Surg. 59 (10): 1128–36, discussion 1137. doi:10.1053/joms.2001.26704. PMID 11573165.
- Teerijoki-Oksa T, Jääskeläinen SK, Forssell K, Forssell H (2004). "Recovery of nerve injury after mandibular sagittal split osteotomy. Diagnostic value of clinical and electrophysiologic tests in the follow-up". Int J Oral Maxillofac Surg. 33 (2): 134–40. doi:10.1054/ijom.2003.0463. PMID 15050068.
- Eckert AW, Maurer P, Kriwalsky MS, Schubert J (September 2006). "P.292 Complications in orthognathic surgery". J Craniomaxillofac Surg. 34 (Suppl 1): 206. doi:10.1016/S1010-5182(06)60797-X.
- Mischkowski RA, Zinser MJ, Kübler AC, Krug B, Seifert U, Zöller JE (December 2006). "Application of an augmented reality tool for maxillary positioning in orthognathic surgery—a feasibility study". J Craniomaxillofac Surg. 34 (8): 478–83. doi:10.1016/j.jcms.2006.07.862. PMID 17157519.
- Uechi J, Okayama M, Shibata T, et al. (December 2006). "A novel method for the 3-dimensional simulation of orthognathic surgery by using a multimodal image-fusion technique". Am J Orthod Dentofacial Orthop. 130 (6): 786–98. doi:10.1016/j.ajodo.2006.03.025. PMID 17169742.
- Park, Kitae E.; Maniskas, Seija; Allam, Omar; Pourtaheri, Navid; Steinbacher, Derek M. (January 2021). "Orthognathic Surgery to Improve Facial Profile: Assessment, 3-Dimensional Planning, and Technique". Aesthetic Surgery Journal. Open Forum. 3 (1): ojaa051. doi:10.1093/asjof/ojaa051. ISSN 2631-4797. PMC 7954391. PMID 33791672.
- Steinbacher, Derek M. (December 2015). "Three-Dimensional Analysis and Surgical Planning in Craniomaxillofacial Surgery". Journal of Oral and Maxillofacial Surgery. 73 (12 Suppl): S40–56. doi:10.1016/j.joms.2015.04.038. ISSN 1531-5053. PMID 26608154.
- Pfaff, Miles J.; Steinbacher, Derek M. (March 2016). "Plastic Surgery Applications Using Three-Dimensional Planning and Computer-Assisted Design and Manufacturing". Plastic and Reconstructive Surgery. 137 (3): 603e–616e. doi:10.1097/01.prs.0000479970.22181.53. ISSN 1529-4242. PMID 26910704. S2CID 35719377.
- Tsuji M, Noguchi N, Shigematsu M, et al. (September 2006). "A new navigation system based on cephalograms and dental casts for oral and maxillofacial surgery". Int J Oral Maxillofac Surg. 35 (9): 828–36. doi:10.1016/j.ijom.2006.02.024. PMID 16690251.
- Contemporary treatment of dentofacial deformity. William R. Proffit, Raymond P. White, David M. Sarver. St. Louis, Mo.: Mosby. 2003. ISBN 0-323-01697-9. OCLC 49221892.
{{cite book}}: CS1 maint: others (link) - Chang, Joy; Steinbacher, Derek; Nanda, Ravindra; Uribe, Flavio (July 2019). ""Surgery-First" Approach with Invisalign Therapy to Correct a Class II Malocclusion and Severe Mandibular Retrognathism". Journal of Clinical Orthodontics. 53 (7): 397–404. ISSN 0022-3875. PMID 31648215.
- Kankam, Hadyn; Madari, Sarika; Sawh-Martinez, Rajendra; Bruckman, Karl C.; Steinbacher, Derek M. (July 2019). "Comparing Outcomes in Orthognathic Surgery Using Clear Aligners Versus Conventional Fixed Appliances". The Journal of Craniofacial Surgery. 30 (5): 1488–1491. doi:10.1097/SCS.0000000000005572. ISSN 1536-3732. PMID 31299750. S2CID 139100781.
- Kankam, Hadyn K. N.; Gupta, Himank; Sawh-Martinez, Rajendra; Steinbacher, Derek M. (July 2018). "Segmental Multiple-Jaw Surgery without Orthodontia: Clear Aligners Alone". Plastic and Reconstructive Surgery. 142 (1): 181–184. doi:10.1097/PRS.0000000000004491. ISSN 1529-4242. PMID 29952900. S2CID 49475709.
- Dr. Charles A. Loschiavo. Personal. 2 April 2009.
- Kim, Yunsoo A.; Steinbacher, Derek M. (August 2014). "Demineralized bone-fibrin sandwich for genioplasty". Aesthetic Plastic Surgery. 38 (4): 755–758. doi:10.1007/s00266-014-0362-y. ISSN 1432-5241. PMID 24938690. S2CID 27263835.
- Walker, Marc E.; Sawh‐Martinez, Rajendra; Steinbacher, Derek M. (2019), "Osseous Genioplasty", Aesthetic Orthognathic Surgery and Rhinoplasty, John Wiley & Sons, Ltd, pp. 517–533, doi:10.1002/9781119187127.ch20, ISBN 978-1-119-18712-7, S2CID 242253796, retrieved 2021-04-11
- Mandible (Lower Jaw) Osteotomy. 2007. British Association of Oral and Maxillofacial Surgeon (BAOMS). 29 February 2009 http://www.baoms.org.uk
- Puricelli, Edela. "A new technique for mandibular osteotomy." Head & Face Medicine 3.15 (2007). Head & Face Medicine. 13 March 2007. BioMed Central Ltd. 27 February 2009 http://www.head-face-med.com
- Lacey MS, Colcleugh RG (1995). "Infected screws in patients treated by mandibular sagittal split osteotomy". J. Oral Maxillofac. Surg. 53 (5): 510–2, discussion 513. doi:10.1016/0278-2391(95)90059-4. PMID 7722717.
- Raffaini M, Hernandez Alfaro F, Ghilardi R, Garcia Lopez A (2002). "The sagittal mandibular osteotomy under local anesthesia and intravenous sedation: four years of multicenter experience". Int J Adult Orthodon Orthognath Surg. 17 (4): 267–71. PMID 12592998.