Traction (orthopedics)
Traction is a set of mechanisms for straightening broken bones or relieving pressure on the spine[1] and skeletal system. There are two types of traction: skin traction and skeletal traction. They are used in orthopedic medicine.
| Traction (orthopedics) | |
|---|---|
 | |
| ICD-9-CM | 93.4 |
| MeSH | D014143 |
Techniques
Traction procedures have largely been replaced by more modern techniques, but certain approaches are still used today:
- Milwaukee brace
- Bryant's traction
- Buck's traction, involving skin traction. It is widely used for femoral fractures, low back pain, acetabular fractures and hip fractures.[2] Skin traction rarely causes fracture reduction, but reduces pain and maintains the length of the bone.[2]
- Dunlop's traction – humeral fractures in children
- Russell's traction
Skeletal traction
Although the use of traction has decreased over the years, an increasing number of orthopaedic practitioners are using traction in conjunction with bracing (see Milwaukee brace).
Harrison et al. (2005) found that mirror image (opposite posture) postural corrective exercises and a new method of lumbosacral tilt traction resulted in 50% reduction in trunk tilt and were associated with nearly resolved pain intensity in this patient population.[3] These researchers felt that their findings warranted further study in the conservative treatment of chronic low back pain and spinal disorders.
Spinal decompression
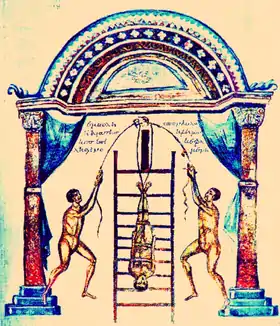
Spinal traction as a means of spinal decompression is often applied without directly touching bones as other methods of traction do. This is sometimes isolated inside-out by inflatable girdles or use of the transversus abdominis muscle. It is also done in conjunction with thigh-supported flexed-hip traction (inversion chairs, back hyperextensions) or done in conjunction with whole-leg traction (boots, tables) via inverted forms of suspension.
Traction of the spine (except the cervical) also occurs with upright suspension of the body from the arms, such as with pull-ups, dips, captain's chair, chinnings (chin up exercise) or other fitness movements with the feet dangling.
Mechanical traction in physical therapy
Mechanical traction can be used for patients with cervical and lumbar spinal disorders such as cervical radiculopathy or lumbar spinal stenosis. Lumbar traction has been widely used in the clinic, previous meta-analyses have confirmed that mechanical traction in the supine position can relieve short-term pain in patients with radiculopathy.[4] It may be applied mechanically through the use of an apparatus with two different modes: intermittent or continuous.
Physiological goals:
- Separation of vertebral bodies
- Movement of facet joints
- Expansion of intervertebral foramen
- Stretch of soft tissues
When mechanical traction is combined with other physical therapy modalities such as passive mobilization, massage, stretching and active exercises, it is an effective treatment for pain reduction in cervical or lumbar spine disorders. [5]
Colombo et al. (2020) found that there are better results in mechanical traction therapy when compared to manual traction therapy. Furthermore, continuous traction was found to have a greater significance than intermittent traction. The suggested delivery of traction therapy was found to be mechanical traction with continuous traction.[6]
Recent guidelines have been put forward for the use of cervical traction to treat cervical radiculopathy. Only low quality evidence has been released and the authors of these guidelines encourage researchers to intensify studies on tractions effect on cervical radiculopathy.[7] Researchers have also demonstrated lumbar traction to be advantageous in treating low back pain. [8] Three studies in 2017 confirmed an increase of nutrient and water flow into the intervertebral discs after traction treatment.[9]
Purpose
The purpose of traction is to:
- Regain normal length and alignment of involved bone
- Lessen or eliminate muscle spasms
- Relieve pressure on nerves, especially spinal nerves
- Prevent or reduce skeletal deformities or muscle contractures
- To provide a fusiform tamponade around a bleeding vessel
In most cases traction is only one part of the treatment plan of a patient needing such therapy. The physician's order will contain:
- Type of traction
- Amount of weight to be applied
- Frequency of neurovascular checks if more frequent than every four hours
- Site care of inserted pins, wires, or tongs
- The site and care of straps, harnesses and halters
- The inclusion of any other physical restraints / straps or appliances (e.g., mouth guard)
- The discontinuation of traction
Future
The variability of traction delivery protocols causes a gap that may be the reason for negative conclusions that traction has no positive effects. A key to the future success of traction may be finding the proper therapeutic dosage levels. Suboptimal dosage choices may be a key for the negative conclusions on traction. Different dosage levels for aspects such as traction force, traction rhythm, duration of treatment, and frequency could be the key to providing efficient effects. Proper dosage levels for any therapeutic treatment will be vital for recovery efficiency. Patients may have a “directional preference” to an axial force which may be an underlying cause for positive results. Future research is needed to discover if directional preference has a positive therapeutic effect within traction.[10]
References
- Burke GL. "The Techniques of Traction and Manipulation of the Spine". Backache from Occiput to Coccyx.
- Skin Traction - Lower Extremity from University of Stellenbosch, Department of Orthopaedic Surgery. Retrieved May 2, 2013
- Harrison DE, Cailliet R, Betz JW, Harrison DD, Colloca CJ, Haas JW, et al. (March 2005). "A non-randomized clinical control trial of Harrison mirror image methods for correcting trunk list (lateral translations of the thoracic cage) in patients with chronic low back pain". European Spine Journal. 14 (2): 155–62. doi:10.1007/s00586-004-0796-z. PMC 3476700. PMID 15517424.
- Wang, Wenxian; Long, Feibing; Wu, Xinshun; Li, Shanhuan; Lin, Ji (2022-06-21). "Clinical Efficacy of Mechanical Traction as Physical Therapy for Lumbar Disc Herniation: A Meta-Analysis". Computational and Mathematical Methods in Medicine. 2022: 5670303. doi:10.1155/2022/5670303. ISSN 1748-670X. PMC 9239808. PMID 35774300.
- Romeo A, Vanti C, Boldrini V, Ruggeri M, Guccione AA, Pillastrini P, Bertozzi L (April 2018). "Cervical Radiculopathy: Effectiveness of Adding Traction to Physical Therapy-A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Physical Therapy. 98 (4): 231–242. doi:10.1093/physth/pzy001. PMID 29315428.
- Colombo, Claudio; Salvioli, Stefano; Gianola, Silvia; Castellini, Greta; Testa, Marco (2020-10-22). "Traction Therapy for Cervical Radicular Syndrome is Statistically Significant but not Clinically Relevant for Pain Relief. A Systematic Literature Review with Meta-Analysis and Trial Sequential Analysis". Journal of Clinical Medicine. 9 (11): 3389. doi:10.3390/jcm9113389. ISSN 2077-0383. PMC 7690405. PMID 33105668.
- Kjaer P, Kongsted A, Hartvigsen J, Isenberg-Jørgensen A, Schiøttz-Christensen B, Søborg B, et al. (September 2017). "National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy". European Spine Journal. 26 (9): 2242–2257. doi:10.1007/s00586-017-5121-8. PMID 28523381. S2CID 4048239.
- Lee JH, Choi KH, Kang S, Kim DH, Kim DH, Kim BR, et al. (September 2019). "Nonsurgical treatments for patients with radicular pain from lumbosacral disc herniation". The Spine Journal. 19 (9): 1478–1489. doi:10.1016/j.spinee.2019.06.004. PMID 31201860. S2CID 189898294.
- Mitchell UH, Helgeson K, Mintken P (September 2017). "Physiological effects of physical therapy interventions on lumbar intervertebral discs: A systematic review". Physiotherapy Theory and Practice. 33 (9): 695–705. doi:10.1080/09593985.2017.1345026. PMID 28715273. S2CID 33228144.
- Alrwaily M, Almutiri M, Schneider M (2018-09-17). "Assessment of variability in traction interventions for patients with low back pain: a systematic review". Chiropractic & Manual Therapies. 26 (1): 35. doi:10.1186/s12998-018-0205-z. PMC 6139896. PMID 30237870.
External links
- Byrne T (1999). "The setup and care of a patient in Buck's traction". Orthopedic Nursing. 18 (2): 79–83. doi:10.1097/00006416-199903000-00011. PMID 10410051.
- "Split Russell's / Buck Traction"
- synd/2984 at Who Named It? - Bryant's traction
- "Physio-pedia about another spinal traction therpay method"