Orbital emphysema
Orbital emphysema (/ˈɔː(r)bɪt(ə)l ˌemfɪˈsiːmə/, also known as pneumo-orbit[8]) is a medical condition that refers to the trapping of air within the loose subcutaneous around the orbit that is generally characterized by sudden onset swelling and bruising at the impacted eye, with or without deterioration of vision, which the severity depends on the density of air trapped under the orbital soft tissue spaces.[1][9]
| Orbital emphysema | |
|---|---|
| Other names | Pneumo-orbit |
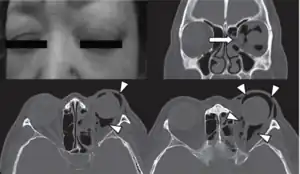 | |
| Woman with preorbital swelling in orbital emphysema shown in CT scans | |
| Pronunciation |
|
| Specialty | Ophthalmology |
| Symptoms | Swelling, bruising, globe dystopia, diplopia, restrict ocular motility, prohibit eyelid closure, loss of sensation over the upper cheek area, nausea, dizziness, vomiting, bradycardia, syncope, heart block[1][2] |
| Complications | Proptosis, visual impairment, central retinal artery occlusion, compressive optic neuropathy, orbital compartment syndrome.[3][4][5] |
| Duration | 7-10 Days[6] |
| Causes | sneezing, nose blowing, or coughing in patients with trauma, postoperative complications, infections |
| Diagnostic method | Based on medical history, computer tomography, and physical examination[6] |
| Differential diagnosis | Palpebral emphysema, true orbital emphysema, orbitopalperbal emphysema[3][6] |
| Treatment | No treatment for stage I and II, lateral canthotomy or cantholysis, orbital decompression by needle aspiration, and bone decompression for stage III and IV orbital emphysema[4][7] |
It is most commonly result from forceful sneezing, nose blowing, or coughing among patients with a history of periorbital trauma or orbital fractures that happened several hours-days in advance.[10] Rare occasions have also been reported in relation to individuals with no traumatic past events that include: infection, esophageal rupture, postoperative complications, pulmonary barotrauma, with the same predisposing factors (sneezing, nose blowing, or coughing).[11] A four-stage system of orbital emphysema was developed for severity classification. Clinical diagnosis can be made based on a combination of medical history, physical examination, and computed tomography.[6] There are three kinds of orbital emphysema including palpebral emphysema, true orbital emphysema, and orbitopalpebral emphysema.[6][3]
Orbital emphysema on its own is a mild and self-limiting disease, and usually requires no treatment. If related visual symptoms or other acute orbital compression symptoms are present,[12] lateral canthotomy or cantholysis, orbital decompression by needle aspiration,[7][4] and bone decompression[11][6][13][14][15][5] may be required to relieve orbital pressure and preserve vision.
Cause
Trauma
Blunt trauma caused by a direct blow at the orbital is the major leading cause of orbital emphysema.[1][16][17] Any object with force and/or speed, typically a ball, fist or vehicle accidents, can result in orbital floor and/or medial wall fractures.[18][19][20] These disruptions permit air entry into the orbital subcutaneous from the sinus, with a one-way check valve mechanism that forbids the air from exiting.[21][22] Victims are often found in sport-related concussion, automobile vehicle accidents, or snowboarding accidents.
Traumatic injuries do not cause onset swelling unless there is a forceful injection of air from vigorous sneezing, nose-blowing, or coughing.[10] These generate an acute increase in intraorbital pressure, compromising the intraorbital neurovascular structures, which subsequently trigger the development of orbital emphysema.[17][23][24]
Postoperative complications
Orbital emphysema is a common result of certain types of surgery, in particular the ones that involve orbital medial wall.[6][25] It may also occur in other oral, nasal, and maxillofacial surgical interventions, in which the occurrence is unexpected.[3][26][27] They can weaken sinuses, bony structure, induce deep orbital tissue damages, or globe perforation that cause air leakage into the periorbital soft tissues and superiorly into the supraorbital fat.[3][13][28] These surgical procedures may possibly introduce staphylococci, streptococci, and anaerobic bacteria via a compromised bony wall that can cause periorbital infection.[25] The corresponding weakened or degenerated tissues cannot withstand the sudden increase in intraocular pressure and impaired ocular perfusion, driven by severe coughing or sneezing. It subsequently results in air trapped in the periorbital subcutaneous tissue and the development of orbital emphysema, which is often mistaken as allergic reactions.[27] Without proper management can lead to cardiac life-threatening conditions such as cardiopulmonary embolism, cardiac tamponade, and respiratory distress, depending on the volume of air trapped under the facial soft tissues.[3][28]
Infection
Infections can spread beyond their initial location, including lamina papyracea.[3]
Signs and Symptoms
The signs and symptoms of orbital emphysema vary depending on the original cause, but it is preliminary associated with swelling, bruising, and tenderness around the impacted eye.[29] It may also involve proptosis or the deterioration of vision, typically diplopia.[1][23] The entrapped air may cause an acute increase in the intraocular pressure or vascular compromise that restrict ocular motility, prohibit the closure of eyelids, and the loss of sensation over the upper cheek areas.[30]
Server entrapment in the soft tissues tends to stimulate oculocardiac reflex, which is likely to generate significant vagal responses including nausea, dizziness, vomiting, bradycardia, syncope and heart block.[1][2] Without treating it promptly may subsequently result in compromisation of ocular function and visual impairment.[9][31][32]
Pathophysiology
Orbital emphysema occurs following forceful injection of air into the soft tissues of the orbit through a breach in one of the orbital walls which is typically associated with orbital fracture after blunt trauma, or less frequently with compressed air injuries, tumours and infections of the sinonasal region or complications after surgery.[1][7][33][34]
Orbital emphysema develops after an orbital fracture in a three-step process.[1][33] After the fracture has occurred on one of the orbital walls, a sino-orbital communication is established.[1][14][33][34][35] The communication will allow air to be forced from the sinuses into the orbit in the presence of a pressure gradient from forceful expiratory efforts, nose-blowing or even a sneeze.[1][7][33][34] Orbital emphysema is typically a harmless disorder because air escapes as quickly as it enters the fracture site, and the increase in intraorbital pressure is usually transient, lasting for as long as the sneeze or nose blowing.[33] However, when orbital soft tissues, such as fat,[1] falls back on the sino-orbital communication,[1][3][4][33] a one-way ball valve will be created, leading to the entrapment of air.[1][3][7][4][15][5][33] When sufficient air accumulates, it will result in acute compartment syndrome and vascular compromise,[1][7][4] causing complications including proptosis, visual impairment, central retinal artery occlusion, compressive optic neuropathy, and other severe complications caused by orbital compartment syndrome.[3][4][5]
There are three variations of orbital emphysema, namely palpebral emphysema, true orbital emphysema, and orbitopalpebral emphysema.[6][3]
Palpebral emphysema
Palpebral emphysema refers to emphysema of the eyelids alone. It is a rare kind of orbital emphysema which is usually caused by fractures of the lacrimal bone.[6][3][36] The lacrimal sac ruptures as a result of the fracture, allowing air from the nasal cavity to enter the tissues of the eyelid.[6][36] Alternatively, facial subcutaneous air may simply pass into the eyelids along fascial plane to produce palpebral emphysema. As long as the orbital septum is intact, air is confined in the eyelids.[6]
True orbital emphysema
True orbital emphysema occurs when there is air behind an intact orbital septum.[6][3][36] This condition arises due to a fracture of more than one bony orbital walls of paranasal sinuses and tearing of adjacent sinus mucosa, and communication of a sinus with the orbit is established. This fracture usually involves the ethmoid, and sometimes involves frontal, sphenoid, and maxillary sinuses.[6][3][36] The air usually enters the orbit when the pressure within the upper respiratory tract is increased due to expiratory efforts, nose blowing or sneezing.[6]
Orbitopalperbal emphysema
Orbitopalpebral emphysema refers to the trapping of air inside both the soft tissues of the orbit and the eyelid. It is usually a sequelae of a true orbital emphysema.[6][36] When too much air accumulates inside the orbit, the orbital septum ruptures due to high intraorbital pressure. Air may then pass freely from the orbit into the eyelids through the break in the orbital septum.[6][36]
Stages
There are four stages of orbital emphysema.[1][15]
Stage I
Stage I orbital emphysema can only be diagnosed with radiological films. There is only a small amount of intraorbital air, and the patient does not show any clinical signs or symptoms.[1][15]
Stage II
Stage II orbital emphysema develops as the intraorbital air volume increases, causing the eyeball to displace horizontally or vertically (globe dystopia) or to protrude anteriorly (proptosis). The patient may experience diplopia as a result of the globe displacement.[1][15]
Stage III
Stage III orbital emphysema develops when the limits of spontaneous decompression are exceeded. The pressure will be transmitted to orbital tissues and then to the globe, resulting in an increase in intraocular pressure which may cause visual loss when the nutrient vessels supplying the optic nerve are compressed.[1][15]
Stage IV
Stage IV orbital emphysema develops when the intraorbital air mass results in an intraocular pressure of more than 60 to 70 mmHg. The significantly elevated intraocular pressure will lead to central retinal artery occlusion, which may result in permanent and irreversible damage to the retina.[1][15]
Clinical Diagnosis
The diagnosis of orbital emphysema is usually made by physical examination of the eyelids,[11][35] and, or by computer tomography (CT).[11][6][3][15][34][37][38]
Physical examination
Physical examination of the eyelid can be done by the palpation for the pathognomonic cracking, crepitation,[11] and tense tissue[35] on the upper and lower eyelids. The findings of the examination are supported with the medical history of the patient and confirmed with orbital CT.[6]
Computed tomography (CT)


Computed tomography is effective and sensitive in the diagnosis of orbital emphysema,[3][37] as it can confirm the anatomical location and size of air, bony defects, indentation of the eyeball, and the condition of the optic nerve, as well as the presence of any extraocular muscle entrapment and herniation of preorbital fat into the sinus cavities.[3][15][38] The location of the orbital emphysema is present near the site of the fracture.[1][3] The scans are usually taken along the transverse plane. Transverse images allow the evaluation of fractures in medial and lateral orbital walls. By reformatting these transverse images or taking coronal images, the examination of orbital floor and roof is permitted. Helical scanning is preferred as it has a lower imaging time and radiation dose comparing to conventional scanning, especially when reforming transverse helical scans into coronal images.[3] The staging of orbital emphysema can then be determined with visual acuity examination and ophthalmoscopy.[6] A disadvantage of using a CT scan is that when detecting air after orbital trauma, the presence of a wooden foreign object can give a false positive result of orbital emphysema. The wooden object can mimic the presence of orbital emphysema. Therefore, patients’ medical history is crucial in making the correct diagnosis.[3]
Other tests
Conventional radiography is commonly employed for imaging orbital injuries and identifying orbital fractures.[3] It can be used to diagnose orbital emphysema because it shows the presence of air in the orbit best while the patient is standing upright.[3] Skull films of posterior-anterior, lateral projections, and orbital rim views are recommended to show fractures in orbital rims and walls.[34] However, CT scan is better than conventional radiography in the diagnosis of the condition,[3][37] as it has a lower high false-negative rate and non-diagnostic rate.[3]
Orbital emphysema can also be diagnosed by magnetic resonance imaging (MRI). Although MRI has a low sensitivity for detecting orbital fractures, it can be used to evaluate rectus muscle pathology, optic nerve pathology, and brain pathology, as well as vascular injury.[3]
Treatment
Orbital emphysema on its own is a mild and self-limiting disease.[1][6][14] The majority of cases of orbital emphysema are self-resolving[6][14][5] and do not need treatment.[11][12][14][5][34][36] The underlying causes and injuries that caused orbital emphysema, on the other hand, may be serious, necessitating urgent intervention including surgery.[34][36] If related visual symptoms or other acute orbital compression symptoms are present,[12] lateral canthotomy or cantholysis, orbital decompression by needle aspiration,[7][4] and bone decompression[11][6][13][14][15][5] may be required to relieve orbital pressure and preserve vision. Prophylactic oral antibiotics may be needed to prevent secondary infection.[1][33]
Reference list
- Hunts JH, Patrinely JR, Holds JB, Anderson RL (May 1994). "Orbital emphysema. Staging and acute management". Ophthalmology. 101 (5): 960–966. doi:10.1016/S0161-6420(94)31230-9. PMID 8190488.
- Abdesslem K, Sondes B, Wael E, Hajer T, Morched D, Fathi K, Mohamed A (December 2014). "[A case of post-traumatic severe orbital emphysema: case report and literature review]". Journal Français d'Ophtalmologie. 37 (10): e165–e167. doi:10.1016/j.jfo.2014.03.012. PMID 25455546.
- Gauguet JM, Lindquist PA, Shaffer K (1 January 2008). "Orbital Emphysema Following Ocular Trauma and Sneezing". Radiology Case Reports. 3 (1): 124. doi:10.2484/rcr.v3i1.124. PMC 4896116. PMID 27303505.
- Lin CY, Tsai CC, Kao SC, Kau HC, Lee FL (1 June 2016). "Needle decompression in a patient with vision-threatening orbital emphysema". Taiwan Journal of Ophthalmology. 6 (2): 93–95. doi:10.1016/j.tjo.2015.02.003. PMC 5602697. PMID 29018719.
- Roelofs KA, Starks V, Yoon MK (1 January 2019). "Orbital Emphysema: A Case Report and Comprehensive Review of the Literature". Ophthalmic Plastic and Reconstructive Surgery. 35 (1): 1–6. doi:10.1097/iop.0000000000001216. PMID 30130334. S2CID 52054981.
- Zimmer-Galler IE, Bartley GB (February 1994). "Orbital emphysema: case reports and review of the literature". Mayo Clinic Proceedings. 69 (2): 115–121. doi:10.1016/s0025-6196(12)61036-2. PMID 8309261.
- Singh M, Phua VM, Sundar G (May 2007). "Sight-threatening orbital emphysema treated with needle decompression". Clinical & Experimental Ophthalmology. 35 (4): 386–387. doi:10.1111/j.1442-9071.2007.01494.x. PMID 17539798. S2CID 28193380.
- Al-Shammari L, Majithia A, Adams A, Chatrath P (March 2008). "Tension pneumo-orbit treated by endoscopic, endonasal decompression: case report and literature review". The Journal of Laryngology and Otology. 122 (3): e8. doi:10.1017/S002221510700165X. PMID 18267045. S2CID 35365970.
- Harmer SG, Ethunandan M, Zaki GA, Brennan PA (March 2007). "Sudden transient complete loss of vision caused by nose blowing after a fracture of the orbital floor". The British Journal of Oral & Maxillofacial Surgery. 45 (2): 154–155. doi:10.1016/j.bjoms.2005.06.008. PMID 16026907.
- Glazer ES, Meyerson SL (1 July 2008). "Delayed presentation and treatment of tracheobronchial injuries due to blunt trauma". Journal of Surgical Education. 65 (4): 302–308. doi:10.1016/j.jsurg.2008.06.006. PMID 18707665.
- Ariyoshi Y, Naito H, Yumoto T, Iida A, Yamamoto H, Fujisaki N, et al. (18 June 2019). "Orbital Emphysema as a Consequence of Forceful Nose-Blowing: Report of a Case". Case Reports in Emergency Medicine. 2019: 4383086. doi:10.1155/2019/4383086. PMC 6604475. PMID 31316840.
- Tsai SH, Chu SJ (November 2008). "Orbital emphysema". The Journal of Trauma. 65 (5): 1200. doi:10.1097/01.ta.0000236035.18788.9c. PMID 18277265.
- Lee SL, Mills DM, Meyer DR, Silver SM (November 2006). "Orbital emphysema". Ophthalmology. 113 (11): 2113.e1–2113.e2. doi:10.1016/j.ophtha.2006.06.013. PMID 17074576.
- Ababneh OH (June 2013). "Orbital, subconjunctival, and subcutaneous emphysema after an orbital floor fracture". Clinical Ophthalmology. 7: 1077–1079. doi:10.2147/opth.s44649. PMC 3678949. PMID 23766631.
- Shameer A, Pushker N, Lokdarshi G, Basheer S, Bajaj MS (September 2017). "Emergency Decompression of Orbital Emphysema with Elevated Intraorbital Pressure". The Journal of Emergency Medicine. 53 (3): 405–407. doi:10.1016/j.jemermed.2016.10.021. PMID 28992871.
- Caranci F, Cicala D, Cappabianca S, Briganti F, Brunese L, Fonio P (October 2012). "Orbital fractures: role of imaging". Seminars in Ultrasound, CT, and MR. 33 (5): 385–391. doi:10.1053/j.sult.2012.06.007. PMID 22964404.
- Dissanaike S, Shalhub S, Jurkovich GJ (December 2008). "The evaluation of pneumomediastinum in blunt trauma patients". The Journal of Trauma. 65 (6): 1340–1345. doi:10.1097/TA.0b013e318169cd24. PMID 19077624.
- Ng P, Chu C, Young N, Soo M (August 1996). "Imaging of orbital floor fractures". Australasian Radiology. 40 (3): 264–268. doi:10.1111/j.1440-1673.1996.tb00400.x. PMID 8826732.
- Soyuncu S, Enver S (October 2009). "Eyelid swelling and lucency in the skull radiograph". Annals of the Academy of Medicine, Singapore. 38 (10): 928. doi:10.47102/annals-acadmedsg.V38N10p928. PMID 19890593. S2CID 40338796.
- "[Fractures of the orbital floor]". Bulletin des Sociétés d'Ophtalmologie de France. 74 (1): 91–95. January 1974. PMID 4430076.
- Bars N, Atlay Y, Tülay E, Tanju G (May 2008). "Extensive subcutaneous emphysema and pneumomediastinum associated with blowout fracture of the medial orbital wall". The Journal of Trauma. 64 (5): 1366–1369. doi:10.1097/01.ta.0000235507.60878.3d. PMID 17514044.
- Chouliaras K, Bench E, Talving P, Strumwasser A, Benjamin E, Lam L, et al. (August 2015). "Pneumomediastinum following blunt trauma: Worth an exhaustive workup?". The Journal of Trauma and Acute Care Surgery. 79 (2): 188–193. doi:10.1097/TA.0000000000000714. PMID 26218684. S2CID 21832402.
- Linberg JV (August 1982). "Orbital emphysema complicated by acute central retinal artery occlusion: case report and treatment". Annals of Ophthalmology. 14 (8): 747–749. PMID 7125471.
- Olmstead D, Gelfand G, Anderson I, Kortbeek JB (2018). "A Case Report of Acute Airway Compromise due to Subcutaneous Emphysema". Case Reports in Medicine. 2018: 3103061. doi:10.1155/2018/3103061. PMC 6286736. PMID 30595698.
- Jatla KK, Enzenauer RW (1 January 2004). "Orbital fractures: a review of current literature". Current Surgery. 61 (1): 25–29. doi:10.1016/j.cursur.2003.08.003. PMID 14972167.
- Ellis E (November 2012). "Orbital trauma". Oral and Maxillofacial Surgery Clinics of North America. 24 (4): 629–648. doi:10.1016/j.coms.2012.07.006. PMID 22981078.
- Çınar E, Yüce B, Fece M, Küçükerdönmez FC (February 2019). "Periorbital Emphysema After Endoscopic Nasal Polyp Surgery". Turkish Journal of Ophthalmology. 49 (1): 47–50. doi:10.4274/tjo.galenos.2018.01460. PMC 6416481. PMID 30829026.
- Shinohara H, Shirota Y, Fujita K (December 2004). "Implication of differences in the incidence of orbital emphysema in ethmoidal and maxillary sinus fractures". Annals of Plastic Surgery. 53 (6): 565–569. doi:10.1097/01.sap.0000134538.44898.1f. PMID 15602254. S2CID 38798670.
- Delpachitra SN, Rahmel BB (October 2016). "Orbital fractures in the emergency department: a review of early assessment and management". Emergency Medicine Journal. 33 (10): 727–731. doi:10.1136/emermed-2015-205005. PMID 26358976. S2CID 26852304.
- Oluwole M, White P (March 1996). "Orbital floor fracture following nose blowing". Ear, Nose, & Throat Journal. 75 (3): 169–170. doi:10.1177/014556139607500313. PMID 8721022. S2CID 21943984.
- Muhammad JK, Simpson MT (August 1996). "Orbital emphysema and the medial orbital wall: a review of the literature with particular reference to that associated with indirect trauma and possible blindness". Journal of Cranio-Maxillo-Facial Surgery. 24 (4): 245–250. doi:10.1016/s1010-5182(96)80008-4. PMID 8880451.
- Hwang K, Kim DH, Lee HS (July 2011). "Orbital fracture due to high-pressure air injection". The Journal of Craniofacial Surgery. 22 (4): 1506–1507. doi:10.1097/SCS.0b013e31821d4c3a. PMID 21778848.
- Fleishman JA, Beck RW, Hoffman RO (November 1984). "Orbital emphysema as an ophthalmologic emergency". Ophthalmology. 91 (11): 1389–1391. doi:10.1016/s0161-6420(84)34135-5. PMID 6514309.
- Brady FA, Roser SM, Hieshima GB (July 1976). "Orbital emphysema". The British Journal of Oral Surgery. 14 (1): 65–71. doi:10.1016/0007-117x(76)90095-0. PMID 1066158.
- Jordan DR, White GL, Anderson RL, Thiese SM (August 1988). "Orbital emphysema: a potentially blinding complication following orbital fractures". Annals of Emergency Medicine. 17 (8): 853–855. doi:10.1016/s0196-0644(88)80571-7. PMID 3394993.
- Lloyd GA (December 1966). "Orbital emphysema". The British Journal of Radiology. 39 (468): 933–938. doi:10.1259/0007-1285-39-468-933. PMID 5954092.
- Birrer RB, Robinson T, Papachristos P (December 1994). "Orbital emphysema: how common, how significant?". Annals of Emergency Medicine. 24 (6): 1115–1118. doi:10.1016/s0196-0644(94)70241-1. PMID 7978593.
- Gonzalez F, Cal V, Elhendi W (July 2005). "Orbital emphysema after sneezing". Ophthalmic Plastic and Reconstructive Surgery. 21 (4): 309–311. doi:10.1097/01.iop.0000170415.93858.6f. PMID 16052149.
- Karapasias N (1 November 2013). "Post traumatic orbital emphysema | Radiology Case | Radiopaedia.org". Radiopaedia. Retrieved 15 April 2021.