Platelet-rich plasma
Platelet-rich plasma (PRP), also known as autologous conditioned plasma, is a concentrate of platelet-rich plasma protein derived from whole blood, centrifuged to remove red blood cells. Plasma is the liquid portion of whole blood. It is composed largely of water and proteins, and it provides a medium for red blood cells, white blood cells and platelets to circulate through the body. Platelets, also called thrombocytes, are cell fragments found in blood that have growth and healing functions.[1][2]
| Platelet-rich plasma | |
|---|---|
 Platelet-rich plasma injection into the hand | |
| MeSH | D053657 |
Though promoted to treat an array of medical problems, evidence for benefit is mixed as of 2020, with some evidence for use in certain conditions and against use in other conditions.[3][4]
As a concentrated source of blood plasma and autologous conditioned plasma, PRP contains several different growth factors and other cytokines that can stimulate healing of soft tissue and joints. There are some indications for use in sports medicine and orthopedics (acute muscle strains, tendinopathy and muscle-fascial injuries and osteoarthritis[5]), or dermatology (androgenic alopecia, wound healing, and skin rejuvenation) or even in proctology (fistula-in-ano[6]).[7] For preparation of PRP, various protocols are used, with an underlying principle of concentrating platelets to 3–5 times physiological levels, then injecting this concentrate in the tissue where healing is desired.[8] Besides the use in clinical practice PRP has been utilized for various tissue engineering applications in the context of bone, cartilage, skin, and soft tissue repair. It has been reviewed to serve as a source for the "delivery of growth factors and/or cells within tissue-engineered constructs, often in combination with biomaterials".[9]
Medical use
Evidence for benefit of PRP is mixed, with some evidence for use in certain conditions and against use in other conditions.[10][11][4] It has been investigated for chronic tendinitis,[12] osteoarthritis,[13] in oral surgery,[14] and in plastic surgery.[15]
Elbow Tendinitis
A 2022 study from the Journal of Clinical Medicine compared PRP injections to physical therapy. They found that PRP lowered pain scores and increased elbow function significantly.[16] A 2022 study examined the effectiveness of PRP for elbow tendinopathy. They found that PRP was effective and that the concentration of the platelets and healing factors such as epidermal growth factor (EGF) were correlated with success of treatment.[17]
A 2022 meta-analysis examined 26 studies on PRP for elbow tendinopathy. They found that PRP treated patients rated their results significantly better using validated patient rated outcomes measures.[18] A 2021 systematic review by the Cochrane Library examined PRP and autologous whole blood injections and concluded that it was "uncertain" if PRP or autologous whole blood injections improved elbow tendon healing.[19]
A 2018 systematic review and meta-analysis of high quality studies found that PRP was beneficial for treatment of lateral epicondylitis.[20]
Numerous systematic reviews and meta-analyses have found that for elbow tendinopathy, PRP is superior to cortisone injections.[21][22][23][24][25] It has been shown to have similar[26] or equal[27][28] effects compared to surgery.
Rotator Cuff Disease
A 2022 systematic review and meta-analysis showed improved patient rated outcomes in patients with partial rotator cuff tears. At 8 weeks post injection, they found PRP to be effective.[29] A 2021 prospective study examined the effectiveness of PRP for partial thickness rotator cuff tears. Patients were given 2 separate PRP injections and followed for 2 years. The study noted: “No adverse events were seen in any patient. Based on global rating scores positive results were seen in 77.9 % of patients at 6 months, 71.6 % at 1 year, and 68.8 % of patients at 2 years”. They found PRP most effective in more damaged tendons.[30] A 2021 meta-analysis found that PRP was effective for partial rotator cuff tears but the effects were no longer evident at 1 year.[31]
PRP has been shown to be superior to cortisone injections in several studies.[32] This is especially evident in the longer term.[33][34]
A 2019 review found it not to be useful in rotator cuff disease.[4] A 2019 meta-analysis found that, for most outcomes in Achilles tendinopathy, PRP treatment did not differ from placebo treatment.[35] A 2018 review found that it may be useful.[20] A 2009 review found few randomized controlled trials that adequately evaluated the safety and efficacy of PRP treatments and concluded that PRP was "a promising, but not proven, treatment option for joint, tendon, ligament, and muscle injuries".[36]
Osteoarthritis
Tentative evidence supports its use in osteoarthritis (OA) of the knee.[37][38] A 2019 meta-analysis found that PRP might be more effective in reducing pain and improving function than hyaluronic acid in knee OA.[39]
Dental
A 2010 Cochrane review of use in sinus lifts during dental implant placement found no evidence of benefit.[14] A 2013 review stated more evidence was needed to determine effectiveness for hair regrowth.[40]
Other Musculoskeletal
A 2014 Cochrane review of PRP in musculoskeletal injuries found very weak evidence for a decrease in pain in the short term, and no difference in function in the short, medium or long term. It has not been shown to be useful for bone healing.[41] A 2016 review of PRP use to augment bone graft found only one study reporting a difference in bone augmentation, while four studies found no difference.[42] As compared to other conservative treatments for non-surgical orthopedic illnesses (e.g. steroid injection for plantar fasciitis), evidence does not support the use of PRP as a conservative treatment.[43] A 2018 review found that evidence was lacking for Achilles tendinopathy.[44]
Hair Loss
PRP is beneficial for alopecia areata[45] and androgenetic alopecia and can be used as an alternative to minoxidil or finasteride.[46] It has been documented to improve hair density and thickness in both genders.[47] A minimum of 3 treatments, once a month for 3 months are recommended, and afterwards a 3-6 month period of continual appointments for maintenance.[48] Factors that determine efficacy include amount of sessions, double versus single centrifugation, age and gender, and where the PRP is inserted.[49]
Future larger randomized controlled trials and other high quality studies are still recommended to be carried out and published for a stronger consensus.[50][47][51] Further development of a standardized practice for procedure is also recommended.[45]
Adverse effects
Adverse effects have been rarely reported to be low in most trials. A 2017 systematic review of the literature did not report of the types and number of adverse events.[52] Health Canada states PRP treatments harvested from, and given back to, the same person (in a single procedure) was not covered by its initial guidance as the procedure falls under health care provider regulatory bodies (rather than Health Canada).[53] There was weak evidence that suggested that harm occurred at comparable, low rates in treated and untreated people.[54][19] Similarly, another 2017 review for treating pain on skin graft donor sites found the evidence for benefit was poor.[55]
Composition

There are three general categories of preparation of PRP based on its leukocyte and fibrin content: leukocyte-rich PRP (L-PRP), leukocyte reduced PRP (P-PRP; leukocyte reduced or pure PRP), leukocyte platelet-rich fibrin.[8][56]
The efficacy of certain growth factors in healing various injuries and the concentrations of these growth factors found within PRP are the theoretical basis for the use of PRP in tissue repair.[57] Though not required for the process, The platelets collected in PRP can be activated by the addition of thrombin or calcium chloride, which induces the release of the mentioned factors from alpha granules. The addition of Thrombin or Calcium Chloride is not required as the bodies natural thrombin will activate the cells upon injection. The growth factors and other cytokines present in PRP include:[57][58][59][60]
- platelet-derived growth factor
- transforming growth factor beta
- fibroblast growth factor
- insulin-like growth factor 1
- insulin-like growth factor 2
- vascular endothelial growth factor A
- vascular endothelial growth factor C
- epidermal growth factor
- Interleukin 8
- keratinocyte growth factor
- connective tissue growth factor
- Hepatocyte growth factor
- Stromal cell-derived factor 1
- Endostatin
Manufacturing
PRP is prepared by taking blood from the person, and then putting it through centrifugation designed to separate PRP from platelet-poor plasma and red blood cells. This is usually done by the clinic offering the treatment, using commercially available kits and equipment.[61] The resulting substance varies from person to person and from facility to facility, making it difficult to understand how safe and effective any specific use is.[61][62]
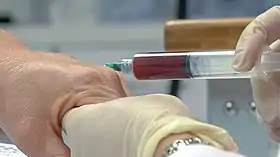
 Blood drawn from patient
Blood drawn from patient Removal of PRP after double centrifugation
Removal of PRP after double centrifugation PRP is Injected into area of injury via ultrasound guidance
PRP is Injected into area of injury via ultrasound guidance
Society and culture
PRP has received attention in the popular media[63][64][65] as a result of its use by athletes.[66] Use in an office setting is not approved by the FDA.[67]
In the 2010s, contentious cosmetic procedures marketed under the name of "vampire facials" grew in popularity, fueled by celebrity endorsement. These "vampire facials" generally center on PRP treatment, and usually (but not always) involve microneedling.[68][69]
PRP has also been injected into the vagina, in a procedure called "O-shot[70]" or "orgasm shot", with claims that this will improve orgasms.[71] There is no evidence, however, to support these claims.[71][72]
Doping
Some concern exists as to whether PRP treatments violate anti-doping rules.[57] As of 2010, it was not clear if local injections of PRP could have a systemic impact on circulating cytokine levels, affecting doping tests and whether PRP treatments have systemic anabolic effects or affect performance.[57] In January 2011, the World Anti-Doping Agency removed intramuscular injections of PRP from its prohibitions after determining that there is a "lack of any current evidence concerning the use of these methods for purposes of performance enhancement".[73]
History
In the early 1940s clinicians used extracts of growth factors and cytokines for healing. The term 'platet-rich plasma' was first used in 1954 by Kingsley and in the 1960s the first PRP blood banks were established, becoming popular by the 1970s.[74] In the 1970s PRP was used in the field of hematology, originally for transfusions to treat thrombocytopenia. Ten years later it was used for maxillofacial surgeries.[7] PRP was first used in Italy in 1987 in an open heart surgery procedure.[75] In 2006 PRP was starting to be considered of potential use for both androgenic alopecia and alopecia areata, though research remained mixed.[7]
See also
References
- Belk, JW; Kraeutler, MJ; Houck, DA; Goodrich, JA; Dragoo, JL; McCarty, EC (17 April 2020). "Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-analysis of Randomized Controlled Trials". The American Journal of Sports Medicine. 49 (1): 249–260. doi:10.1177/0363546520909397. PMID 32302218. S2CID 215809299.
- "Platelet Rich Plasma". KHT. Retrieved 2023-08-21.
- Belk, JW; Kraeutler, MJ; Houck, DA; Goodrich, JA; Dragoo, JL; McCarty, EC (17 April 2020). "Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-analysis of Randomized Controlled Trials". The American Journal of Sports Medicine. 49 (1): 249–260. doi:10.1177/0363546520909397. PMID 32302218. S2CID 215809299.
- Hurley, ET; Hannon, CP; Pauzenberger, L; Fat, DL; Moran, CJ; Mullett, H (May 2019). "Nonoperative Treatment of Rotator Cuff Disease With Platelet-Rich Plasma: A Systematic Review of Randomized Controlled Trials". Arthroscopy: The Journal of Arthroscopic & Related Surgery. 35 (5): 1584–1591. doi:10.1016/j.arthro.2018.10.115. PMID 31000394. S2CID 122575307.
- Smith, Patrick A. (2016-04-01). "Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial". The American Journal of Sports Medicine. 44 (4): 884–891. doi:10.1177/0363546515624678. ISSN 1552-3365. PMID 26831629. S2CID 42338794.
- de la Portilla, F.; Segura-Sampedro, J. J.; Reyes-Díaz, M. L.; Maestre, M. V.; Cabrera, A. M.; Jimenez-Rodríguez, R. M.; Vázquez-Monchul, J. M.; Diaz-Pavón, J. M.; Padillo-Ruiz, F. J. (2017-07-29). "Treatment of transsphincteric fistula-in-ano with growth factors from autologous platelets: results of a phase II clinical trial". International Journal of Colorectal Disease. 32 (11): 1545–1550. doi:10.1007/s00384-017-2866-9. ISSN 1432-1262. PMID 28755243. S2CID 23285036.
- Alves, Rubina; Grimalt, Ramon (2017-07-06). "A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification". Skin Appendage Disorders. 4 (1): 18–24. doi:10.1159/000477353. ISSN 2296-9195. PMID 29457008. Retrieved 2022-07-20.
- Pavlovic V, Ciric M, Jovanovic V, Stojanovic P (2016). "Platelet Rich Plasma: a short overview of certain bioactive components". Open Medicine. 11 (1): 242–247. doi:10.1515/med-2016-0048. PMC 5329835. PMID 28352802.
- Lang, Siegmund; Loibl, Markus; Herrmann, Marietta (2018). "Platelet-Rich Plasma in Tissue Engineering: Hype and Hope". European Surgical Research. 59 (3–4): 265–275. doi:10.1159/000492415. ISSN 1421-9921. PMID 30244245. S2CID 52344177.
- Mohammed, W; Farah, S; Nassiri, M; McKenna, J (2020). "Therapeutic efficacy of platelet-rich plasma injection compared to corticosteroid injection in plantar fasciitis: A systematic review and meta-analysis". Journal of Orthopaedics. 22: 124–134. doi:10.1016/j.jor.2020.03.053. PMC 7177161. PMID 32336895.
- Lin, MT; Wei, KC; Wu, CH (28 March 2020). "Effectiveness of Platelet-Rich Plasma Injection in Rotator Cuff Tendinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Diagnostics. 10 (4): 189. doi:10.3390/diagnostics10040189. PMC 7235747. PMID 32231127.
- Mishra A, Woodall J, Vieira A (January 2009). "Treatment of tendon and muscle using platelet-rich plasma". Clinics in Sports Medicine. 28 (1): 113–25. doi:10.1016/j.csm.2008.08.007. PMID 19064169.
- Andia I, Sánchez M, Maffulli N (January 2012). "Joint pathology and platelet-rich plasma therapies". Expert Opinion on Biological Therapy. 12 (1): 7–22. doi:10.1517/14712598.2012.632765. PMID 22171664. S2CID 39322743.
- Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, Worthington H, Coulthard P (Spring 2010). "Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review". European Journal of Oral Implantology. 3 (1): 7–26. PMID 20467595.
- Por YC, Shi L, Samuel M, Song C, Yeow VK (May 2009). "Use of tissue sealants in face-lifts: a metaanalysis". Aesthetic Plastic Surgery. 33 (3): 336–9. doi:10.1007/s00266-008-9280-1. PMID 19089492. S2CID 26761928.
- Annaniemi, Juho Aleksi; Pere, Jüri; Giordano, Salvatore (2022-12-23). "Platelet-Rich Plasma Injections Decrease the Need for Any Surgical Procedure for Chronic Epicondylitis versus Conservative Treatment-A Comparative Study with Long-Term Follow-Up". Journal of Clinical Medicine. 12 (1): 102. doi:10.3390/jcm12010102. ISSN 2077-0383. PMC 9821066. PMID 36614903.
- Dejnek, Maciej; Moreira, Helena; Płaczkowska, Sylwia; Barg, Ewa; Reichert, Paweł; Królikowska, Aleksandra (2022-06-27). "Effectiveness of Lateral Elbow Tendinopathy Treatment Depends on the Content of Biologically Active Compounds in Autologous Platelet-Rich Plasma". Journal of Clinical Medicine. 11 (13): 3687. doi:10.3390/jcm11133687. ISSN 2077-0383. PMC 9267331. PMID 35806972.
- Paramanantham, Madhavan; Seenappa, Hariprasad; Venkataraman, Sagar; Shanthappa, Arun H. (March 2022). "Functional Outcome of Platelet-Rich Plasma (PRP) Intra-lesional Injection for Tennis Elbow - A Prospective Cohort Study". Cureus. 14 (3): e22974. doi:10.7759/cureus.22974. ISSN 2168-8184. PMC 8990042. PMID 35415041.
- Karjalailen, Teemu (September 30, 2021). "Autologous blood and platelet‐rich plasma injection therapy for lateral elbow pain". Cochrane Database of Systematic Reviews. 2021 (9): CD010951. doi:10.1002/14651858.CD010951.pub2. PMC 8481072. PMID 34590307.
- Chen, Xiao; Jones, Ian A.; Park, Caron; Vangsness, C. Thomas (July 2018). "The Efficacy of Platelet-Rich Plasma on Tendon and Ligament Healing: A Systematic Review and Meta-analysis With Bias Assessment". The American Journal of Sports Medicine. 46 (8): 2020–2032. doi:10.1177/0363546517743746. ISSN 1552-3365. PMC 6339617. PMID 29268037.
- Klifto, Kevin M.; Colbert, Stephen H.; Richard, Marc J.; Anakwenze, Oke A.; Ruch, David S.; Klifto, Christopher S. (May 2022). "Platelet-rich plasma vs. corticosteroid injections for the treatment of recalcitrant lateral epicondylitis: a cost-effectiveness Markov decision analysis". Journal of Shoulder and Elbow Surgery. 31 (5): 991–1004. doi:10.1016/j.jse.2021.12.010. ISSN 1532-6500. PMID 35031496. S2CID 245900117.
- Kemp, Jordyn A.; Olson, Megan A.; Tao, Matthew A.; Burcal, Christopher J. (2021-06-01). "Platelet-Rich Plasma versus Corticosteroid Injection for the Treatment of Lateral Epicondylitis: A Systematic Review of Systematic Reviews". International Journal of Sports Physical Therapy. 16 (3): 597–605. doi:10.26603/001c.24148. ISSN 2159-2896. PMC 8169032. PMID 34123513.
- Li, Ang; Wang, Hongbo; Yu, Zhenghong; Zhang, Guangquan; Feng, Shiqing; Liu, Liyun; Gao, Yanzheng (December 2019). "Platelet-rich plasma vs corticosteroids for elbow epicondylitis: A systematic review and meta-analysis". Medicine. 98 (51): e18358. doi:10.1097/MD.0000000000018358. ISSN 1536-5964. PMC 6940118. PMID 31860992.
- Houck, Darby A.; Kraeutler, Matthew J.; Thornton, Loree B.; McCarty, Eric C.; Bravman, Jonathan T. (March 2019). "Treatment of Lateral Epicondylitis With Autologous Blood, Platelet-Rich Plasma, or Corticosteroid Injections: A Systematic Review of Overlapping Meta-analyses". Orthopaedic Journal of Sports Medicine. 7 (3): 2325967119831052. doi:10.1177/2325967119831052. ISSN 2325-9671. PMC 6419259. PMID 30899764.
- Arirachakaran, Alisara; Sukthuayat, Amnat; Sisayanarane, Thaworn; Laoratanavoraphong, Sorawut; Kanchanatawan, Wichan; Kongtharvonskul, Jatupon (June 2016). "Platelet-rich plasma versus autologous blood versus steroid injection in lateral epicondylitis: systematic review and network meta-analysis". Journal of Orthopaedics and Traumatology. 17 (2): 101–112. doi:10.1007/s10195-015-0376-5. ISSN 1590-9999. PMC 4882297. PMID 26362783.
- Hardy, Richard; Tori, Aerika; Fuchs, Hannah; Larson, Taiyo; Brand, Jefferson; Monroe, Emily (November 2021). "To Improve Pain and Function, Platelet-Rich Plasma Injections May Be an Alternative to Surgery for Treating Lateral Epicondylitis: A Systematic Review". Arthroscopy: The Journal of Arthroscopic & Related Surgery. 37 (11): 3360–3367. doi:10.1016/j.arthro.2021.04.043. ISSN 1526-3231. PMID 33957212. S2CID 233982749.
- Kim, Chul-Ho; Park, Yong-Beom; Lee, Jae-Sung; Jung, Hyoung-Seok (February 2022). "Platelet-rich plasma injection vs. operative treatment for lateral elbow tendinosis: a systematic review and meta-analysis". Journal of Shoulder and Elbow Surgery. 31 (2): 428–436. doi:10.1016/j.jse.2021.09.008. ISSN 1532-6500. PMID 34656779. S2CID 239019467.
- Boden, Allison L.; Scott, Michael T.; Dalwadi, Poonam P.; Mautner, Kenneth; Mason, R. Amadeus; Gottschalk, Michael B. (January 2019). "Platelet-rich plasma versus Tenex in the treatment of medial and lateral epicondylitis". Journal of Shoulder and Elbow Surgery. 28 (1): 112–119. doi:10.1016/j.jse.2018.08.032. ISSN 1532-6500. PMID 30551782. S2CID 54632733.
- Zhu, Pengfei; Wang, Zhengchao; Li, Hongmei; Cai, Yu (2022-09-16). "Platelet-Rich Plasma Injection in Non-Operative Treatment of Partial-Thickness Rotator Cuff Tears: A Systematic Review and Meta-Analysis". Journal of Rehabilitation Medicine. 54: jrm00312. doi:10.2340/jrm.v54.1434. ISSN 1651-2081. PMC 9495266. PMID 35892292.
- Prodromos, Chadwick C.; Finkle, Susan; Prodromos, Alexandra; Chen, Jasmine Li; Schwartz, Aron; Wathen, Lucas (2021-05-29). "Treatment of Rotator Cuff Tears with platelet rich plasma: a prospective study with 2 year follow-up". BMC Musculoskeletal Disorders. 22 (1): 499. doi:10.1186/s12891-021-04288-4. ISSN 1471-2474. PMC 8164813. PMID 34051761.
- Xiang, Xiao-Na; Deng, Jie; Liu, Yan; Yu, Xi; Cheng, Biao; He, Hong-Chen (December 2021). "Conservative treatment of partial-thickness rotator cuff tears and tendinopathy with platelet-rich plasma: A systematic review and meta-analysis". Clinical Rehabilitation. 35 (12): 1661–1673. doi:10.1177/02692155211011944. ISSN 1477-0873. PMID 33896214. S2CID 229348580.
- Kwong, Cory A.; Woodmass, Jarret M.; Gusnowski, Eva M.; Bois, Aaron J.; Leblanc, Justin; More, Kristie D.; Lo, Ian K. Y. (February 2021). "Platelet-Rich Plasma in Patients With Partial-Thickness Rotator Cuff Tears or Tendinopathy Leads to Significantly Improved Short-Term Pain Relief and Function Compared With Corticosteroid Injection: A Double-Blind Randomized Controlled Trial". Arthroscopy: The Journal of Arthroscopic & Related Surgery. 37 (2): 510–517. doi:10.1016/j.arthro.2020.10.037. ISSN 1526-3231. PMID 33127554. S2CID 226217973.
- Kim, Sang Jun; Kim, Eun Kyung; Kim, Sun Jeong; Song, Da Hyun (2018-01-03). "Effects of bone marrow aspirate concentrate and platelet-rich plasma on patients with partial tear of the rotator cuff tendon". Journal of Orthopaedic Surgery and Research. 13 (1): 1. doi:10.1186/s13018-017-0693-x. ISSN 1749-799X. PMC 5753487. PMID 29298726.
- Giovannetti de Sanctis, Edoardo; Franceschetti, Edoardo; De Dona, Ferdinando; Palumbo, Alessio; Paciotti, Michele; Franceschi, Francesco (2020-12-25). "The Efficacy of Injections for Partial Rotator Cuff Tears: A Systematic Review". Journal of Clinical Medicine. 10 (1): 51. doi:10.3390/jcm10010051. ISSN 2077-0383. PMC 7795404. PMID 33375716.
- Liu, Chun-jie; Yu, Kun-lun; Bai, Jiang-bo; Tian, De-hu; Liu, Guo-li (April 2019). "Platelet-rich plasma injection for the treatment of chronic Achilles tendinopathy: A meta-analysis". Medicine. 98 (16): e15278. doi:10.1097/MD.0000000000015278. ISSN 0025-7974. PMC 6494278. PMID 31008973.
- Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA (November 2009). "Platelet-rich plasma: from basic science to clinical applications". The American Journal of Sports Medicine. 37 (11): 2259–72. doi:10.1177/0363546509349921. PMID 19875361. S2CID 5914979.
- Dai WL, Zhou AG, Zhang H, Zhang J (March 2017). "Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Trials". Arthroscopy. 33 (3): 659–670.e1. doi:10.1016/j.arthro.2016.09.024. PMID 28012636.
- Shen L, Yuan T, Chen S, Xie X, Zhang C (January 2017). "The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials". Journal of Orthopaedic Surgery and Research. 12 (1): 16. doi:10.1186/s13018-017-0521-3. PMC 5260061. PMID 28115016.
- Han, Yanhong; Huang, Hetao; Pan, Jianke; Lin, Jiongtong; Zeng, Lingfeng; Liang, Guihong; Yang, Weiyi; Liu, Jun (July 1, 2019). "Meta-analysis Comparing Platelet-Rich Plasma vs Hyaluronic Acid Injection in Patients with Knee Osteoarthritis". Pain Medicine (Malden, Mass.). 20 (7): 1418–1429. doi:10.1093/pm/pnz011. ISSN 1526-4637. PMC 6611633. PMID 30849177.
- Valente Duarte de Sousa IC, Tosti A (May 2013). "New investigational drugs for androgenetic alopecia". Expert Opinion on Investigational Drugs. 22 (5): 573–89. doi:10.1517/13543784.2013.784743. PMID 23550739. S2CID 21653303.
- Griffin XL, Smith CM, Costa ML (February 2009). "The clinical use of platelet-rich plasma in the promotion of bone healing: a systematic review". Injury. 40 (2): 158–62. doi:10.1016/j.injury.2008.06.025. PMID 19084836.
- Pocaterra A, Caruso S, Bernardi S, Scagnoli L, Continenza MA, Gatto R (August 2016). "Effectiveness of platelet-rich plasma as an adjunctive material to bone graft: a systematic review and meta-analysis of randomized controlled clinical trials". International Journal of Oral and Maxillofacial Surgery. 45 (8): 1027–34. doi:10.1016/j.ijom.2016.02.012. PMID 26987695.
- Franchini M, Cruciani M, Mengoli C, Marano G, Pupella S, Veropalumbo E, Masiello F, Pati I, Vaglio S, Liumbruno GM (November 2018). "Efficacy of platelet-rich plasma as conservative treatment in orthopaedics: a systematic review and meta-analysis". Blood Transfusion = Trasfusione del Sangue. 16 (6): 502–513. doi:10.2450/2018.0111-18. PMC 6214820. PMID 30201082.
- Zhang, YJ; Xu, SZ; Gu, PC; Du, JY; Cai, YZ; Zhang, C; Lin, XJ (August 2018). "Is Platelet-rich Plasma Injection Effective for Chronic Achilles Tendinopathy? A Meta-analysis". Clinical Orthopaedics and Related Research. 476 (8): 1633–1641. doi:10.1007/s11999.0000000000000258. PMC 6259774. PMID 29601383.
- Tejapira, Kasama; Yongpisarn, Tanat; Sakpuwadol, Nawara; Suchonwanit, Poonkiat (2022-11-24). "Platelet-rich plasma in alopecia areata and primary cicatricial alopecias: A systematic review". Frontiers in Medicine. Frontiers Media SA. 9. doi:10.3389/fmed.2022.1058431. ISSN 2296-858X. PMC 9731377. PMID 36507528.
- Gentile, Pietro; Garcovich, Simone (2020-04-13). "Systematic Review of Platelet-Rich Plasma Use in Androgenetic Alopecia Compared with Minoxidil®, Finasteride®, and Adult Stem Cell-Based Therapy". International Journal of Molecular Sciences. MDPI AG. 21 (8): 2702. doi:10.3390/ijms21082702. ISSN 1422-0067. PMC 7216252. PMID 32295047.
- Evans, Adam G.; Mwangi, James M.; Pope, Rand W.; Ivanic, Mirjana G.; Botros, Mina A.; Glassman, Gabriella E.; Pearce, F. Bennett; Kassis, Salam (2020-05-26). "Platelet-rich plasma as a therapy for androgenic alopecia: a systematic review and meta-analysis". Journal of Dermatological Treatment. Informa UK Limited. 33 (1): 498–511. doi:10.1080/09546634.2020.1770171. ISSN 0954-6634. PMID 32410524. S2CID 218648227.
- Gupta, Aditya K.; Cole, John; Deutsch, David P.; Everts, Peter A.; Niedbalski, Robert P.; Panchaprateep, Ratchathorn; Rinaldi, Fabio; Rose, Paul T.; Sinclair, Rodney; Vogel, James E.; Welter, Ryan J.; Zufelt, Michael D.; Puig, Carlos J. (2019). "Platelet-Rich Plasma as a Treatment for Androgenetic Alopecia". Dermatologic Surgery. Ovid Technologies (Wolters Kluwer Health). 45 (10): 1262–1273. doi:10.1097/dss.0000000000001894. ISSN 1076-0512. PMID 30882509. S2CID 81980415.
- Gupta, Aditya; Bamimore, Mary (2022-08-01). "Platelet-Rich Plasma Monotherapies for Androgenetic Alopecia: A Network Meta-Analysis and Meta-Regression Study". Journal of Drugs in Dermatology. SanovaWorks. 21 (9): 943–952. doi:10.36849/jdd.6948. ISSN 1545-9616. PMID 36074501. S2CID 252120370.
- Gupta, Aditya K.; Bamimore, Mary A.; Foley, Kelly A. (2020-04-13). "Efficacy of non-surgical treatments for androgenetic alopecia in men and women: a systematic review with network meta-analyses, and an assessment of evidence quality". Journal of Dermatological Treatment. Informa UK Limited. 33 (1): 62–72. doi:10.1080/09546634.2020.1749547. ISSN 0954-6634. PMID 32250713. S2CID 215405183.
- Oth, O; Stene, JJ; Glineur, R; Vujovic, A (2018). "Injection of PRP (Platelet-rich plasma) as a treatment for androgenetic alopecia : a systematic review of the literature". Revue Médicale de Bruxelles. AMUB/Revue Médicale de Bruxelles. 39 (5): 438–446. doi:10.30637/2018.17-056. ISSN 0035-3639. PMID 29869472.
- Frautschi RS, Hashem AM, Halasa B, Cakmakoglu C, Zins JE (March 2017). "Current Evidence for Clinical Efficacy of Platelet Rich Plasma in Aesthetic Surgery: A Systematic Review". Aesthetic Surgery Journal. 37 (3): 353–362. doi:10.1093/asj/sjw178. PMID 28207031.
- "Health Canada clarifies position on Platelet Rich Plasma treatments". Health Canada. Health Canada. 26 July 2019. Retrieved 7 January 2020.
- Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC (April 2014). "Platelet-rich therapies for musculoskeletal soft tissue injuries". The Cochrane Database of Systematic Reviews. 29 (4): CD010071. doi:10.1002/14651858.CD010071.pub3. PMC 6464921. PMID 24782334.
- Sinha S, Schreiner AJ, Biernaskie J, Nickerson D, Gabriel VA (November 2017). "Treating pain on skin graft donor sites: Review and clinical recommendations". The Journal of Trauma and Acute Care Surgery. 83 (5): 954–964. doi:10.1097/TA.0000000000001615. PMID 28598907. S2CID 44520644.
- Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A (June 2012). "The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: new perspectives". Current Pharmaceutical Biotechnology. 13 (7): 1153–62. doi:10.2174/138920112800624373. PMID 21740376.
- Borrione P, Gianfrancesco AD, Pereira MT, Pigozzi F (October 2010). "Platelet-rich plasma in muscle healing". American Journal of Physical Medicine & Rehabilitation. 89 (10): 854–61. doi:10.1097/PHM.0b013e3181f1c1c7. PMID 20855985.
- Yu W, Wang J, Yin J (April 2011). "Platelet-rich plasma: a promising product for treatment of peripheral nerve regeneration after nerve injury". The International Journal of Neuroscience. 121 (4): 176–80. doi:10.3109/00207454.2010.544432. PMID 21244302. S2CID 26837842.
- Wartiovaara, U.; Salven, P.; Mikkola, H.; Lassila, R.; Kaukonen, J.; Joukov, V.; Orpana, A.; Ristimäki, A.; Heikinheimo, M.; Joensuu, H.; Alitalo, K.; Palotie, A. (July 1998). "Peripheral blood platelets express VEGF-C and VEGF which are released during platelet activation". Thrombosis and Haemostasis. 80 (1): 171–175. doi:10.1055/s-0037-1615158. ISSN 0340-6245. PMID 9684805. S2CID 795299.
- Custo, S; Baron, B; Felice, a; Seria (5 July 2022). "A comparative profile of total protein and six angiogenically-active growth factors in three platelet products". GMS Interdisciplinary Plastic and Reconstructive Surgery DGPW. 11 (Doc06). doi:10.3205/iprs000167. PMC 9284722. PMID 35909816.
- Dhurat R, Sukesh M (2014). "Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author's Perspective". Journal of Cutaneous and Aesthetic Surgery. 7 (4): 189–97. doi:10.4103/0974-2077.150734. PMC 4338460. PMID 25722595.
- Kanchanatawan W, Arirachakaran A, Chaijenkij K, Prasathaporn N, Boonard M, Piyapittayanun P, Kongtharvonskul J (May 2016). "Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee". Knee Surgery, Sports Traumatology, Arthroscopy. 24 (5): 1665–77. doi:10.1007/s00167-015-3784-4. PMID 26387122. S2CID 35221300.
- Schwarz A (2009-02-16). "A Promising Treatment for Athletes, in Blood". New York Times. New York.
- Kolata G (2010-01-12). "Popular Blood Therapy May Not Work". New York Times.
- Reynolds G (2011-01-26). "Phys Ed: Does Platelet-Rich Plasma Therapy Really Work?". New York Times.
- Storrs C (2009-12-18). "Is Platelet-Rich Plasma an Effective Healing Therapy?". Scientific American.
- Beitzel K, Allen D, Apostolakos J, Russell RP, McCarthy MB, Gallo GJ, Cote MP, Mazzocca AD (February 2015). "US definitions, current use, and FDA stance on use of platelet-rich plasma in sports medicine". The Journal of Knee Surgery. 28 (1): 29–34. doi:10.1055/s-0034-1390030. PMID 25268794.
- Georgiou, Aristos (14 September 2018). "What is a vampire facial?". Newsweek. Retrieved 29 March 2019.
- "What it's really like to get the infamous vampire facial". The Independent. 28 February 2018. Retrieved 29 March 2019.
- "O Shot in San Diego". The Independent. 28 February 2023. Retrieved 17 January 2023.
- Osborne, Hannah (8 July 2016). "Injecting blood plasma into your clitoris for $2,500 won't give you with better orgasms". International Business Times UK. Retrieved 1 October 2018.
- Goodman, Michael P. (2016). Female Genital Plastic and Cosmetic Surgery. John Wiley & Sons. p. PT391. ISBN 9781118848487.
There is presently no information in peer reviewed literature.
- "World Anti-Doping Agency announces changes to Prohibited List". Irish Medical Times. 2011-01-10.
- Mościcka, Patrycja; Przylipiak, Andrzej (2021-07-14). "History of autologous platelet‐rich plasma: A short review". Journal of Cosmetic Dermatology. Wiley. 20 (9): 2712–2714. doi:10.1111/jocd.14326. ISSN 1473-2130. PMC 9291029. PMID 34214233.
- Ferrari M, Zia S, Valbonesi M, Henriquet F, Venere G, Spagnolo S, Grasso MA, Panzani I. A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Organs. 1987 Jan;10(1):47-50. PMID 3570542