Post-traumatic arthritis
Post-traumatic arthritis (PTA) is a form of osteoarthritis following an injury to a joint.[1]
| Post-traumatic arthritis | |
|---|---|
| Other names | Post-traumatic osteoarthritis, post-traumatic inflammatory arthritis |
 | |
| Post-traumatic arthritis of the wrist | |
| Specialty | Orthopedics |
| Symptoms | stiffness, swelling, synovial effusion, pain, redness, tenderness, grinding, instability, intra-articular bleeding |
| Types | Post-traumatic osteoarthritis, post-traumatic inflammatory arthritis |
| Causes | Physical injury |
| Risk factors | Overweight, physical activity, injuries |
| Diagnostic method | Medical history, X-ray |
| Treatment | Medication, surgery, physical therapy |
| Medication | NSAIDs, cortisone, paracetamol, corticosteroid |
| Frequency | Over 5.6 million people in the US |
Classification
Post-traumatic arthritis is a form of osteoarthritis and the former can occur after the latter. However, post-traumatic arthritis can also occur after the development of chronic inflammatory arthritis.
Generally, post-traumatic arthritis is classified in two groups: post-traumatic osteoarthritis and post-traumatic inflammatory arthritis.[2]
Post-traumatic osteoarthritis
Post-traumatic osteoarthritis is the most common variation of post-traumatic arthritis.[3] Between 20 and 50%[4] of all osteoarthritis cases are preceded by post-traumatic arthritis. Patients having post-traumatic osteoarthritis are usually younger than osteoarthritis patients without any previous physical injuries.[5]
Post-traumatic inflammatory arthritis
Less common is post-traumatic inflammatory arthritis, accounting for between 2 and 25% of all post-traumatic arthritis cases.[6] There are reports about a connection between previous physical injury and inflammatory arthritis, such as rheumatoid arthritis[7][8] or psoriatic arthritis.[9][10]
Signs and symptoms
The symptoms of post-traumatic arthritis are similar to the ones occurring with osteoarthritis. General symptoms are stiffness, swelling, synovial effusion, pain, redness, tenderness, grinding, instability and intra-articular bleeding of the injured joint.[1][11]
As a result of these symptoms, post-traumatic arthritis often comes along with the loss of ability.
Risk factors
Since post-traumatic arthritis usually occurs after injuring a joint, the risk of having post-traumatic arthritis after such an injury is significant higher. Risk factors which increase the danger of getting post-traumatic arthritis are being overweight and physical activity.[12] The prevalence of post-traumatic arthritis is much higher when doing heavy work and overusing the injured joints. Examinations also revealed that a body mass index (BMI) increase of five units results in a 35% higher risk of post-traumatic arthritis.[13]
It is reported that genetics do have an influence on the prevalence of post-traumatic arthritis.[14][15] According to newer examinations, the sex of the patients may also have an influence on post-traumatic arthritis, since females are affected by post-traumatic arthritis more frequently than males.[16]
Pathogenesis
The process of post-traumatic arthritis can be divided into three phases: immediate, acute, and chronic.[1][17]
Immediate phase
This phase usually begins a few seconds after the injury; it is characterized by cell necrosis, collagen rupture, swelling of the cartilage, hemarthrosis, and the loss of glycosaminoglycans (GAGs).[1][18]
Acute phase
In this phase, acute post-traumatic arthrosis emerges. Matrix degradation, leukocyte infiltration, inflammatory mediators, deficient lubricants, and apoptosis can occur. Typically, the acute phase comes hours after the injury.[1][19]
Chronic phase
The chronic phase occurs months or years after the trauma. Typical symptoms are joint pain and dysfunction.[1][12]
Diagnosis
Post-traumatic arthritis is diagnosed with the help of a patient's medical history. Additionally, radiographic imaging can assist in diagnosing post-traumatic arthritis.[20]
Management
It is not possible to cure the acute post-traumatic arthritis in order to prevent a chronic post-traumatic arthritis.[1] There are many different options to manage chronic post-traumatic arthritis.[12]
Lifestyle
Since being overweight is a risk factor for post-traumatic arthritis, lifestyle changes that help manage body weight are important in the treatment and prevention of the condition. Lifestyle changes and weight loss often involve educating the affected person about how to practice a healthy lifestyle.[21]
Therapeutic measures
Physical therapy may help reduce pain and other symptoms of post-traumatic arthritis.[22] The efficacy of massage therapy[23] and manual therapy[24] are not yet proven.[22][23][24]
Medication
Post-traumatic arthritis is treated symptomatically with nonsteroidal anti-inflammatory drugs (NSAIDs).[1][12] For more moderate symptoms, paracetamol is also used.[25][26] Another medical treatment approach is the injection of cortisone or corticosteroid into the affected joint.[1][27]
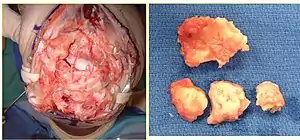
Surgery
If medications, lifestyle changes, and physical therapy are not enough to reduce the symptoms, especially the pain, surgery and other such interventions for managing post-traumatic arthritis are available. In many cases, joint replacement or cartilage resurfacing are recommended. As clinical studies have demonstrated, such surgical methods can be effective at reducing symptomatic pain[28][29] and the costs associated with management of the condition.[30][31]
Epidemiology
About 12% of all osteoarthritis cases in the United States are classified as post-traumatic osteoarthritis.[2] This means that over 5.6 million people are affected by post-traumatic osteoarthritis only in the United States.[2] Females are more often affected than males.[16]
Post-traumatic arthritis costs the US health care system approximately US$3.06 billion (0.15%) of total health care costs each year.[2]
References
- Punzi, Leonardo; Galozzi, Paola; Luisetto, Roberto; Favero, Marta; Ramonda, Roberta; Oliviero, Francesca; Scanu, Anna (6 September 2016). "Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation". RMD Open. 2 (2): e000279. doi:10.1136/rmdopen-2016-000279. PMC 5013366. PMID 27651925.
- Brown, Thomas D.; Johnston, Richard C.; Saltzman, Charles L.; Marsh, J. Lawrence; Buckwalter, Joseph A. (November 2006). "Posttraumatic Osteoarthritis: A First Estimate of Incidence, Prevalence, and Burden of Disease". Journal of Orthopaedic Trauma. 20 (10): 739–44. doi:10.1097/01.bot.0000246468.80635.ef. PMID 17106388.
- Muthuri, S.G.; McWilliams, D.F.; Doherty, M.; Zhang, W. (2011-11-01). "History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies". Osteoarthritis and Cartilage. 19 (11): 1286–1293. doi:10.1016/j.joca.2011.07.015. PMID 21884811.
- Lohmander, L. Stefan; Englund, P. Martin; Dahl, Ludvig L.; Roos, Ewa M. (October 2007). "The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis". The American Journal of Sports Medicine. 35 (10): 1756–1769. doi:10.1177/0363546507307396. PMID 17761605.
- Gelber, A. C.; Hochberg, M. C.; Mead, L. A.; Wang, N. Y.; Wigley, F. M.; Klag, M. J. (2000-09-05). "Joint injury in young adults and risk for subsequent knee and hip osteoarthritis". Annals of Internal Medicine. 133 (5): 321–328. doi:10.7326/0003-4819-133-5-200009050-00007. PMID 10979876.
- Williams, K A; Scott, J T (November 1967). "Influence of trauma on the development of chronic inflammatory polyarthritis". Annals of the Rheumatic Diseases. 26 (6): 532–537. doi:10.1136/ard.26.6.532. PMC 1010439. PMID 6066236.
- Söderlin, Maria K.; Bergsten, Ulrika; Svensson, Björn; BARFOT Study Group (March 2011). "Patient-reported events preceding the onset of rheumatoid arthritis: possible clues to aetiology". Musculoskeletal Care. 9 (1): 25–31. doi:10.1002/msc.193. PMID 21351367.
- Malleson, P (May 1997). "Management of childhood arthritis. Part 1: acute arthritis". Archives of Disease in Childhood. 76 (5): 460–462. doi:10.1136/adc.76.5.460. PMC 1717186. PMID 9196369.
- Olivieri, Ignazio; Padula, Angela; D'Angelo, Salvatore; Scarpa, Raffaele (November 2008). "Role of trauma in psoriatic arthritis". The Journal of Rheumatology. 35 (11): 2085–2087. doi:10.3899/jrheum.080668. PMID 19004049.
- Punzi, L.; Pianon, M.; Bertazzolo, N.; Fagiolo, U.; Rizzi, E.; Rossini, P.; Todesco, S. (May 1998). "Clinical, laboratory and immunogenetic aspects of post-traumatic psoriatic arthritis: a study of 25 patients". Clinical and Experimental Rheumatology. 16 (3): 277–281X. PMID 9631749.
- "Post Traumatic Wrist Arthritis | Orthopaedic Surgery | Michigan Medicine | University of Michigan". medicine.umich.edu. Retrieved 2018-03-28.
- Anderson, Donald D.; Chubinskaya, Susan; Guilak, Farshid; Martin, James A.; Oegema, Theodore R.; Olson, Steven A.; Buckwalter, Joseph A. (2011-06-01). "Post-traumatic osteoarthritis: Improved understanding and opportunities for early intervention". Journal of Orthopaedic Research. 29 (6): 802–809. doi:10.1002/jor.21359. PMC 3082940. PMID 21520254.
- Jiang L, Tian W, Wang Y, Rong J, Bao C, Liu Y, Zhao Y, Wang C (May 2012). "Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis". Joint Bone Spine. 79 (3): 291–7. doi:10.1016/j.jbspin.2011.05.015. PMID 21803633.
- Valdes, Ana M; Doherty, Sally A; Muir, Kenneth R; Wheeler, Margaret; Maciewicz, Rose A; Zhang, Weiya; Doherty, Michael (2013). "The genetic contribution to severe post-traumatic osteoarthritis". Annals of the Rheumatic Diseases. 72 (10): 1687–1690. doi:10.1136/annrheumdis-2012-202562. PMC 3786638. PMID 23355107.
- Spector TD, MacGregor AJ (2004). "Risk factors for osteoarthritis: genetics". Osteoarthritis and Cartilage. 12 Suppl A: S39–44. doi:10.1016/j.joca.2003.09.005. PMID 14698640.
- Zhang Y, Jordan JM (August 2010). "Epidemiology of osteoarthritis". Clinics in Geriatric Medicine. 26 (3): 355–69. doi:10.1016/j.cger.2010.03.001. PMC 2920533. PMID 20699159.
- Lieberthal, Jason; Sambamurthy, Nisha; Scanzello, Carla R. (2015). "Inflammation in Joint Injury and Post-Traumatic Osteoarthritis". Osteoarthritis and Cartilage. 23 (11): 1825–1834. doi:10.1016/j.joca.2015.08.015. PMC 4630675. PMID 26521728.
- Swärd, P.; Frobell, R.; Englund, M.; Roos, H.; Struglics, A. (November 2012). "Cartilage and bone markers and inflammatory cytokines are increased in synovial fluid in the acute phase of knee injury (hemarthrosis)—a cross-sectional analysis". Osteoarthritis and Cartilage. 20 (11): 1302–1308. doi:10.1016/j.joca.2012.07.021. PMID 22874525.
- Heard, B. J.; Solbak, N. M.; Achari, Y.; Chung, M.; Hart, D. A.; Shrive, N. G.; Frank, C. B. (December 2013). "Changes of early post-traumatic osteoarthritis in an ovine model of simulated ACL reconstruction are associated with transient acute post-injury synovial inflammation and tissue catabolism". Osteoarthritis and Cartilage. 21 (12): 1942–1949. doi:10.1016/j.joca.2013.08.019. PMID 24012772.
- Bierma-Zeinstra, Sita M. A.; Oster, J. Dorinde; Bernsen, Roos M. D.; Verhaar, Jan A. N.; Ginai, Abida Z.; Bohnen, Arthur M. (August 2002). "Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care". The Journal of Rheumatology. 29 (8): 1713–1718X. PMID 12180735.
- Cibulka, Michael T.; White, Douglas M.; Woehrle, Judith; Harris-Hayes, Marcie; Enseki, Keelan; Fagerson, Timothy L.; Slover, James; Godges, Joseph J. (2009). "Hip Pain and Mobility Deficits – Hip Osteoarthritis". The Journal of Orthopaedic and Sports Physical Therapy. 39 (4): A1–25. doi:10.2519/jospt.2009.0301. PMC 3963282. PMID 19352008.
- Wang, Shi-Yi; Olson-Kellogg, Becky; Shamliyan, Tatyana A.; Choi, Jae-Young; Ramakrishnan, Rema; Kane, Robert L. (2012-11-06). "Physical Therapy Interventions for Knee Pain Secondary to Osteoarthritis: A Systematic Review". Annals of Internal Medicine. 157 (9): 632–44. doi:10.7326/0003-4819-157-9-201211060-00007. PMID 23128863.
- De Luigi, Arthur Jason (May 2012). "Complementary and alternative medicine in osteoarthritis 1". PM&R: The Journal of Injury, Function, and Rehabilitation. 4 (5 Suppl): S122–133. doi:10.1016/j.pmrj.2012.01.012. PMID 22632691.
- French, H. P.; Brennan, A.; White, B.; Cusack, T. (April 2011). "Manual therapy for osteoarthritis of the hip or knee – A systematic review". Manual Therapy. 16 (2): 109–117. doi:10.1016/j.math.2010.10.011. PMID 21146444.
- Flood J (March 2010). "The role of acetaminophen in the treatment of osteoarthritis". The American Journal of Managed Care. 16 Suppl Management: S48–54. PMID 20297877.
- Zhang, W.; Moskowitz, R. W.; Nuki, G.; Abramson, S.; Altman, R. D.; Arden, N.; Bierma-Zeinstra, S.; Brandt, K. D.; Croft, P. (September 2007). "OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence". Osteoarthritis and Cartilage. 15 (9): 981–1000. doi:10.1016/j.joca.2007.06.014. PMID 17719803.
- Arroll, Bruce; Goodyear-Smith, Felicity (2004-04-10). "Corticosteroid injections for osteoarthritis of the knee: meta-analysis". BMJ. 328 (7444): 869. doi:10.1136/bmj.38039.573970.7C. PMC 387479. PMID 15039276.
- Santaguida, Pasqualina L.; Hawker, Gillian A.; Hudak, Pamela L.; Glazier, Richard; Mahomed, Nizar N.; Kreder†, Hans J.; Coyte, Peter C.; Wright, James G. (2008). "Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review". Canadian Journal of Surgery. 51 (6): 428–436X. PMC 2592576. PMID 19057730.
- Carr, Andrew J; Robertsson, Otto; Graves, Stephen; Price, Andrew J; Arden, Nigel K; Judge, Andrew; Beard, David J (2012-04-07). "Knee replacement". The Lancet. 379 (9823): 1331–40. doi:10.1016/S0140-6736(11)60752-6. PMID 22398175.
- Jenkins, P. J.; Clement, N. D.; Hamilton, D. F.; Gaston, P.; Patton, J. T.; Howie, C. R. (January 2013). "Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis". The Bone & Joint Journal. 95-B (1): 115–121. doi:10.1302/0301-620X.95B1.29835. PMID 23307684.
- Daigle, Meghan E.; Weinstein, Alexander M.; Katz, Jeffrey N.; Losina, Elena (2012). "The cost-effectiveness of total joint arthroplasty: a systematic review of published literature". Best Practice & Research. Clinical Rheumatology. 26 (5): 649–58. doi:10.1016/j.berh.2012.07.013. PMC 3879923. PMID 23218429.