Precision cut lung slices
Precision cut lung slices or PCLS refer to thin sections of lung tissue that are prepared with high precision and are typically used for experimental purposes in the field of respiratory research.[1] These slices are utilized to study various aspects of lung physiology, pathology, and pharmacology, providing researchers with a valuable tool for investigating lung diseases and testing the effects of drugs on lung tissue.[2]
Precision cut lung slices are prepared using specialized equipment called Compresstome vibratomes, ensuring that the tissue remains viable and retains its structural and functional characteristics, making them ideal for a wide range of experimental applications.[3][4]
History
The history of Precision-cut Lung Slices (PCLS) dates back to the 1920s when scientists first explored tissue slices for studying organ metabolism and toxicology. Initially, manual slicing of tissues, such as the liver, led to significant variability in thickness and limited viability.[5]
A critical advancement occurred in the 1940s when Stadie and Riggs introduced a microtome equipped with a thin razor blade, reducing thickness variability to about 5%. These improved slices became known as precision-cut tissue slices.[6]
Creating PCLS posed unique challenges due to the lung's intricate structure. In the 1980s, Placke and Fisher achieved a breakthrough by infusing heated liquid agarose into the airways of hamster and rat lungs, preventing airway and alveolar collapse during slicing.[7]
Basic preparation
Creating Precision-cut Lung Slices (PCLS) is a meticulous process that involves several essential steps. The use of vibratomes is crucial in ensuring the production of precise and high-quality lung slices for research purposes.[8]
Use of vibratomes

The basic steps involved in preparing PCLS using Compresstome vibratomes include: [9]
- Tissue Selection
- Start by carefully selecting lung tissue from the desired species, such as rodents or humans, ensuring the tissue is of high quality and health.
- Tissue Embedding
- To facilitate slicing and maintain tissue structure, the lung tissue is typically embedded in a suitable medium, such as agarose or gelatin, into the specimen holder of the Compresstome vibratome.
- Slicing Process
- The vibratome operates by oscillating a blade vertically at high frequencies while the tissue is submerged in a cutting solution. This mechanical oscillation creates thin and precise slices of lung tissue. Researchers can adjust cutting parameters, such as slice thickness, to meet specific experimental requirements. Typically, PCLS have thicknesses ranging from 200-500µm.
- Post-processing
- Depending on the research objectives, PCLS may undergo additional steps such as washing, culturing, or treatment with substances of interest, such as drugs or stimuli.
Maintenance of PCLS
Ensuring the viability of Precision-cut Lung Slices (PCLS) during ex vivo maintenance presents several challenges. Typically, PCLS are submerged in culture medium within multi-well plates, simulating tissue culture conditions at 37 °C, 5% CO2, and 95–100% air humidity.[10] The culture medium is refreshed daily and optimized with essential nutrients, enabling viable PCLS to be maintained for up to 14 days, a significant improvement compared to previous reports of only 3–5 days.[11] Additionally, the inclusion of antibiotics like penicillin and streptomycin helps prevent pathogen contamination from the outset of culture.[12]
While in culture, PCLS retain their viability, normal metabolic activity, tissue integrity, and responsiveness to stimuli such as lipopolysaccharide (LPS).[11] However, it's important to note that extended culture periods may lead to some changes in PCLS function. For instance, although human PCLS can contract in response to methacholine, the secretion of LPS-induced TNF-α, while maintained, may diminish over time.[13] Furthermore, long-term cultivation can result in the loss of certain cell populations, such as pneumocytes and lymphocytes, as well as the degradation of connective tissue fibers. These changes may contribute to decreased sensitivity of cultured PCLS to external stimuli.[13]
In practice, PCLS can maintain comparable viability and tissue homeostasis for 1 to 3 days, though extended periods can be achieved with optimized culture conditions.[14]
Experimental applications
Precision-cut lung slices find extensive use in a variety of experimental applications in the field of respiratory research. Some of the key areas where PCLS are employed include:
Asthma
In the pursuit of understanding and developing treatments for asthma, researchers have explored various models, including animal models like mice and rats, to mimic different aspects of the condition. While these animal models have contributed to our knowledge, they come with limitations, particularly in terms of translatability to humans.[15]
To address these limitations and enhance our understanding of asthma, researchers have turned to human Precision-cut Lung Slices (PCLS) obtained from both healthy and diseased individuals as a valuable ex vivo tool.[16] PCLS derived from healthy and asthmatic lungs exhibit altered responses to various stimuli, including bronchoconstriction and hyperresponsiveness, which closely resemble those observed in patients and various animal models.[16]
Moreover, PCLS from individuals with asthma have been shown to display significantly increased airway inflammation and hyperresponsiveness when stimulated by factors such as rhinovirus.[17] These PCLS also exhibit elevated gene expression related to asthma pathogenesis, including genes like Il25, Tslp, and Il13.[18] These findings align with observations in asthmatic patients, indicating that PCLS models provide a promising platform for asthma research.[16]
COPD (Chronic Obstructive Pulmonary Disease)
While no in vivo models fully encompass all aspects of clinical COPD pathology, certain animal models, such as those involving cigarette smoke exposure, elastase-induced emphysema, and LPS challenge, have yielded valuable insights. For instance, exposing guinea pigs or mice to cigarette smoke can reproduce key features of human COPD, including emphysema, small airway remodeling, and pulmonary hypertension. However, this model typically manifests mild emphysema and requires months to develop.[19] In contrast, delivering elastase to the lungs of mice rapidly induces an emphysematous phenotype, allowing for controlled disease severity by adjusting elastase dose, administration route, and duration.[20] It's worth noting that the physiological relevance of elastase and LPS models is debatable due to differences in underlying mechanisms.[21]
The use of Precision-cut Lung Slices (PCLS) from in vivo models has proven particularly valuable in modeling COPD. For instance, PCLS obtained from smoke-exposed mice have shown elevated expression of chemokines when stimulated with viral mimics or influenza A virus.[22] Murine PCLS have also demonstrated that Influenza A infection and cigarette smoke can impair bronchodilator responsiveness to β2-adrenoceptor agonists. Future studies employing PCLS from COPD patients hold the potential to enable both functional and phenotypic immune cell characterization, facilitating a more comprehensive understanding of molecular mechanisms underlying disease heterogeneity.
Idiopathic Pulmonary Fibrosis (IPF)
Precision-cut Lung Slices (PCLS) have proven effective in studying the early stages of lung fibrosis in IPF. When exposed to TGF-β1 and cadmium chloride, both human and rat PCLS have displayed relevant pathohistological changes commonly observed in the early phases of lung fibrosis. These changes include the upregulation of critical pro-fibrotic genes, increased thickness of alveolar septa, and abnormal activation of pulmonary cells.[23]
Recent advancements in research have led to the establishment of an ex vivo human PCLS model specifically focused on early-stage fibrosis. This model involves exposing PCLS to a combination of pro-fibrotic growth factors and signaling molecules, including TGF-β1, TNF-α, platelet-derived growth factor-AB, and lysophosphatidic acid.[24] This approach offers a pathway to investigate the underlying mechanisms of early IPF and assess novel therapies.[25]
Researchers are actively evaluating novel treatments for IPF using PCLS. For example, caffeine, which inhibits TGF-β-induced increases in pro-fibrotic gene expression, has shown promise by significantly reducing fibrosis in PCLS from bleomycin-treated mice. Additionally, targeting PI3K signaling has emerged as a promising anti-fibrotic treatment strategy, as demonstrated using PCLS derived from IPF patients.[26]
The use of PCLS in IPF research holds great potential for understanding the disease's early stages, testing innovative therapies, and uncovering novel treatment strategies.
Infection and Inflammation
Precision-cut Lung Slices (PCLS) have been instrumental in studying the body's innate responses to viral and, to a lesser extent, bacterial challenges. This system has shed light on which cells become infected within the intact lung, offering insights distinct from in vitro air-liquid interface cultures.[27]
Studies by Goris et al. have revealed variations in the infectability of different cell types within the lung. For instance, bovine parainfluenza virus infection was observed primarily in cells beneath the lung epithelium within the PCLS system.[28][29] Importantly, this suggests that the epithelium, when in its natural physiological structure, resists infection. Similar findings were reported by Kirchhoff et al.[30] These studies emphasize the significance of studying cells within their physiological environment, considering cell associations and structural architecture. Such interactions not only affect infectability but also shape the system's response to infection.
The PCLS system serves as a valuable tool for understanding inflammatory responses. It has been employed to investigate the innate response to bacterial wall components like LPS and to conduct complex mixed infection studies involving multiple viruses or viral and bacterial co-infections. This approach enables precise analysis of immune responses to each stimulus. In simpler models, PCLS have been used to assess the impact of LPS on the innate immune response, testing the effects of various immunomodulators on innate signaling.[31][32]
Furthermore, the ability to obtain slices from diseased lungs, such as those affected by conditions like COPD and asthma, provides a robust model for studying how respiratory diseases influence infectivity and host responses. This is particularly relevant for diseases like COPD and asthma, which have links to pathogen-induced exacerbations.
PCLS research in infection and inflammation enhances our understanding of immune responses, paving the way for insights into disease mechanisms and potential therapeutic strategies.
Drug Testing
Precision-cut Lung Slices (PCLS) play a crucial role in evaluating novel therapeutic targets for asthma, especially as tolerance to conventional treatments like glucocorticoids and β2-receptor agonists becomes more common. Researchers have increasingly focused on targets relevant to asthma pathogenesis, and PCLS have become a valuable tool for evaluating these targets as potential therapeutics.[33]
For instance, studies have shown that inhibiting histone deacetylase with trichostatin A can alleviate airway constriction in human PCLS and simultaneously reduce airway hyperresponsiveness in antigen-challenged mice.[34] Additionally, activating soluble guanylate cyclase in airway smooth muscle using riociguat and cinaciguat analogs has been found to induce bronchodilation in normal human PCLS and reverse airway hyperresponsiveness in allergic asthmatic mice, restoring normal lung function.[33][35]
The use of PCLS in drug development is expanding further, with specific agonists or inhibitors targeting bitter-taste receptors, peroxisome proliferator-activated receptor (PPAR) γ, phosphoinositide-3 kinase (PI3K), BK channels, and spleen tyrosine kinase (Syk) all undergoing investigation within this context.[33][36]
PCLS research contributes significantly to the development of innovative therapeutic strategies for asthma, addressing the evolving challenges of treatment resistance.[33]
Advantages of PCLS
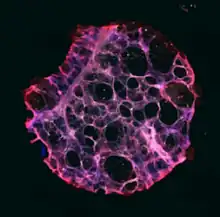
Precision-cut Lung Slices (PCLS) offer several distinct advantages that make them invaluable tools in respiratory research. They excel in preserving the intricate lung architecture, maintaining essential tissue structures like small airways, respiratory parenchyma, structural and immune cell populations, and connective tissue.[37] The cellular composition within PCLS closely mirrors that of intact lungs, retaining the organization of structural and immune cells.[38][39] However, it's important to note that specific cell types' distribution may vary among slices due to regional variability within the lung, especially in the presence of non-uniform disease-related changes.[40]
In certain contexts, PCLS can be considered as "mini" lungs.[41] While lacking a recruitable immune system, PCLS provide a unique opportunity to correlate cell-specific functions with organ physiology. They exhibit complex responses to challenges and stimuli, such as airway contraction and immune responses, shedding light on disease mechanisms and treatment evaluations.[42]
PCLS have found applications in a wide range of respiratory research areas, including asthma, COPD, idiopathic pulmonary fibrosis, allergies, infections, and toxicology studies. Researchers have harnessed the advantages of PCLS to model and study these prominent respiratory diseases, facilitating insights and translational relevance to human disease.[40]
Limitations of PCLS
Precision-cut Lung Slices (PCLS) provide valuable insights into lung physiology and pathology, but they do have limitations. Firstly, PCLS represent a static "snapshot" of lung tissue at the time of excision, lacking access to the dynamic, recruitable immune system present in living organisms. This limitation hinders the full understanding of immune responses within the lung.[43]
Furthermore, lung tissue is inherently heterogeneous, with variations in epithelial integrity, immune cell populations, and responses to stimulation across different lung regions. When studying diseases, such as respiratory conditions, this heterogeneity can complicate data interpretation, requiring careful statistical analysis to account for variability between slices.[44][45]
PCLS have a limited ability to fully replicate the intricate and dynamic immune responses observed in living organisms. They cannot recruit non-resident immune cells, and their viability is restricted to approximately two weeks.[46] While they can capture initial signals induced by pathogens, they cannot fully mimic the complex immune responses seen in a living lung.[47]
Another limitation is that PCLS are typically used as static systems and do not replicate the natural breathing motion of the lung.[48] This is particularly relevant when studying diseases like ventilator-induced lung injury, where mechanical stress from ventilation plays a crucial role. Attempts to stretch or deform PCLS have been made to simulate mechanical dynamics, but accurately replicating these processes remains a challenge.[49][50][51]
Administering treatments in PCLS can be challenging because the entire slice is bathed in the compound or stimulant of interest. This poses difficulties in translating findings to inhaled or systemic applications in vivo, making dosing and translation [52]
Administering treatments in PCLS can be challenging because the entire slice is bathed in the compound or stimulant of interest. This poses difficulties in translating findings to inhaled or systemic applications in vivo, making dosing and translation complex.[53][54]
See also
- Precision cut tissue slices
- Vibratome
References
- Morin, Jean-Paul; Baste, Jean-Marc; Gay, Arnaud; Crochemore, Clément; Corbière, Cécile; Monteil, Christelle (2013). "Precision cut lung slices as an efficient tool for in vitro lung physio-pharmacotoxicology studies". Xenobiotica. 43 (1): 63–72. doi:10.3109/00498254.2012.727043. PMID 23030793. S2CID 207427454.
- Liu, Yan; Wu, Ping; Wang, Yin; Liu, Yansong; Yang, Hongfang; Zhou, Guohua; Wu, Xiaoqi; Wen, Qingping (2022). "Application of Precision-Cut Lung Slices as an in Vitro Model for Research of Inflammatory Respiratory Diseases". Bioengineering. 9 (12): 767. doi:10.3390/bioengineering9120767. PMC 9774555. PMID 36550973.
- Sewald, K.; Braun, A. (2013). "Assessment of immunotoxicity using precision-cut tissue slices". Xenobiotica; the Fate of Foreign Compounds in Biological Systems. 43 (1): 84–97. doi:10.3109/00498254.2012.731543. PMC 3518294. PMID 23199366.
- Abdelaal, H. M.; Kim, H. O.; Wagstaff R; Sawahata, R.; Southern, P. J.; Skinner, P. J. (2015). "Comparison of Vibratome and Compresstome sectioning of fresh primate lymphoid and genital tissues for in situ MHC-tetramer and immunofluorescence staining". Biological Procedures Online. 17 (1): 2. doi:10.1186/s12575-014-0012-4. PMC 4318225. PMID 25657614.
- Lam, Maggie; Lamanna, Emma; Organ, Louise; Donovan, Chantal; Bourke, Jane E. (2023). "Perspectives on precision cut lung slices—powerful tools for investigation of mechanisms and therapeutic targets in lung diseases". Frontiers in Pharmacology. 14. doi:10.3389/fphar.2023.1162889. PMC 10228656. PMID 37261291.
- Alsafadi, Hani N.; Uhl, Franziska E.; Pineda, Ricardo H.; Bailey, Kolene E.; Rojas, Mauricio; Wagner, Darcy E.; Königshoff, Melanie (2020). "Applications and Approaches for Three-Dimensional Precision-Cut Lung Slices. Disease Modeling and Drug Discovery". American Journal of Respiratory Cell and Molecular Biology. 62 (6): 681–691. doi:10.1165/rcmb.2019-0276TR. PMC 7401444. PMID 31991090.
- Alsafadi, Hani N.; Uhl, Franziska E.; Pineda, Ricardo H.; Bailey, Kolene E.; Rojas, Mauricio; Wagner, Darcy E.; Königshoff, Melanie (2020). "Applications and Approaches for Three-Dimensional Precision-Cut Lung Slices. Disease Modeling and Drug Discovery". American Journal of Respiratory Cell and Molecular Biology. 62 (6): 681–691. doi:10.1165/rcmb.2019-0276TR. PMC 7401444. PMID 31991090.
- Akram, Khondoker M.; Yates, Laura L.; Mongey, Róisín; Rothery, Stephen; Gaboriau, David C. A.; Sanderson, Jeremy; Hind, Matthew; Griffiths, Mark; Dean, Charlotte H. (2019). "Live imaging of alveologenesis in precision-cut lung slices reveals dynamic epithelial cell behaviour". Nature Communications. 10 (1): 1178. Bibcode:2019NatCo..10.1178A. doi:10.1038/s41467-019-09067-3. PMC 6414680. PMID 30862802.
- Michalaki, Christina; Dean, Charlotte; Johansson, Cecilia (2022). "The Use of Precision‐Cut Lung Slices for Studying Innate Immunity to Viral Infections". Current Protocols. 2 (8): e505. doi:10.1002/cpz1.505. hdl:10044/1/99043. PMC 9545600. PMID 35938685.
- Dimou, Paraskevi; Trivedi, Sumita; Liousia, Maria; d'Souza, Reena R.; Klampatsa, Astero (2022). "Precision-Cut Tumor Slices (PCTS) as an Ex Vivo Model in Immunotherapy Research". Antibodies. 11 (2): 26. doi:10.3390/antib11020026. PMC 9036232. PMID 35466279.
- Temann, A.; Golovina, T.; Neuhaus, V.; Thompson, C.; Chichester, J. A.; Braun, A.; Yusibov, V. (2017). "Evaluation of inflammatory and immune responses in long-term cultured human precision-cut lung slices". Human Vaccines & Immunotherapeutics. 13 (2): 351–358. doi:10.1080/21645515.2017.1264794. PMC 5328235. PMID 27929748.
- Preuß, Eike B.; Schubert, Stephanie; Werlein, Christopher; Stark, Helge; Braubach, Peter; Höfer, Anne; Plucinski, Edith K.J.; Shah, Harshit R.; Geffers, Robert; Sewald, Katherina; Braun, Armin; Jonigk, Danny D.; Kühnel, Mark P. (2022). "The Challenge of Long-Term Cultivation of Human Precision-Cut Lung Slices". The American Journal of Pathology. 192 (2): 239–253. doi:10.1016/j.ajpath.2021.10.020. PMC 8891143. PMID 34767811.
- Neuhaus, V.; Schaudien, D.; Golovina, T.; Temann, U. A.; Thompson, C.; Lippmann, T.; Bersch, C.; Pfennig, O.; Jonigk, D.; Braubach, P.; Fieguth, H. G.; Warnecke, G.; Yusibov, V.; Sewald, K.; Braun, A. (2017). "Assessment of long-term cultivated human precision-cut lung slices as an ex vivo system for evaluation of chronic cytotoxicity and functionality". Journal of Occupational Medicine and Toxicology (London, England). 12: 13. doi:10.1186/s12995-017-0158-5. PMC 5446749. PMID 28559920.
- Sanderson, M. J. (2011). "Exploring lung physiology in health and disease with lung slices". Pulmonary Pharmacology & Therapeutics. 24 (5): 452–465. doi:10.1016/j.pupt.2011.05.001. PMC 3168687. PMID 21600999.
- Mullane, K.; Williams, M. (2014). "Animal models of asthma: Reprise or reboot?". Biochemical Pharmacology. 87 (1): 131–139. doi:10.1016/j.bcp.2013.06.026. PMID 23831953.
- Wohlsen, A.; Martin, C.; Vollmer, E.; Branscheid, D.; Magnussen, H.; Becker, W. M.; Lepp, U.; Uhlig, S. (2003). "The early allergic response in small airways of human precision-cut lung slices". The European Respiratory Journal. 21 (6): 1024–1032. doi:10.1183/09031936.03.00027502. PMID 12797499. S2CID 19972045.
- Kennedy, J. L.; Koziol-White, C. J.; Jeffus, S.; Rettiganti, M. R.; Fisher, P.; Kurten, M.; Eze, A.; House, S.; Sikes, J. D.; Askew, E.; Putt, C.; Panettieri, R. A.; Jones, S. M.; Kurten, R. C. (2018). "Effects of rhinovirus 39 infection on airway hyperresponsiveness to carbachol in human airways precision cut lung slices". The Journal of Allergy and Clinical Immunology. 141 (5): 1887–1890.e1. doi:10.1016/j.jaci.2017.11.041. PMC 5938135. PMID 29317243.
- Ying, S.; O'Connor, B.; Ratoff, J.; Meng, Q.; Fang, C.; Cousins, D.; Zhang, G.; Gu, S.; Gao, Z.; Shamji, B.; Edwards, M. J.; Lee, T. H.; Corrigan, C. J. (2008). "Expression and cellular provenance of thymic stromal lymphopoietin and chemokines in patients with severe asthma and chronic obstructive pulmonary disease". Journal of Immunology (Baltimore, Md. : 1950). 181 (4): 2790–2798. doi:10.4049/jimmunol.181.4.2790. PMID 18684970. S2CID 86013485.
- Wright, J. L.; Cosio, M.; Churg, A. (2008). "Animal models of chronic obstructive pulmonary disease". American Journal of Physiology. Lung Cellular and Molecular Physiology. 295 (1): L1-15. doi:10.1152/ajplung.90200.2008. PMC 2494776. PMID 18456796.
- Antunes, M. A.; Rocco, P. R. (2011). "Elastase-induced pulmonary emphysema: Insights from experimental models". Anais da Academia Brasileira de Ciencias. 83 (4): 1385–1396. doi:10.1590/s0001-37652011005000039. PMID 22159348.
- Liu, G.; Särén, L.; Douglasson, H.; Zhou, X. H.; Åberg, P. M.; Ollerstam, A.; Betts, C. J.; Balogh Sivars, K. (2021). "Precision cut lung slices: An ex vivo model for assessing the impact of immunomodulatory therapeutics on lung immune responses". Archives of Toxicology. 95 (8): 2871–2877. doi:10.1007/s00204-021-03096-y. PMID 34191076. S2CID 235687459.
- Agraval, H.; Crue, T.; Schaunaman, N.; Numata, M.; Day, B. J.; Chu, H. W. (2023). "Electronic Cigarette Exposure Increases the Severity of Influenza a Virus Infection via TRAIL Dysregulation in Human Precision-Cut Lung Slices". International Journal of Molecular Sciences. 24 (5): 4295. doi:10.3390/ijms24054295. PMC 10002047. PMID 36901724.
- Westra, I. M.; Pham, B. T.; Groothuis, G. M.; Olinga, P. (2013). "Evaluation of fibrosis in precision-cut tissue slices". Xenobiotica; the Fate of Foreign Compounds in Biological Systems. 43 (1): 98–112. doi:10.3109/00498254.2012.723151. PMID 23002908. S2CID 11829880.
- Alsafadi, H. N.; Staab-Weijnitz, C. A.; Lehmann, M.; Lindner, M.; Peschel, B.; Königshoff, M.; Wagner, D. E. (2017). "An ex vivo model to induce early fibrosis-like changes in human precision-cut lung slices". American Journal of Physiology. Lung Cellular and Molecular Physiology. 312 (6): L896–L902. doi:10.1152/ajplung.00084.2017. PMID 28314802. S2CID 2255748.
- Cedilak, M.; Banjanac, M.; Belamarić, D.; Paravić Radičević, A.; Faraho, I.; Ilić, K.; Čužić, S.; Glojnarić, I.; Eraković Haber, V.; Bosnar, M. (2019). "Precision-cut lung slices from bleomycin treated animals as a model for testing potential therapies for idiopathic pulmonary fibrosis". Pulmonary Pharmacology & Therapeutics. 55: 75–83. doi:10.1016/j.pupt.2019.02.005. PMID 30776489. S2CID 73462721.
- Cedilak, M.; Banjanac, M.; Belamarić, D.; Paravić Radičević, A.; Faraho, I.; Ilić, K.; Čužić, S.; Glojnarić, I.; Eraković Haber, V.; Bosnar, M. (2019). "Precision-cut lung slices from bleomycin treated animals as a model for testing potential therapies for idiopathic pulmonary fibrosis". Pulmonary Pharmacology & Therapeutics. 55: 75–83. doi:10.1016/j.pupt.2019.02.005. PMID 30776489. S2CID 73462721.
- Liu, G.; Betts, C.; Cunoosamy, D. M.; Åberg, P. M.; Hornberg, J. J.; Sivars, K. B.; Cohen, T. S. (2019). "Use of precision cut lung slices as a translational model for the study of lung biology". Respiratory Research. 20 (1): 162. doi:10.1186/s12931-019-1131-x. PMC 6642541. PMID 31324219.
- Goris, K.; Uhlenbruck, S.; Schwegmann-Wessels, C.; Köhl, W.; Niedorf, F.; Stern, M.; Hewicker-Trautwein, M.; Bals, R.; Taylor, G.; Braun, A.; Bicker, G.; Kietzmann, M.; Herrler, G. (2009). "Differential sensitivity of differentiated epithelial cells to respiratory viruses reveals different viral strategies of host infection". Journal of Virology. 83 (4): 1962–1968. doi:10.1128/JVI.01271-08. PMC 2643795. PMID 19052091.
- Kirchhoff, J.; Uhlenbruck, S.; Goris, K.; Keil, G. M.; Herrler, G. (2014). "Three viruses of the bovine respiratory disease complex apply different strategies to initiate infection". Veterinary Research. 45 (1): 20. doi:10.1186/1297-9716-45-20. PMC 3942114. PMID 24548739.
- Kirchhoff, J.; Uhlenbruck, S.; Keil, G. M.; Schwegmann-Wessels, C.; Ganter, M.; Herrler, G. (2014). "Infection of differentiated airway epithelial cells from caprine lungs by viruses of the bovine respiratory disease complex". Veterinary Microbiology. 170 (1–2): 58–64. doi:10.1016/j.vetmic.2014.01.038. PMID 24612951.
- Seehase, S.; Lauenstein, H. D.; Schlumbohm, C.; Switalla, S.; Neuhaus, V.; Förster, C.; Fieguth, H. G.; Pfennig, O.; Fuchs, E.; Kaup, F. J.; Bleyer, M.; Hohlfeld, J. M.; Braun, A.; Sewald, K.; Knauf, S. (2012). "LPS-induced lung inflammation in marmoset monkeys - an acute model for anti-inflammatory drug testing". PLOS ONE. 7 (8): e43709. Bibcode:2012PLoSO...743709S. doi:10.1371/journal.pone.0043709. PMC 3429492. PMID 22952743.
- Alsafadi, H. N.; Staab-Weijnitz, C. A.; Lehmann, M.; Lindner, M.; Peschel, B.; Königshoff, M.; Wagner, D. E. (2017). "An ex vivo model to induce early fibrosis-like changes in human precision-cut lung slices". American Journal of Physiology. Lung Cellular and Molecular Physiology. 312 (6): L896–L902. doi:10.1152/ajplung.00084.2017. PMID 28314802. S2CID 2255748.
- https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(23)00392-4/fulltext
- Banerjee, A.; Trivedi, C. M.; Damera, G.; Jiang, M.; Jester, W.; Hoshi, T.; Epstein, J. A.; Panettieri Jr, R. A. (2012). "Trichostatin a abrogates airway constriction, but not inflammation, in murine and human asthma models". American Journal of Respiratory Cell and Molecular Biology. 46 (2): 132–138. doi:10.1165/rcmb.2010-0276OC. PMC 3297166. PMID 22298527.
- Ghosh, A.; Koziol-White, C. J.; Asosingh, K.; Cheng, G.; Ruple, L.; Groneberg, D.; Friebe, A.; Comhair, S. A.; Stasch, J. P.; Panettieri Jr, R. A.; Aronica, M. A.; Erzurum, S. C.; Stuehr, D. J. (2016). "Soluble guanylate cyclase as an alternative target for bronchodilator therapy in asthma". Proceedings of the National Academy of Sciences of the United States of America. 113 (17): E2355-62. Bibcode:2016PNAS..113E2355G. doi:10.1073/pnas.1524398113. PMC 4855555. PMID 27071111.
- Bai, Y.; Krishnamoorthy, N.; Patel, K. R.; Rosas, I.; Sanderson, M. J.; Ai, X. (2016). "Cryopreserved Human Precision-Cut Lung Slices as a Bioassay for Live Tissue Banking. A Viability Study of Bronchodilation with Bitter-Taste Receptor Agonists". American Journal of Respiratory Cell and Molecular Biology. 54 (5): 656–663. doi:10.1165/rcmb.2015-0290MA. PMC 4942196. PMID 26550921.
- Alsafadi, H. N.; Uhl, F. E.; Pineda, R. H.; Bailey, K. E.; Rojas, M.; Wagner, D. E.; Königshoff, M. (2020). "Applications and Approaches for Three-Dimensional Precision-Cut Lung Slices. Disease Modeling and Drug Discovery". American Journal of Respiratory Cell and Molecular Biology. 62 (6): 681–691. doi:10.1165/rcmb.2019-0276TR. PMC 7401444. PMID 31991090.
- Lyons-Cohen, M. R.; Thomas, S. Y.; Cook, D. N.; Nakano, H. (2017). "Precision-cut Mouse Lung Slices to Visualize Live Pulmonary Dendritic Cells". Journal of Visualized Experiments : Jove (122). doi:10.3791/55465. PMC 5512285. PMID 28448013.
- Kretschmer, S.; Dethlefsen, I.; Hagner-Benes, S.; Marsh, L. M.; Garn, H.; König, P. (2013). "Visualization of intrapulmonary lymph vessels in healthy and inflamed murine lung using CD90/Thy-1 as a marker". PLOS ONE. 8 (2): e55201. Bibcode:2013PLoSO...855201K. doi:10.1371/journal.pone.0055201. PMC 3568125. PMID 23408960.
- Viana, F.; O'Kane, C. M.; Schroeder, G. N. (2021). "Precision‐cut lung slices: A powerful ex vivo model to investigate respiratory infectious diseases". Molecular Microbiology. 117 (3): 578–588. doi:10.1111/mmi.14817. PMC 9298270. PMID 34570407.
- "Precision-Cut Lung Slices (PCLS)".
- Temann, A.; Golovina, T.; Neuhaus, V.; Thompson, C.; Chichester, J. A.; Braun, A.; Yusibov, V. (2017). "Evaluation of inflammatory and immune responses in long-term cultured human precision-cut lung slices". Human Vaccines & Immunotherapeutics. 13 (2): 351–358. doi:10.1080/21645515.2017.1264794. PMC 5328235. PMID 27929748.
- Davidovich, N.; Huang, J.; Margulies, S. S. (2013). "Reproducible uniform equibiaxial stretch of precision-cut lung slices". American Journal of Physiology. Lung Cellular and Molecular Physiology. 304 (4): L210-20. doi:10.1152/ajplung.00224.2012. PMC 3567360. PMID 23275624.
- Dudek, M.; Puttur, F.; Arnold-Schrauf, C.; Kühl, A. A.; Holzmann, B.; Henriques-Normark, B.; Berod, L.; Sparwasser, T. (2016). "Lung epithelium and myeloid cells cooperate to clear acute pneumococcal infection". Mucosal Immunology. 9 (5): 1288–1502. doi:10.1038/mi.2015.128. PMC 4990776. PMID 26627460.
- Martin, C.; Uhlig, S.; Ullrich, V. (1996). "Videomicroscopy of methacholine-induced contraction of individual airways in precision-cut lung slices". The European Respiratory Journal. 9 (12): 2479–2487. doi:10.1183/09031936.96.09122479. PMID 8980957.
- Craig, A.; Mai, J.; Cai, S.; Jeyaseelan, S. (2009). "Neutrophil recruitment to the lungs during bacterial pneumonia". Infection and Immunity. 77 (2): 568–575. doi:10.1128/IAI.00832-08. PMC 2632043. PMID 19015252.
- Alsafadi, Hani N.; Staab-Weijnitz, Claudia A.; Lehmann, Mareike; Lindner, Michael; Peschel, Britta; Königshoff, Melanie; Wagner, Darcy E. (2017). "An ex vivo model to induce early fibrosis-like changes in human precision-cut lung slices". American Journal of Physiology-Lung Cellular and Molecular Physiology. 312 (6): L896–L902. doi:10.1152/ajplung.00084.2017. PMID 28314802. S2CID 2255748.
- Bates JHT; Smith, B. J. (2018). "Ventilator-induced lung injury and lung mechanics". Annals of Translational Medicine. 6 (19): 378. doi:10.21037/atm.2018.06.29. PMC 6212358. PMID 30460252.
- Dassow, C.; Wiechert, L.; Martin, C.; Schumann, S.; Müller-Newen, G.; Pack, O.; Guttmann, J.; Wall, W. A.; Uhlig, S. (2010). "Biaxial distension of precision-cut lung slices". Journal of Applied Physiology (Bethesda, Md. : 1985). 108 (3): 713–721. doi:10.1152/japplphysiol.00229.2009. PMID 20075265.
- Dassow, C.; Wiechert, L.; Martin, C.; Schumann, S.; Müller-Newen, G.; Pack, O.; Guttmann, J.; Wall, W. A.; Uhlig, S. (2010). "Biaxial distension of precision-cut lung slices". Journal of Applied Physiology. 108 (3): 713–721. doi:10.1152/japplphysiol.00229.2009. PMID 20075265.
- Ewart, L.; Dehne, E. M.; Fabre, K.; Gibbs, S.; Hickman, J.; Hornberg, E.; Ingelman-Sundberg, M.; Jang, K. J.; Jones, D. R.; Lauschke, V. M.; Marx, U.; Mettetal, J. T.; Pointon, A.; Williams, D.; Zimmermann, W. H.; Newham, P. (2018). "Application of Microphysiological Systems to Enhance Safety Assessment in Drug Discovery". Annual Review of Pharmacology and Toxicology. 58: 65–82. doi:10.1146/annurev-pharmtox-010617-052722. PMID 29029591.
- complex.https://erj.ersjournals.com/content/9/12/2479.short
- Ewart, L.; Dehne, E. M.; Fabre, K.; Gibbs, S.; Hickman, J.; Hornberg, E.; Ingelman-Sundberg, M.; Jang, K. J.; Jones, D. R.; Lauschke, V. M.; Marx, U.; Mettetal, J. T.; Pointon, A.; Williams, D.; Zimmermann, W. H.; Newham, P. (2018). "Application of Microphysiological Systems to Enhance Safety Assessment in Drug Discovery". Annual Review of Pharmacology and Toxicology. 58: 65–82. doi:10.1146/annurev-pharmtox-010617-052722. PMID 29029591.
- Stucki, J. D.; Hobi, N.; Galimov, A.; Stucki, A. O.; Schneider-Daum, N.; Lehr, C. M.; Huwer, H.; Frick, M.; Funke-Chambour, M.; Geiser, T.; Guenat, O. T. (2018). "Medium throughput breathing human primary cell alveolus-on-chip model". Scientific Reports. 8 (1): 14359. Bibcode:2018NatSR...814359S. doi:10.1038/s41598-018-32523-x. PMC 6156575. PMID 30254327.