Emotional detachment
In psychology, emotional detachment, also known as emotional blunting, is a condition or state in which a person lacks emotional connectivity to others, whether due to an unwanted circumstance or as a positive means to cope with anxiety. Such a coping strategy, also known as emotion focused-coping, is used when avoiding certain situations that might trigger anxiety.[3] It refers to the evasion of emotional connections. Emotional detachment may be a temporary reaction to a stressful situation, or a chronic condition such as depersonalization-derealization disorder. It may also be caused by certain antidepressants. Emotional blunting, also known as reduced affect display, is one of the negative symptoms of schizophrenia.
| Part of a series on |
| Emotions |
|---|
  |
Signs and symptoms
Emotional detachment may not be as outwardly obvious as other psychiatric symptoms. Patients diagnosed with emotional detachment have reduced ability to express emotion, to empathize with others or to form powerful emotional connections. Patients are also at an increased risk for many anxiety and stress disorders. This can lead to difficulties in creating and maintaining personal relationships. The person may move elsewhere in their mind and appear preoccupied or "not entirely present", or they may seem fully present but exhibit purely intellectual behavior when emotional behavior would be appropriate. They may have a hard time being a loving family member, or they may avoid activities, places, and people associated with past traumas. Their dissociation can lead to lack of attention and, hence, to memory problems and in extreme cases, amnesia. In some cases, they present an extreme difficulty in giving or receiving empathy which can be related to the spectrum of narcissistic personality disorder.[4] Additionally, emotional blunting is negatively correlated with remission quality. The negative symptoms are far less likely to disappear when a patient is experiencing emotional blunting.[5]
In a study of children ages 4–12, traits of aggression and antisocial behaviors were found to be correlated with emotional detachment. Researchers determined that these could be early signs of emotional detachment, suggesting parents and clinicians to evaluate children with these traits for a higher behavioral problem in order to avoid bigger problems (such as emotional detachment) in the future.[6]
A correlation was found of higher emotional blunting among patients treated with depression who scored higher on the Hospital Anxiety and Depression Scale (HADS) and were male (though the frequency difference was slight).[5]
Emotional detachment in small amounts is normal. For example, being able to emotionally and psychologically detach from work when one is not in the workplace is a normal behavior. Emotional detachment becomes an issue when it impairs a person's ability to function on a day-to-day level.[7]
Scales
While some depression severity scales provide insight to emotional blunting levels, many symptoms are not adequately covered.[8] An attempt to resolve this issue is the Oxford Depression Questionnaire (ODQ), a scale specifically designed for full assessment of emotional blunting symptoms. The ODQ is designed specifically for patients with Major Depressive Disorder (MDD) in order to assess individual levels of emotional blunting.
Another scale, known as the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants (OQESA), was developed using qualitative methods.[5]
Causes
Emotional detachment and/or emotional blunting have multiple causes, as the cause can vary from person to person. Emotional detachment or emotional blunting often arises due to adverse childhood experiences, for example physical, sexual or emotional abuse. Emotional detachment is a maladaptive coping mechanism for trauma, especially in young children who have not developed coping mechanisms. Emotional detachments can also be due to psychological trauma in adulthood, like abuse, or traumatic experiences like war, automobile accidents etc.[9][10]
Emotional blunting is often caused by antidepressants, in particular selective serotonin reuptake inhibitors (SSRIs) used in MDD and often as an add-on treatment in other psychiatric disorders.[11][12] Individuals with MDD usually experience emotional blunting as well.[8] Emotional blunting is a symptom of MDD,[5] as depression is negatively correlated with emotional (both positive and negative) experiences.[13]
Schizophrenia often occurs with negative symptoms, extrapyramidal signs (EPS), and depression. The latter overlaps with emotional blunting and is shown to be a core part of the present effects.[14] Schizophrenia in general causes abnormalities in emotional understanding of individuals, all of which are clinically considered as an emotional blunting symptom. Individuals with schizophrenia show less emotional experiences, display less emotional expressions, and fail to recognize the emotional experiences and/or expressions of other individuals.[15]
The changes in fronto-limbic activity in conjunction with depression succeeding a left hemisphere basal ganglia stroke (LBG stroke) may contribute to emotional blunting. LBG strokes are associated with depression and often caused by disorders of the basal ganglia (BG). Such disorders alter the emotional perception and experiences of the patient.[13]
In many cases people with eating disorders (ED) show signs of emotional detachment. This is due to the fact that many of the circumstances that often lead to an ED are the same as the circumstances that lead to emotional detachment. For example, people with ED often have experienced childhood abuse. Eating disorders on their own are a maladaptive coping mechanism and to cope with the effects of an eating disorder, people may turn to emotional detachment.[16]
Bereavement or losing a loved one can also be causes of emotional detachment.[16]
Unfortunately, the prevalence of emotional blunting is not fully known.[5]
Behavioral mechanism
Emotional detachment is a maladaptive coping mechanism, which allows a person to react calmly to highly emotional circumstances. Emotional detachment in this sense is a decision to avoid engaging emotional connections, rather than an inability or difficulty in doing so, typically for personal, social, or other reasons. In this sense it can allow people to maintain boundaries, and avoid undesired impact by or upon others, related to emotional demands. As such it is a deliberate mental attitude which avoids engaging the emotions of others.
This detachment does not necessarily mean avoiding empathy; rather, it allows the person to rationally choose whether or not to be overwhelmed or manipulated by such feelings. Examples where this is used in a positive sense might include emotional boundary management, where a person avoids emotional levels of engagement related to people who are in some way emotionally overly demanding, such as difficult co-workers or relatives, or is adopted to aid the person in helping others.
Emotional detachment can also be "emotional numbing",[17] "emotional blunting", i.e., dissociation, depersonalization or in its chronic form depersonalization disorder.[18] This type of emotional numbing or blunting is a disconnection from emotion, it is frequently used as a coping survival skill during traumatic childhood events such as abuse or severe neglect. After continually using this coping mechanism, it can become a response to daily stresses.[19]
Emotional detachment may allow acts of extreme cruelty and abuse, supported by the decision to not connect empathically with the person concerned. Social ostracism, such as shunning and parental alienation, are other examples where decisions to shut out a person creates a psychological trauma for the shunned party.[20]
See also
- Alexithymia
- Anhedonia § Social anhedonia
- Asociality
- Assertiveness
- Borderline Personality Disorder
- Dissociation
- Dissociative disorders (in DSM-IV)
- Emotional contagion
- Emotional dysregulation
- Emotional isolation
- Psychic distance
- Reactive attachment disorder
- Social rejection
- Splitting (psychology)
- Stoicism
- Structured Clinical Interview for DSM-IV
References
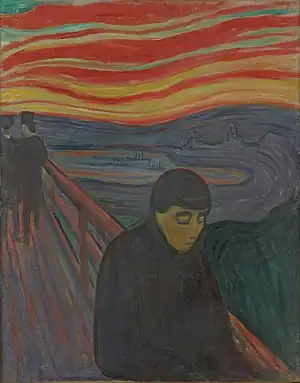
- Aarkrog T (1990). Edvard Munch: The Life of a Person with Borderline Personality as Seen Through His Art [Edvard Munch, et livsløb af en grænsepersonlighed forstået gennem hans billeder]. Danmark: Lundbeck Pharma A/S. ISBN 978-8798352419.
- Wylie HW (1980). "Edvard Munch". The American Imago; A Psychoanalytic Journal for the Arts and Sciences. Johns Hopkins University Press. 37 (4): 413–443. JSTOR 26303797. PMID 7008567.
- "Emotion-focused coping". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d.
- Johnson, Stephen M (1987), Humanizing the Narcissistic Style, NY: Norton and Co., p. 125, ISBN 0-393-70037-2
- Goodwin, G.M.; Price, J.; De Bodinat, C.; Laredo, J. (2017). "Emotional blunting with antidepressant treatments: A survey among depressed patients". Journal of Affective Disorders. Elsevier BV. 221: 31–35. doi:10.1016/j.jad.2017.05.048. ISSN 0165-0327. PMID 28628765. S2CID 3755520. Retrieved 2021-11-20.
- Manti, Eirini; Scholte, Evert M.; Van Berckelaer-Onnes, Ina A.; Van Der Ploeg, Jan D. (2009). "Social and emotional detachment: A cross-cultural comparison of the non-disruptive behavioural psychopathic traits in children". Criminal Behaviour and Mental Health. 19 (3): 178–192. doi:10.1002/cbm.732. PMID 19475645.
- Haun, Verena C.; Nübold, Annika; Bauer, Anna G. (2018-01-07). "Being mindful at work and at home: Buffering effects in the stressor-detachment model". Journal of Occupational and Organizational Psychology. 91 (2): 385–410. doi:10.1111/joop.12200. ISSN 0963-1798. S2CID 149204708.
- Christensen, Michael Cronquist; Fagiolini, Andrea; Florea, Ioana; Loft, Henrik; Cuomo, Alessandro; Goodwin, Guy M. (November 2021). "Validation of the Oxford Depression Questionnaire: Sensitivity to change, minimal clinically important difference, and response threshold for the assessment of emotional blunting". Journal of Affective Disorders. 294: 924–931. doi:10.1016/j.jad.2021.07.099. ISSN 0165-0327. PMID 34378539.
- "Chapter The Theory of Trauma-Related Structural Dissociation of the Personality", Dissociation and the Dissociative Disorders, Routledge, pp. 273–292, 2010-11-01, doi:10.4324/9780203893920-28, ISBN 978-0-203-89392-0, retrieved 2022-04-01
- Foa, Edna B.; Hearst-Ikeda, Diana (1996), Michelson, Larry K.; Ray, William J. (eds.), "Emotional Dissociation in Response to Trauma", Handbook of Dissociation: Theoretical, Empirical, and Clinical Perspectives, Boston, MA: Springer US, pp. 207–224, doi:10.1007/978-1-4899-0310-5_10, ISBN 978-1-4899-0310-5, retrieved 2021-03-22
- McCabe, Ciara; Mishor, Zevic; Cowen, Philip J.; Harmer, Catherine J. (2010). "Diminished Neural Processing of Aversive and Rewarding Stimuli During Selective Serotonin Reuptake Inhibitor Treatment". Biological Psychiatry. 67 (5): 439–445. doi:10.1016/j.biopsych.2009.11.001. PMC 2828549. PMID 20034615.
- "Emotional blunting: unresolved MDD symptom or effect of treatment?". Progress In Mind. 10 September 2019.
- Paradiso, Sergio; Ostedgaard, Katharine; Vaidya, Jatin; Ponto, Laura Boles; Robinson, Robert (2013-02-28). "Emotional blunting following left basal ganglia stroke: The role of depression and fronto-limbic functional alterations". Psychiatry Research: Neuroimaging. 211 (2): 148–159. doi:10.1016/j.pscychresns.2012.05.008. ISSN 0925-4927. PMC 4019790. PMID 23176970.
- Müller, M. J.; Kienzle, B.; Dahmen, N. (2002). "Depression, Emotional Blunting, and Akinesia in Schizophrenia: Overlap and Differentiation". The European Journal of Health Economics. 3: S99–S103. doi:10.1007/s10198-002-0114-9. ISSN 1618-7598. JSTOR 3570157. PMID 15609162. S2CID 42372770.
- Henry, Julie D.; Green, Melissa J.; de Lucia, Amber; Restuccia, Corinne; McDonald, Skye; O'Donnell, Maryanne (2007-09-01). "Emotion dysregulation in schizophrenia: Reduced amplification of emotional expression is associated with emotional blunting". Schizophrenia Research. 95 (1): 197–204. doi:10.1016/j.schres.2007.06.002. ISSN 0920-9964. PMID 17630254. S2CID 44415559.
- Reid, Marie; Wilson‐Walsh, Rebecca; Cartwright, Luke; Hammersley, Richard (May 2020). "Stuffing down feelings: Bereavement, anxiety and emotional detachment in the life stories of people with eating disorders". Health & Social Care in the Community. 28 (3): 979–987. doi:10.1111/hsc.12930. ISSN 0966-0410. PMID 31840343. S2CID 209384124.
- Allwood, Maureen A.; Bell, Debora J.; Horan, Jacqueline (2011). "Posttrauma numbing of fear, detachment, and arousal predict delinquent behaviors in early adolescence". Journal of Clinical Child and Adolescent Psychology. 40 (5): 659–667. doi:10.1080/15374416.2011.597081. ISSN 1537-4416. PMID 21916685. S2CID 205874162.
- Michal, Matthias; Koechel, Ansgar; Canterino, Marco; Adler, Julia; Reiner, Iris; Vossel, Gerhard; Beutel, Manfred E.; Gamer, Matthias (2013-09-13). "Depersonalization disorder: Disconnection of cognitive evaluation from autonomic responses to emotional stimuli". PLOS ONE. 8 (9): e74331. Bibcode:2013PLoSO...874331M. doi:10.1371/journal.pone.0074331. ISSN 1932-6203. PMC 3772934. PMID 24058547.
- Kaplan, Carola M. (September 2013). ""Sudden Holes in Space and Time": Trauma, Dissociation, and the Precariousness of Everyday Life". Psychoanalytic Inquiry. 33 (5): 467–478. doi:10.1080/07351690.2013.815064. ISSN 0735-1690. S2CID 219728825 – via EBSCO.
- Williams, Kipling D.; Nida, Steve A. (2011), Ostracism, Consequences and Coping, West Lafayette, IN: Purdue University