Running injuries
Running injuries (or running-related injuries, RRI) affect about half of runners annually. The frequencies of various RRI depend on the type of running, such as speed and mileage. Some injuries are acute, caused by sudden overstress, such as side stitch, strains, and sprains. Many of the common injuries that affect runners are chronic, developing over longer periods as the result of overuse. Common overuse injuries include shin splints, stress fractures, Achilles tendinitis, Iliotibial band syndrome, Patellofemoral pain (runner's knee), and plantar fasciitis.
| Running injuries | |
|---|---|
| Other names | Running-related injuries (RRI) |
| Specialty | Sports medicine |
Proper running form is important in injury prevention. A major aspect of running form is foot strike pattern. The way in which the foot makes contact with the ground determines how the force of the impact is distributed throughout the body. Different types of modern running shoes are created to adjust the foot strike pattern in an effort to reduce the risk of injury. In recent years, barefoot running has increased in popularity in many Western countries, because of claims that it reduces the risk of injury. However, this has not been proven and is still debated.
Overview
"The causes of running injuries are so multifactorial and diverse, and apparently vary greatly from individual to individual, that any preventive measure proposed would probably be of help to only a small minority. The only obvious exception would be, of course, the reduction in jogging activity itself. A recent study came to the same unspectacular conclusion. … We suspect, however, that it would be as difficult to motivate determined joggers to decrease their injury risk by cutting down on mileage as it would be to motivate the sedentary population to decrease its cardiovascular risk by taking up activities such as jogging."[1]
"A prospective cohort study of 300 runners followed for two years showed that 73 percent of women and 62 percent of men sustained an injury, with 56 percent of the injured runners sustaining more than one injury during the study period." [2]
A prospective cohort study of 76 runners followed for one year showed that 51 percent reported an injury. Injured runners were heavier. "Over 60% of male injured runners and over 50% of female injured runners had increased their weekly running distance by >30% between consecutive weeks at least once in the 4 weeks prior to injury." [3]
"… an evolutionary perspective indicates that we did not evolve to run long distances at fast speeds on a regular basis. As a result, it is unlikely there was selection for the human body to cope with some of the extreme demands runners place on their bodies."[4]
Acute injuries
Side stitch
A side stitch is an intense stabbing abdominal pain under the lower edge of the ribcage that occurs during exercise. It is also called a side ache, side cramp, muscle stitch, or simply a stitch, and the medical term is Exercise-related Transient Abdominal Pain (ETAP). It sometimes extends to shoulder tip pain, and commonly occurs during running, swimming, and horseback riding. Approximately two-thirds of runners will experience at least one episode of a stitch each year. The precise cause is unclear, although it most likely involves irritation of the abdominal lining, and the condition is more likely after consuming a meal or a sugary beverage. If the pain is present only when exercising and is completely absent at rest, in an otherwise healthy person, it does not require investigation. Typical treatment strategies involve deep breathing and/or manual pressure on the affected area.[5][6][7]
Strains
A strain is an injury that occurs to a muscle, tendon, or both. Generally, the muscle or tendon overstretches and partially tears, under more physical stress than it can withstand,[8] often from a sudden increase in duration, intensity, or frequency of an activity. Strains most commonly occur in the foot, leg, or back.[9] Immediate treatment typically includes five steps abbreviated as PRICE: protection, rest, ice, compression, elevation.[10]
Sprains
A sprain, also known as a torn ligament, is the stretching or tearing of ligaments within a joint, often caused by an injury abruptly forcing the joint beyond its functional range of motion. Ligaments are tough, inelastic fibers made of collagen that connect two or more bones to form a joint.[11] Sprains can occur at any joint but most commonly occur in the ankle, knee, or wrist.[12] The majority of sprains are mild, causing minor swelling and bruising that can be resolved with conservative treatment, typically summarized as RICE: rest, ice, compression, elevation. However, severe sprains involve complete tears, ruptures, or fractures, often leading to joint instability, severe pain, and decreased functional ability. These sprains require surgical fixation, prolonged immobilization, and physical therapy.[13]
Morton's neuroma
Morton's neuroma is a tightening of the tissues surrounding the nerves leading into your toes. [14] This is caused by wearing shoes with a narrow toe bed, like high heels, or in high-impact activities like running or jogging. Treatments can include switching to a shoe with a wider toe bed, the use of inserts in your shoe, cortisol shots, or in extreme cases, surgery can be done to remove the affected nerve.
Overuse injuries
Causes and prevention
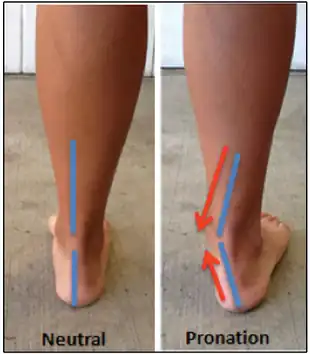
In general, overuse injuries are the result of repetitive impact between the foot and the ground. With improper running form, the force of the impact can be distributed abnormally throughout the feet and legs. Running form tends to worsen with fatigue. When moving at a constant pace along a straight path, a symmetrical gait is considered to be normal. Asymmetry is considered to be a risk factor for injury. One study attempted to quantify the change in running form between a rested and fatigued state by measuring asymmetrical running gait in the lower limbs. The results showed that "knee internal rotation and knee stiffness became more asymmetrical with fatigue, increasing by 14% and 5.3%, respectively."[15] These findings suggest that focusing on proper running form, particularly when fatigued, could reduce the risk of running-related injuries. Running in worn-out shoes may also increase the risk of injury, and altering the footwear might be helpful. These injuries can also arise due to a sudden increase in the intensity or amount of exercise.
Shin splints
A shin splint, also known as Medial Tibial Stress Syndrome (MTSS), is pain along the inside edge of the shinbone (tibia) due to inflammation of tissue in the area. Generally this is between the middle of the lower leg to the ankle. The pain may be dull or sharp, and is generally brought on by high-impact exercise that overloads the tibia. Groups that are commonly affected include runners (especially on concrete or asphalt), dancers, gymnasts, and military personnel. Rates of shin splints in at-risk groups range from 4% to 35%. The condition occurs more often in women. Shin splints are generally treated by rest followed by a gradual return to exercise over a period of weeks.[16][17]
Stress fractures
A stress fracture is a fatigue-induced bone fracture caused by repeated stress over time. Instead of resulting from a single severe impact, stress fractures are the result of accumulated injury from repeated submaximal loading, such as running or jumping. Because of this mechanism, stress fractures are common overuse injuries in athletes.[18]
Stress fractures can be described as small cracks in the bone, or "hairline fractures". Stress fractures of the foot are sometimes called "march fractures" because of the injury's prevalence among heavily marching soldiers.[19] Stress fractures most frequently occur in weight-bearing bones of the lower extremities, such as the tibia and fibula (bones of the lower leg), metatarsal and navicular bones (bones of the foot). Less common are stress fractures to the femur, pelvis, and sacrum. Treatment usually consists of rest followed by a gradual return to exercise over a period of months.[18]
Achilles tendinitis
Achilles tendinitis is inflammation of the Achilles tendon, resulting in pain along the back of the leg near the heel. There are two types of Achilles tendinitis, insertional and noninsertional. Noninsertional Achilles tendinitis is the type that more commonly affects runners. In this case, inflammation is occurring in the middle portion of the tendon, whereas insertional Achilles tendinitis is inflammation located where the tendon connects (inserts) to the heel bone. Having tight calf muscles may also increase the risk of Achilles tendinitis. Stretching the calves before starting heavy exercise may help relieve tightness in the muscles.[20]
Patellofemoral pain syndrome
Patellofemoral pain syndrome is associated with pain in the knee and around the patella (kneecap). It is sometimes referred to as runner's knee, but this term is also used for other overuse injuries that involve knee pain. It can be caused by a single incident but is often the result of overuse or a sudden increase in physical activity. Patellofemoral pain syndrome is often mistaken for Chondromalacia patellae which is another condition commonly referred to as 'Runner's Knee'. This is because both of them involve pain in or around the patella (knee cap) and this is how they are distinguished from other running injuries like Patellar Tendonitis (Jumper's Knee).[21]
Iliotibial band syndrome

Iliotibial band syndrome (ITBS) is defined as inflammation of the iliotibial band on the outside of the knee. This inflammation occurs a result of the iliotibial band and the outside of the knee joint rubbing together. The resulting pain typically is initially mild and worsens if running continues. Recurrence is a common issue with iliotibial band syndrome, as pain goes away with a period of rest, but symptoms can easily come back as the runner returns to training. During recovery, the muscles on the outside of the hip can be stretched to reduce tightness in the band.
Plantar fasciitis
The plantar fascia extends from the heel bone to the toes, and helps support the arch of the foot.[22] Plantar fasciitis is a common cause of heel pain and affects about two million people in the United States. Though once considered an inflammatory condition, plantar fasciitis is now characterized as a degenerative pathology. Intrinsic risk factors include obesity and limited ankle flexibility. Extrinsic risk factors include deconditioning, hard surfaces, inadequate stretching and poor footwear.[23]
Footwear
Traditional running shoes
Study participants wearing running shoes with moderate lateral torsional stiffness "were 49% less likely to incur any type of lower extremity injury and 52% less likely to incur an overuse lower extremity injury than" participants wearing running shoes with minimal lateral torsional stiffness, both of which were statistically significant observations." [24] Lateral torsional stiffness can be assessed simply by twisting the heel and toe in opposite directions.[25]
In the 1984 Bern 16 km race questionnaire, runners who had no shoe brand preference and presumably changed brands frequently had significantly fewer running injuries. There was also some correlation between higher shoe price and increased injury but — "It is probably incorrect, however, to interpret this surprising finding to mean that more expensive shoes cause more running injuries…". That group was 1 1⁄2 minutes slower than expected from their training and had a higher proportion of orthotics use. It may well be that runners with existing injuries hope that expensive shoes will fix their body. [26]
So-called "traditional" running shoes are designed to give more support and cushion the landing to reduce the effects of impact. They allow for more-comfortable running on hard surfaces such as asphalt and also protect the foot when stepping on rocks or other potentially sharp objects. However, "perceived impact is lower than actual impact, which results in inadequate impact-moderating behavior and consequent injury" — too much running. [27]
Barefoot running
Barefoot running has been promoted as one method of reducing the risk of running-related injuries. Barefoot running is thought to improve running form by encouraging forefoot striking. The collision of the forefoot with the ground generates a significantly smaller impact force in comparison to striking heel first.[28] However, barefoot running leaves the foot unprotected from stepping on sharp objects. Although running barefoot may reduce the risk of running-related injuries, it is important to take time while switching from running with shoes.
Beginning to run barefoot without reducing intensity or mileage of training can actually cause muscle or tendon injury. Changing one's style of running shoe or switching to barefoot running will most likely alter the foot strike pattern, meaning that the force of impact will be absorbed differently. Injuries are more likely to occur in novice barefoot runners. This may be a result of not yet having fully adapted to a new style of running, and therefore running with inconsistent technique. To measure this, a study was conducted involving runners who habitually run with a rearfoot strike while wearing shoes. Of the runners involved in the study, 32% used a heel strike pattern in initial attempts at running barefoot. Running barefoot while heel striking leads to increased muscle activation and impact accelerations.[29] The findings suggest that an inconsistency in running technique among novice barefoot runners may put them at a higher risk of injury in comparison to running with shoes.
Minimalist footwear
As an intermediate option between traditional running shoes and running barefoot, "minimalist" shoes lack thickly cushioned heels and are designed to encourage forefoot striking.[30] Compared to traditional running shoes, one study observed that high-speed runners in minimalist shoes experienced a significant redistribution of mechanical work from the knee to the ankle.[31] Therefore, minimalist shoes may be beneficial for runners who have experienced a knee injury in the past, although the shoes might increase the risk of ankle and calf injuries. As with barefoot running, runners who switch to minimalist shoes should not start out at full training intensity.
References
- Marti, Bernard; Vader, John Paul; Minder, Christoph E.; Abelin, Theodor (May–Jun 1988). "On the epidemiology of running injuries: The 1984 Bern Grand-Prix study". American Journal of Sports Medicine. 16 (3): 285–294. doi:10.1177/036354658801600316. PMID 3381988. S2CID 41199266.
- Callahan, Lisa R. (4 October 2022). "Overview of running injuries of the lower extremity". Wolters Kluwer.
- Winter, Sara C.; Gordon, Susan; Brice, Sara M.; Lindsay, Daniel; Barrs, Sue (May 2020). "A Multifactorial Approach to Overuse Running Injuries: A 1-Year Prospective Study". Sports Health. 12 (3): 296–303. doi:10.1177/1941738119888504. PMC 7222667. PMID 31994970.
- Lieberman, Daniel E. (2017). "History of Distance Running". In Waite, Brandee L.; Krabak, Brian J.; Lipman, Grant S. (eds.). The Long Distance Runner's Guide to Injury Prevention and Treatment. Skyhorse Publishing. pp. 2–17.
- Morton, Darren P.; Callister, Robin (February 2000). "Characteristics and etiology of exercise-related transient abdominal pain". Medicine & Science in Sports & Exercise. 32 (2): 432–438. doi:10.1097/00005768-200002000-00026. PMID 10694128.
- Morton, Darren P.; Callister, Robin (January 2015). "Exercise-Related Transient Abdominal Pain (ETAP)". Sports Medicine. 45 (1): 23–35. doi:10.1007/s40279-014-0245-z. PMC 4281377. PMID 25178498. S2CID 18088581.
- Wetsman, Nicole (20 October 2017). "When you get a stitch in your side, what's really going on?". Popular Science. Retrieved 30 November 2020.
- "Sprains and Strains: In-Depth". National Institutes of Health. January 2015. Retrieved 1 December 2020.
- Mulcahey, Mary K. (June 2020). "Sprains, Strains and Other Soft-Tissue Injuries". OrthoInfo. American Academy of Orthopaedic Surgeons. Retrieved 1 December 2020.
- Järvinen, T.A.H.; et al. (April 2007). "Muscle injuries: optimising recovery". Best Practice & Research: Clinical Rheumatology. 21 (2): 317–331. doi:10.1016/j.berh.2006.12.004. PMID 17512485.
- Bahr, Roald; Alfredson, Håkan; Järvinen, Markku; Järvinen, Tero; Khan, Karim; Kjaer, Michael; Matheson, Gordon; Maehlum, Sverre (2012-06-22), Bahr, Roald (ed.), "Types and Causes of Injuries", The IOC Manual of Sports Injuries, Wiley-Blackwell, pp. 1–24, doi:10.1002/9781118467947.ch1, ISBN 978-1-118-46794-7
- Hartshorne, Henry. "Sprained Joints". The Home Cyclopedia Of Health And Medicine. Retrieved 1 December 2020.
- "Ligament Sprain". Physiopedia. Retrieved 1 December 2020.
- "Morton's neuroma - Symptoms and causes". Mayo Clinic.
- Radzak, Kara N.; Putnam, Ashley M.; Tamura, Kaori; Hetzler, Ronald K.; Stickley, Christopher D. (January 2017). "Asymmetry between lower limbs during rested and fatigued state running gait in healthy individuals". Gait & Posture. 51: 268–274. doi:10.1016/j.gaitpost.2016.11.005. ISSN 1879-2219. PMID 27842295.
- Alaia, Michael J. (August 2019). "Shin Splints". OrthoInfo. American Academy of Orthopaedic Surgeons. Retrieved 30 November 2020.
- Reshef, N; Guelich, DR (April 2012). "Medial tibial stress syndrome". Clinics in Sports Medicine. 31 (2): 273–290. doi:10.1016/j.csm.2011.09.008. PMID 22341017.
- Behrens, Steve; Deren, Matson; Fadale, Monchik (March–April 2013). "Stress Fractures of the Pelvis and Legs in Athletes: A Review". Sports Health: A Multidisciplinary Approach. 5 (2): 165–174. doi:10.1177/1941738112467423. PMC 3658382. PMID 24427386.
- Payne, Jacqueline (26 March 2018). "Metatarsal Fractures". Patient.info. Retrieved 30 November 2020.
- Kadakia, Anish R. (June 2010). "Achilles Tendinitis". OrthoInfo. American Academy of Orthopaedic Surgeons. Retrieved 30 November 2020.
- "Runner's Knee & Jumper's Knee pain relief and treatment". www.physique.co.uk. Retrieved 2022-08-10.
- Petraglia, Federica; Ramazzina, Ileana; Costantino, Cosimo (10 May 2017). "Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review". Muscles, Ligaments and Tendons Journal. 7 (1): 107–118. doi:10.11138/mltj/2017.7.1.107. PMC 5505577. PMID 28717618.
- Schwartz, Emily N.; Su, John (Winter 2014). "Plantar fasciitis: a concise review". The Permanente Journal. 18 (1): 105–117. doi:10.7812/TPP/13-113. PMC 3951039. PMID 24626080.
- Helton, Gary L.; et al. (October 2019). "Association Between Running Shoe Characteristics and Lower Extremity Injuries in United States Military Academy Cadets". The American Journal of Sports Medicine. 47 (12): 2853–2862. doi:10.1177/0363546519870534. PMID 31498686. S2CID 198305119.
- Williams, Bruce E. (March 2010). "A three-point approach to testing running shoes". Lower Extremity Review.
- Marti, B. (1989). "Relationships between Running Injuries and Running Shoes — Results of a Study of 5,000 Participants of a 16-km Run — The May 1984 Berne Grand Prix". In Segesser, B.; Pförringer, W. (eds.). The Shoe in Sport. Year Book Medical Publishers. pp. 256–265. ISBN 9780815178149.
- Robbins, Steven E.; Gouw, Gerard J. (1991). "Athletic footwear: unsafe due to perceptual illusions" (PDF). Medicine & Science in Sports & Exercise. 23 (2): 217–224. doi:10.1249/00005768-199102000-00012. PMID 2017018.
- Lieberman, Daniel. "Running Barefoot: Biomechanics of Foot Strike". Harvard University. Retrieved 9 February 2017.
- Lucas-Cuevas, Angel Gabriel; Priego Quesada, José Ignacio; Giménez, José Vicente; Aparicio, Inma; Jimenez-Perez, Irene; Pérez-Soriano, Pedro (November 2016). "Initiating running barefoot: Effects on muscle activation and impact accelerations in habitually rearfoot shod runners". European Journal of Sport Science. 16 (8): 1145–1152. doi:10.1080/17461391.2016.1197317. ISSN 1536-7290. PMID 27346636. S2CID 23392717.
- Lieberman, Daniel. "Running Barefoot: Heel Striking & Running Shoes". Harvard University. Retrieved 30 November 2020.
- Fuller, Joel T.; Buckley, Jonathan D.; Tsiros, Margarita D.; Brown, Nicholas A. T.; Thewlis, Dominic (1 October 2016). "Redistribution of Mechanical Work at the Knee and Ankle Joints During Fast Running in Minimalist Shoes". Journal of Athletic Training. 51 (10): 806–812. doi:10.4085/1062-6050-51.12.05. ISSN 1938-162X. PMC 5189234. PMID 27834504.