Sleep problems in women
Sleep problems in women can manifest at various stages of their life cycle. Both subjective and objective data indicate that women are at an increased risk of experiencing different types of sleeping problems during different life stages.[1][2][3][4][5] Factors such as hormonal changes, aging, psycho-social aspects, physical and psychological conditions, and the presence of sleeping disorders can disrupt women's sleep.[1][2][3][4][5] Research supports the presence of disturbed sleep during the menstrual cycle, pregnancy, postpartum period, and menopausal transition.[1][2][3][4][5] The relationship between sleep and women's psychological well-being suggests that the underlying causes of sleep disturbances are often multi-factorial throughout a woman's lifespan.[1][2][3][4][5]
Sleep during menstrual cycle
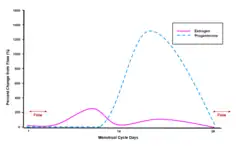
Initial variations of sleep in women begin with the menstrual cycle.[2] In subjective studies, women who report PMS or PMDD report increases in poor sleep quality.[6] However, most objective laboratory-based PSG measures of young healthy women do not confirm irregular sleep patterns, neither in sleep duration nor sleep quality across the menstrual cycle.[1] One exception is the reduction of REM sleep and markedly more so the increase of Stage 2 sleep during the luteal phase of the menstrual cycle.[1][2] Several studies attribute this to increased estrogen and progesterone concentrations.[7] One actigraphy study reports a modest decline in total sleep time of 25 min in late-reproductive woman during the premenstrual week.[1] The measurement of subjectively reported sleep during the menstrual cycle differs.[2] Seventy percent of women report a negative impact on their sleep.[2] Furthermore, they report a decrease in sleep quality on 2.5 days each month.[2] Poor sleep quality, connected with poor mood and menstrual pain, especially during the premenstrual week, are most likely to be reported.[1] Psychological factors influencing sleep quality in women, related to hormonal fluctuations, such as mood disorders and sleep disorders, are often higher in women after the onset menarche.[2]
Sleep during pregnancy
An estimated 46% of women experience subjectively poor sleep during pregnancy and this percentage increases progressively up to approximately 78% in the late stages of pregnancy.[2][8] Reasons vary according to the trimester, relating to hormonal changes and physical discomfort:[1] anatomic changes, sleep fragmentation, fragmentation of breathing, metabolic changes which might increase sleep disorders such as restless leg syndrome, gastroesophageal reflux, increase in overnight sodium excretion, changes in the musculoskeletal system, nocturnal uterine contractions, changes in iron and folate metabolism, and changes in the circadian and homeostatic regulation of sleep.[2]
First trimester
Laboratory-based studies show that most women experience more disruption during night-time sleep and become sleepier. They sleep on average more during this time compared to pre-pregnancy sleep time.[1][2] Total sleep time, however, decreases as the pregnancy progresses.[5] Nocturia and musculoskeletal discomfort account for the physiological factors impacting sleep during the first trimester.[2] Subjectively, women report an increase in night-time awakening and an increase in total sleep time.[1] Pregnant women's main physiological complaints during the first trimester which disrupt the quality of sleep are nausea and vomiting, urinary frequency, backaches, and feeling uncomfortable and fatigued; as well as tender breasts, headache, vaginal discharge, flatulence, constipation, shortness of breath, and heartburn.[1][5] Other contributing factors for sleep quality are age, parity, mood disorders, anxiety and primary sleep disorders.[1]
Second trimester
Laboratory based measures during the second trimester show a further decrease in total sleep time, slow-wave sleep and sleep quality.[1][2] No changes in REM sleep have been observed.[1] Fetal movements, uterine contractions, musculoskeletal discomfort and rhinitis and nasal congestion account for the physiological factors which influence sleep.[2] Self-reported total sleep time and quality decreases during the second trimester.[2] Reported contributing factors are fetal movements, heartburn, cramps or tingling in the legs, breathing problems, and anxiety.[1]
Third trimester
Objectively, slow-wave sleep and total sleep time as well as general sleep quality decreases further progressively during the third trimester.[1][2] More night-time awakenings are common.[1][2] Sleep onset latency problems and napping becomes more frequent.[1] Physiological factors impacting sleep at this stage during the pregnancy are nocturia, fetal movement, uterine contractions, heartburn, orthopnea, leg cramps, rhinitis, nasal congestion, and sleeping position.[2] Women at the third trimester report progressively reduced Total Sleep Time, and similarly to the second trimester, being uncomfortable, feeling fetal movements, heartburn, frequent urination, cramps and respiratory difficulties.[1] The last weeks before delivery influence sleep quality reportedly most markedly.[1] It is, however, curious that in spite of virtually all women experiencing poor sleep, only one third consider themselves to have current sleep problems.[1]
Postpartum
Total sleep time is objectively the lowest during the 1 month postpartum though it steadily increases toward normal.[1] Main contributing factors influencing sleep during the postpartum period are infant behaviours such as infant sleep and feeding patterns, bed-sharing and infant temperament.[1][2] It appears that slow-wave sleep is preserved during the first weeks postpartum in spite and because of chronic sleep deprivation.[1] Frequent napping occurs.[1] Recent studies suggest additionally a myriad of further contributing factors influencing postpartum sleep.[1][2] It has been found that multiparas sleep remained relatively stable while first time mothers experienced a decline in sleep efficiency.[3] Furthermore, mothers of bottle-fed babies experienced less night-time awakening than breast feeding mothers.[1][2] Parents general physical and psychological health should be considered as well; however, by three months postpartum, mothers' and infants' sleep tend to stabilise and mothers' sleep becomes more regular.[1][2]
Menopausal transition
Poor sleep quality, sleep fragmentation and increased awakenings are common complaints during the menopausal transition.[1][2][3][5] Reportedly, 31% to 42% of women suffer from chronic insomnia during their menopausal transition.[2] However, some objective PSG studies have not shown significant differences in sleep architecture in pre‐, peri‐, and postmenopausal women.[1][2][3][5] Nonetheless, quantitative and qualitative studies report elevated beta activity, resulting objectively and subjectively in a consistent coupling of sleep disturbances such as sleep fragmentation, increased waking after sleep onset and poor sleep efficiency with vasomotor symptoms such as hot flashes.[1][2][3][5] Besides vasomotor symptoms are changes in hormone levels such as estrogen, affective disorders, stress and perceived health, urinary problems, obesity, gastrointestinal problems, endocrine problems, and cardiovascular problems contributing factors to menopause' associated sleeping problems and insomnia.[1][2][3][4][5] Sleep during the menopausal transition is furthermore influenced by pain disorders and specifically by comorbid physical and psychiatric conditions.[1][2][4] Other proposed causes for sleep problems during menopause are increased incidences of obstructive sleep apnea, increased sleep disordered breathing, and inadequate sleep hygiene.[4][5] Another important factor contributing to changed sleep patterns in ageing women in general is the circadian disruption, showing in disturbed regulation of body temperature at sleep onset and early morning cortisol levels.[2] Postmenopausal women tend to express a morning chronotype.[2] These changes in chronotype compared to premenopausal women require a different sleep hygiene.[1]
References
- Moline M, Broch L, Zak R (July 2004). "Sleep Problems Across the Life Cycle in Women". Current Treatment Options in Neurology. 6 (4): 319–330. doi:10.1007/s11940-004-0031-6. PMID 15157409. S2CID 11011868.
- Bei B, Coo S, Baker FC, Trinder J (2015). "Sleep in Women: A Review". Australian Psychologist. 50 (1): 14–24. doi:10.1111/ap.12095. ISSN 1742-9544. S2CID 70400873.
- Pengo MF, Won CH, Bourjeily G (July 2018). "Sleep in Women Across the Life Span". Chest. 154 (1): 196–206. doi:10.1016/j.chest.2018.04.005. PMC 6045782. PMID 29679598.
- Ameratunga D, Goldin J, Hickey M (July 2012). "Sleep disturbance in menopause". Internal Medicine Journal. 42 (7): 742–7. doi:10.1111/j.1445-5994.2012.02723.x. PMID 22288870. S2CID 39014698.
- Gava G, Orsili I, Alvisi S, Mancini I, Seracchioli R, Meriggiola MC (October 2019). "Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy". Medicina. 55 (10): 668. doi:10.3390/medicina55100668. PMC 6843314. PMID 31581598.
- Meers, Jessica M.; Nowakowski, Sara (August 2020). "Sleep, premenstrual mood disorder, and women's health". Current Opinion in Psychology. 34: 43–49. doi:10.1016/j.copsyc.2019.09.003. ISSN 2352-2518. PMID 31610482. S2CID 204044995.
- Mehta, Navina; Shafi, Fariha; Bhat, Abid (2015). "Unique Aspects of Sleep in Women". Missouri Medicine. 112 (6): 430–434. ISSN 0026-6620. PMC 6168103. PMID 26821442.
- "National Sleep Foundation". National Sleep Foundation. Retrieved 2022-10-03.