Strangles
Strangles (equine distemper) is a contagious upper respiratory tract infection of horses and other equines caused by a Gram-positive bacterium, Streptococcus equi.[1] As a result, the lymph nodes swell, compressing the pharynx, larynx, and trachea, and can cause airway obstruction leading to death, hence the name strangles.[2] Strangles is enzootic in domesticated horses worldwide. The contagious nature of the infection has at times led to limitations on sporting events.[3]
Signs

.jpg.webp)
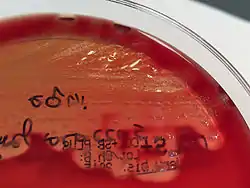
A horse with strangles typically develops abscesses in the lymph nodes of the head and neck, causing coughing fits and difficulty swallowing. Clinical signs include fever up to 106°F and yellow-coloured nasal discharge from both the nose and eyes.[2]
Abscesses may form in other areas of the body, such as the abdomen, lungs, and brain.[1] This is considered a chronic form of strangles called "bastard strangles", which can have serious implications if the abscesses rupture. Horses develop this form of strangles when their immune systems are compromised or if the bacteria rapidly invade the body.[2]
Complications
Possible complications include the horse becoming a chronic carrier of the disease, asphyxia due to enlarged lymph nodes compressing the larynx or windpipe, bastard strangles (spreading to other areas of the body), pneumonia, guttural pouch filled with pus, abscesses, purpura haemorrhagica, and heart disease. The average course of this disease is 23 days.
Cause
The disease is spread by an infected horse when nasal discharge or pus from the draining lymph nodes contaminate pastures, feed troughs, brushes, bedding, tack, etc.[2]
Prevention
Both intramuscular[4] and intranasal[5] vaccines are available, although their efficacy is rated at no more than 50%.[6] Isolation of new horses for four to six weeks, immediate isolation of infected horses, and disinfection of stalls, water buckets, feed troughs, and other equipment can help prevent the spread of strangles.[6] As with any contagious disease, hand washing is a simple and effective tool.[7]
Treatment
As with many streptococcal infections, beta-lactam antibiotics (e.g penicillins) are the most effective treatments, but some authorities are of the opinion that use of antibiotics is contraindicated once abscesses have begun to form, as they predispose to lymphatic spread of the infection (bastard strangles), which has a much higher mortality rate.
After an abscess has burst, keeping the wound clean is important. A diluted povidone-iodine solution has been used with good results to disinfect the open hole, flushing the inside with a syringe-tipped catheter or with a teat cannula, followed by gentle scrubbing to keep the surrounding area clean.
Symptomatic therapy is an alternative treatment, and is where warm packs are used to mature the abscesses so making them less painful and more comfortable for the horse, but once the abscesses have been matured, they must be kept clean to prevent further infections. This treatment for S. equi only helps reduce pain for the horse rather than curing the infection.
Outcomes
Strangles has an 8.1% mortality rate.[2] Mortality is lower in cases without complications than it is in cases of bastard strangles. The disease is very contagious and morbidity is high. Precautions to limit the spread of the illness are necessary and those affected are normally isolated. An isolation period of 4–6 weeks is usually necessary to ensure that the disease is not still incubating before ending the quarantine.
Epidemiology
Equines of any age may contract the disease, although younger and elderly equines are more susceptible. Young equines may lack immunity to the disease because they have not had prior exposure. Geriatric equines may have a weaker immune system.
See also
References
- "Strangles in Horses". www.omafra.gov.on.ca. Archived from the original on 2019-10-30. Retrieved 2016-11-24.
- "Equine Strangles" (PDF). 2008. Retrieved November 23, 2016.
- "Race club downplays 'strangles' impact". ABC.au News. 1 May 2012. Retrieved 16 May 2012.
- Robinson, Carl; et al. (2020). "Intramuscular vaccination with Strangvac is safe and induces protection against equine strangles caused by Streptococcus equi". Vaccine. 38 (31): 4861–4868. doi:10.1016/j.vaccine.2020.05.046. PMID 32507408. S2CID 219538289.
- Florindo, H. F.; et al. (2009). "The enhancement of the immune response against S. equi antigens through the intranasal administration of poly-ɛ-caprolactone-based nanoparticles". Biomaterials. 30 (5): 879–89. doi:10.1016/j.biomaterials.2008.10.035. PMID 19027152.
- Boyle, A. G.; Timoney, John F.; Newton, J. R.; Hines, M. T.; Waller, A. S.; Buchanan, B. R. (2018). "Streptococcus equi infections in horses: guidelines for treatment, control, and prevention of strangles—revised consensus statement". Journal of Veterinary Internal Medicine. 32 (2): 633–647. doi:10.1111/jvim.15043. PMC 5867011. PMID 29424487.
- Rendle, David; et al. (2021). "Streptococcus equi infections: current best practice in the diagnosis and management of 'strangles'". UK-Vet Equine. 5 (Sup2): S3–S15. doi:10.12968/ukve.2021.5.2.S.3. S2CID 233854031.