Video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery (VATS) is a type of minimally invasive thoracic surgery performed using a small video camera mounted to a fiberoptic thoracoscope (either 5 mm or 10 mm caliber), with or without angulated visualization, which allows the surgeon to see inside the chest by viewing the video images relayed onto a television screen, and perform procedures using elongated surgical instruments. The camera and instruments are inserted into the patient's chest cavity through small incisions in the chest wall, usually via specially designed guiding tubes known as "ports".
| Video-assisted thoracoscopic surgery | |
|---|---|
_CRUK_378.svg.png.webp) Diagram showing video assisted thoracoscopy (VATS) | |
| MeSH | D020775 |
VATS procedures are done using either conventional surgical instruments or laparoscopic instruments. Unlike with laparoscopy, carbon dioxide insufflation is not generally required in VATS due to the inherent rigidity of the thoracic cage. However, lung deflation on the side of the operated chest is a must to be able to visualize and pass instruments into the thorax; this is usually effected with a double-lumen endotracheal tube that allows for single-lung ventilation, or a one-side bronchial occlusion delivered via a standard single-lumen tracheal tube.[1]
History
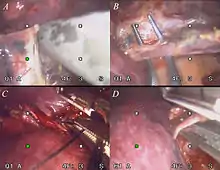
VATS came into widespread use beginning in the early 1990s. Operations that traditionally were carried out with thoracotomy or sternotomy that today can be performed with VATS include: biopsy for diagnosis of pulmonary, pleural or mediastinal pathology; decortication for empyema; pleurodesis for recurrent pleural effusions or spontaneous pneumothorax; surgical stapler-assisted wedge resection of lung masses; resection of mediastinal or pleural masses; thoracic sympathectomy for hyperhidrosis; operations for diaphragmatic hernias or paralysis; esophageal resection or resection of esophageal masses or diverticula; and VATS lobectomy/mediastinal lymphadenectomy for lung cancer.[1]
Similarly to laparoscopy, VATS has enjoyed widespread use for technically straightforward operations such as pulmonary decortication, pleurodesis, and lung or pleural biopsies, while more technically demanding operations such as esophageal operations, mediastinal mass resections, or pulmonary lobectomy for early stage lung cancer, have been slower to catch on and have tended to remain confined to selected centers. It is expected that advanced VATS techniques will continue to grow in numbers spurred by patient demand and greater surgeon comfort and familiarity with the techniques.
Benefits
The main advantage of VATS is that the smaller postoperative wounds drastically reduce the risk for wound infection and dehiscence, which allows for a faster recovery by the patient and a greater chance for the wound to heal.[1]
Traditional thoracic surgery requires opening the chest through thoracotomy or sternotomy incisions, which are significantly traumatic to the body. Sternotomy requires the use of a sternal saw to split the sternum and a retractor to spread apart the divided sternum to allow visualization and access to the thoracic structures. Thoracotomy, as most commonly performed, requires division of one or more major muscles of the chest wall including the latissimus, pectoralis or serratus muscles, along with spreading of the ribs with a rib spreader. Because the costovertebral joints have only limited flexibility, the use of a rib spreader usually results in iatrogenic rib fractures, which can lead to complications like a flail chest or intercostal neuralgia. Because of this, thoracic surgeons generally intentionally use a bone cutter to remove section of one or more ribs in an effort to prevent jagged rib fractures. Although sternotomy and thoracotomy have been proven over decades to provide highly effective access to thoracic structures and in general are tolerated by patients, both incisions have the potential for causing significant pain that may last for extended periods and both prevent the patients from heavy lifting or strenuous activity for weeks in order to heal, and can still result in malunions and nonunions. The great advantage of VATS over sternotomy or thoracotomy is the avoidance of muscle division and bone-cutting, which allows for reduced postoperative pain, shorter duration of hospital stay and quicker return to full activity.[2]
See also
References
- Shields, Thomas (2004). General Thoracic Surgery. Lippincott Williams & Wilkins. p. 524. ISBN 978-0-7817-3889-7.
- Chai, Tianci; Lin, Yuhan; Kang, Mingqiang; Lin, Jiangbo (March 2019). "Thoracotomy versus video-assisted thoracoscopic resection of lung cancer: A protocol for a systematic review and meta-analysis". Medicine. 98 (10): e14646. doi:10.1097/MD.0000000000014646. ISSN 0025-7974. PMC 6417539.
Further reading
- Calvin SH Ng, Song Wan, Tak Wai Lee, Innes YP Wan, Ahmed Arifi, Anthony PC Yim. Video-assisted thoracic surgery in spontaneous pneumothorax. Can Respir J 2002;9:122-127
- Calvin SH Ng, Song Wan, Tak Wai Lee, Alan DL Sihoe, Innes YP Wan, Ahmed A Arifi, Anthony PC Yim. Video assisted thoracoscopic surgery for mediastinal extramedullary haematopoiesis. Ann R Coll Surg Engl 2002;84:161-163
- Calvin SH Ng, Song Wan, Anthony PC Yim. Paradigm shift in surgical approaches to spontaneous pneumothorax: VATS. Thorax 2004;59:357
- Calvin SH Ng, Tak Wai Lee, Song Wan, Innes YP Wan, Alan DL Sihoe, Ahmed A Arifi, Anthony PC Yim. Thoracotomy is associated with significantly more profound suppression in Lymphocytes and Natural Killer cells than Video-Assisted Thoracic Surgery following major lung resections for cancer. J Invest Surg 2005;18:81-88
- Calvin SH Ng, Tak Wai Lee, Song Wan, Anthony PC Yim. Video-Assisted Thoracic Surgery in the Management of Spontaneous Pneumothorax: The Current Status. Postgrad Med J 2006;82:179-185
- Calvin SH Ng, Song Wan, Malcolm J Underwood, Anthony PC Yim. VATS and Extramedullary Haematopoiesis. Eur Resp J 2006;28:255-6
- Juan C Garzon, Calvin SH Ng, Alan D Sihoe, Anthony V Manlulu, Randolph HL Wong, Tak Wai Lee, Anthony PC Yim. Video-Assisted Thoracic Surgery Pulmonary Resection for Lung Cancer in Patients with Poor Lung Function. Ann Thorac Surg 2006;81:1996-2003
- Calvin SH Ng, Anthony PC Yim. Spontaneous Hemopneumothorax. Curr Opin Pulm Med 2006;12:273-277
- Calvin SH Ng, Song Wan, Connie WC Hui, Tak Wai Lee, Malcolm J Underwood, Anthony PC Yim. Video-Assisted Thoracic Surgery for Early Stage Lung Cancer – Can short-term immunological advantages improve long-term survival? Ann Thorac Cardiovasc Surg 2006;12:308-12
- Calvin SH Ng, Song Wan, Connie WC Hui, Innes YP Wan, Tak Wai Lee, Malcolm J Underwood, Anthony PC Yim. VATS lobectomy for lung cancer is associated with less immunochemokine disturbances than thoracotomy. Eur J Cardiothorac Surg 2007;31:83-7
- Juan C Garzon, Calvin SH Ng, Tak Wai Lee, Anthony PC Yim. Video-assisted Thoracic Surgery for Pneumothorax in LAM. Heart Lung Circ 2007;16: 300-302
- Calvin SH Ng, Innes YP Wan, Anthony PC Yim. Impact of Video-Assisted Thoracoscopic Major Lung Resection on Immune Function. Asian Cardiovasc Thorac Annals 2009;17:426-432
- Calvin SH Ng, Anthony PC Yim. Videothoracoscopic Approach to Posterior Mediastinal Tumors. Mineo TC (eds). Thoracic Surgery Clinics 2010 May; 20(2):297-309
- Calvin SH Ng, Innes YP Wan, Anthony PC Yim. VATS Thymectomy- The Better Approach. Ann Thorac Surg 2010;89: S2135
- Wong RHL, Ng CSH, Wong JKW, Tsang S. Needlescopic video-assisted thoracic surgery for reversal of thoracic sympathectomy. Interact CardioVasc Thorac Surg 2012;14:350-2
- Ng CSH, Wong RHL, Yeung ECL, Kwok MWT, Lau RWH, Ho AMH, Yim APC, Underwood MJ. Needlescopic Video-Assisted Thoracoscopic Pericardial Window. Surgical Practice 2012;16(2):84-5
- Ng CSH, Wan S, Wong RHL, Ho AMH, Yim APC. Angiogenic Response to Major Lung Resection for Non-Small Cell Lung Cancer with Video-Assisted Thoracic Surgical and Open Access. ScientificWorldJournal. 2012;2012:636754
- Ng CSH, Yeung ECL, Wong RHL, Kwok WT. Single-port Sympathectomy for Palmar Hyperhidrosis with VasoView: HemoPro 2 Endoscopic Vein Harvesting Device. J Thorac Cardiovasc Surg. 2012 Nov;144(5):1256-7
- Ng CSH, Hui JWY, Wong RHL. Minimizing Single Port Access in VATS Wedge Resection by Hookwire. Asian Cardiovasc Thorac Annals 2013;21(1):114-115
- Ng CSH, Lau KKW, Gonzalez-Rivas D, Rocco G. Evolution in Surgical Approach & Techniques for Lung Cancer. Thorax 2013;68:681
- Ng CSH. Uniportal VATS in Asia. J Thorac Dis 2013;5(S3):S221-S225
- Ng CSH, Lau RWH, Wong RHL, Yim APC. Evolving Techniques of Endoscopic Thoracic Sympathectomy: Smaller Incisions or Less? The Surgeon 2013;11:290-291
- Ng CSH, Lau RWH, Wong RHL, Ho AMH, Wan S. Single Port Vasoview Ò Sympathectomy for Palmar Hyperhidrosis: A Clinical Update. Journal of Laparoendoscopic & Advanced Surgical Techniques 2014;24(1):32-4
- Ng CSH, Wong RHL, Lau RWH, Yim APC. Minimizing Chest Wall Trauma in Single Port Video-Assisted Thoracic Surgery. J Thorac Cardiovasc Surg 2014;147(3):1095-6
External links
 Media related to Video-assisted thoracoscopic surgery at Wikimedia Commons
Media related to Video-assisted thoracoscopic surgery at Wikimedia Commons