Tinea versicolor
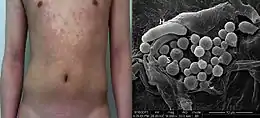
Tinea versicolor (also pityriasis versicolor) is a condition characterized by a skin eruption on the trunk and proximal extremities.[1] The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases.[2][3] These yeasts are normally found on the human skin and become troublesome only under certain circumstances, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.[2][4]
| Tinea versicolor | |
|---|---|
| Other names | Dermatomycosis furfuracea,[1] pityriasis versicolor,[1] tinea flava,[1] lota |
 | |
| Specialty | Dermatology |
| Causes | Malassezia globosa, Malassezia furfur |
The condition pityriasis versicolor was first identified in 1846.[5] Versicolor comes from the Latin versāre 'to turn' + color.[6] It is also commonly referred to as Peter Elam's disease in many parts of South Asia.[7]
Signs and symptoms

The symptoms of this condition include:
- Occasional fine scaling of the skin producing a very superficial ash-like scale
- Pale, dark tan, or pink in color, with a reddish undertone that can darken when the patient is overheated, such as in a hot shower or during/after exercise. Tanning typically makes the affected areas contrast more starkly with the surrounding skin.[9]
- Sharp border[10]
Pityriasis versicolor is more common in hot, humid climates or in those who sweat heavily, so it may recur each summer.[10]
The yeasts can often be seen under the microscope within the lesions and typically have a so-called "spaghetti and meatball appearance"[11] as the round yeasts produce filaments.
In people with dark skin tones, pigmentary changes such as hypopigmentation (loss of color) are common, while in those with lighter skin color, hyperpigmentation (increase in skin color) is more common. These discolorations have led to the term "sun fungus".[12]
Pathophysiology
In cases of tinea versicolor caused by the fungus Malassezia furfur, lightening of the skin occurs due to the fungus's production of azelaic acid, which has a slight bleaching effect.[13]
Diagnosis
.JPG.webp)
Tinea versicolor may be diagnosed by a potassium hydroxide (KOH) preparation and lesions may fluoresce copper-orange when exposed to Wood's lamp (UV-A light).[14] The differential diagnosis for tinea versicolor infection includes:
- Progressive macular hypomelanosis
- Pityriasis alba
- Pityriasis rosea
- Seborrheic dermatitis
- Erythrasma
- Vitiligo
- Leprosy
- Syphilis
- Post-inflammatory hypopigmentation
Treatment
Treatments for tinea versicolor include:
- Topical antifungal medications containing selenium sulfide are often recommended.[14] Ketoconazole (Nizoral ointment and shampoo) is another treatment. It is normally applied to dry skin and washed off after 20 minutes, repeated daily for two weeks. Ciclopirox (ciclopirox olamine) is an alternative treatment to ketoconazole, as it suppresses growth of the yeast Malassezia furfur. Initial results show similar efficacy to ketoconazole with a relative increase in subjective symptom relief due to its inherent anti-inflammatory properties.[15] Other topical antifungal agents such as clotrimazole, miconazole, terbinafine, or zinc pyrithione can lessen symptoms in some patients.[16] Additionally, hydrogen peroxide has been known to lessen symptoms and, on certain occasions, remove the problem, although permanent scarring has occurred with this treatment in some people. Clotrimazole is also used combined with selenium sulfide.
- Oral medications are viewed as a second-line of treatment for pityriasis versicolor in the event of widespread, severe, recalcitrant or recurrent cases. Systemic therapies include itraconazole (200 mg daily for seven days) and fluconazole (150 to 300 mg weekly dose for 2 to 4 weeks) that are preferred to oral ketoconazole which is no longer approved due to its potential hepatotoxic side effects.[17] The single-dose regimens and pulse therapy regimens can be made more effective by having the patient exercise 1–2 hours after the dose, to induce sweating. The sweat is allowed to evaporate, and showering is delayed for a day, leaving a film of the medication on the skin.[18]
Epidemiology
This skin disease commonly affects adolescents and young adults, especially in warm and humid climates. The yeast is thought to feed on skin oils (lipids), as well as dead skin cells. Infections are more common in people who have seborrheic dermatitis, dandruff, and hyperhidrosis.[4]
References
- Rapini, Ronald P; Bolognia, Jean L.; Jorizzo, Joseph L (2007). Dermatology: 2-Volume Set. St Louis: Mosby. pp. Chapter 76. ISBN 978-1-4160-2999-1.
- Morishita N; Sei Y. (December 2006). "Microreview of pityriasis versicolor and Malassezia species". Mycopathologia. 162 (6): 373–76. doi:10.1007/s11046-006-0081-2. PMID 17146580. S2CID 30397515.
- Prohic A; Ozegovic L. (January 2007). "Malassezia species isolated from lesional and non-lesional skin in patients with pityriasis versicolor". Mycoses. 50 (1): 58–63. doi:10.1111/j.1439-0507.2006.01310.x. PMID 17302750. S2CID 25493290.
- Weedon, D. (2002). Skin pathology (2nd ed.). Churchill Livingstone. ISBN 0-443-07069-5.
- Inamadar AC, Palit A (2003). "The genus Malassezia and human disease". Indian J Dermatol Venereol Leprol. 69 (4): 265–70. PMID 17642908.
- "versicolor". Collins English Dictionary — Complete & Unabridged 10th Edition. HarperCollins Publishers. Retrieved March 2, 2013.
- Kaushik A, Pinto HP, Bhat RM, Sukumar D, Srinath MK (2014). "A study of the prevalence and precipitating factors of pruritus in pityriasis versicolor". Indian Dermatology Online Journal. 5 (2): 223–224. doi:10.4103/2229-5178.131141. PMC 4030364. PMID 24860771.
- Ran Yuping (2016). "Observation of Fungi, Bacteria, and Parasites in Clinical Skin Samples Using Scanning Electron Microscopy". In Janecek, Milos; Kral, Robert (eds.). Modern Electron Microscopy in Physical and Life Sciences. InTech. doi:10.5772/61850. ISBN 978-953-51-2252-4. S2CID 53472683.
- "What to Avoid While Treating Tinea Versicolor". Archived from the original on 2013-07-27. Retrieved 2013-01-05.
- Pityriasis versicolor | DermNet New Zealand. Dermnetnz.org. Retrieved on 2016-10-14.
- "Adolescent Health Curriculum - Medical Problems - Dermatology - Papulosquamous Lesions (B4)". Archived from the original on 2008-11-28. Retrieved 2008-12-10.
- "Tioconazole (Topical Route) - MayoClinic.com". Retrieved 2008-12-10.
- Vary JC Jr (November 2015). "Selected Disorders of Skin Appendages-Acne, Alopecia, Hyperhidrosis". The Medical Clinics of North America. 99 (6): 1195–1211. doi:10.1016/j.mcna.2015.07.003. PMID 26476248.
- Likness, LP (June 2011). "Common dermatologic infections in athletes and return-to-play guidelines". The Journal of the American Osteopathic Association. 111 (6): 373–379. doi:10.7556/jaoa.2011.111.6.373. PMID 21771922.
- Ratnavel RC, Squire RA, Boorman GC (2007). "Clinical efficacies of shampoos containing ciclopirox olamine (1.5%) and ketoconazole (2.0%) in the treatment of seborrhoeic dermatitis". J Dermatolog Treat. 18 (2): 88–96. doi:10.1080/16537150601092944. PMID 17520465. S2CID 34852507.
- Faergemann, Jan (2000). "Management of Seborrheic Dermatitis and Pityriasis Versicolor". Am. J. Clin. Dermatol. 1 (2): 75–80. doi:10.2165/00128071-200001020-00001. PMID 11702314. S2CID 43516330.
- Karray, M; McKinney, WP (2021), "article-30211", Tinea Versicolor, Treasure Island (FL): StatPearls Publishing, PMID 29494106, retrieved 2021-08-07
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License. - Ketoconazole. Fpnotebook.com. Retrieved on 2016-10-14.
External links
 Media related to Tinea versicolor at Wikimedia Commons
Media related to Tinea versicolor at Wikimedia Commons