Alveolar lung disease
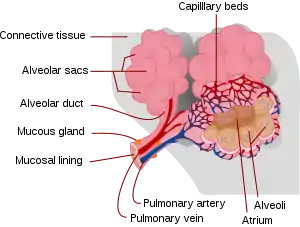
Alveolar lung diseases, are a group of diseases that mainly affect the alveoli of the lungs.[1]
| Alveolar lung disease | |
|---|---|
 | |
| Alveolus | |
| Specialty | Pulmonology |
Causes
Alveoli are the functional units of the lungs. Alveolar lung diseases are classified as processes that affect these units that ultimately lead to issues with ventilation. There are a number of different causes of insult to the alveoli including build up of fluid, hemorrhage, infection, malignancy and build up of protein and mineral deposits.
Conditions classified under alveolar lung disease include pulmonary edema (cardiogenic or non-cardiogenic), pneumonia (bacterial or viral), bronchoalveolar carcinoma, pulmonary hemorrhage, alveolar proteinosis and amyloidosis, and alveolar microlithiasis.
Alveolar lung disease may be divided into acute or chronic. Causes of acute alveolar lung disease include pulmonary edema (cardiogenic or neurogenic), pneumonia (bacterial or viral), systemic lupus erythematosus,[2] bleeding in the lungs (e.g., Goodpasture syndrome),[3] idiopathic pulmonary hemosiderosis,[4] and granulomatosis with polyangiitis.
Chronic alveolar lung disease can be caused by pulmonary alveolar proteinosis,[5] alveolar cell carcinoma, mineral oil pneumonia, sarcoidosis (alveolar form), lymphoma, tuberculosis, metastases, or desquamative interstitial pneumonia.
Diagnosis
Initial evaluation and Testing
Patients with alveolar lung disease may have difficulty breathing and/or a cough which may be productive of sputum or blood.
A physician will listen to the patient's lungs to help determine if there is likely a lower lung disease. Depending on the type of alveolar lung disease, the listener may hear "crackles" that indicate an excess of fluid in the lungs or an absence of lung sounds in certain regions which may indicate poor ventilation due to consolidation of pus or fibrosis.[6]
A pulse oximeter is a device that measures the amount of oxygen available in the blood. This is an important measurement in evaluation of a patient with difficulty breathing with suspected alveolar lung disease.
Imaging
Chest x-ray is the initial imaging modality of choice for evaluation of potential alveolar lung disease. Bedside ultrasound may also be utilized. The absence of radiographic evidence early on in the course of disease does not exclude alveolar disease.
Alveolar disease is visible on chest radiography as small, ill-defined nodules of homogeneous density centered on the acini or bronchioles. The nodules coalesce early in the course of disease, such that the nodules may only be seen as soft fluffy edges in the periphery.[1]
When the nodules are centered on the hilar regions, the chest x-ray may develop what is called the "butterfly," or "batwing" appearance. The nodules may also have a segmental or lobar distribution. Air alveolograms and air bronchograms can also be seen which indicate fluid in the alveoli with air in the terminal bronchioles indicating disease is alveolar.[1]
These findings appear soon after the onset of symptoms and change rapidly thereafter.
A segmental or lobar pattern may be apparent after aspiration pneumonia, atelectasis, lung contusion, localized pulmonary edema, obstructive pneumonia, pneumonia, pulmonary embolism with infarction, or tuberculosis.
Management
The two focuses of management for alveolar disease is supportive care to maintain oxygenation and ventilation to ensure that adequate oxygen is being delivered to blood, and to treat the underlying insult to the alveoli.
Supportive Care
Maintaining oxygenation and ventilation in alveolar lung disease is achieved through a number of methods. The mechanism of these treatments is primarily to provide oxygen and keep the alveoli open so that they can take up oxygen from and deliver it to the bloodstream. Ventilatory support is recognized as an essential component to treat pulmonary edema and acute respiratory distress syndrome.[7]
Non-invasive ventilation is the first step for patient's who require ventilatory support. This can take the form of oxygen delivered via nasal cannula or non-rebreather mask. Patients who require additional support may be given a high-flow nasal cannula which has an added function of providing positive pressure on the alveoli, can warm and humidify air and decrease required inspiratory effort of the patient.[8] BiPAP and CPAP can also be used as next level treatment. Finally, intubation with ventilator support can be used with positive pressure to improve ventilation and oxygenation.[9]
In cases where methods to support the lungs to provide oxygen to the blood fail, extracorporeal membrane oxygenation, or ECMO can be considered.
Treating underlying causes
Treating underlying causes of damage to alveoli is also essential in most alveolar lung disease.
Some more commonly seen instances of alveolar lung disease include pulmonary edema and pneumonia.
For pulmonary edema, medical treatment in addition to measures to maintain ventilation include diuretics to remove excess fluid from the lungs. Presumed bacterial pneumonia is typically treated with antibiotics.
References
- Al-Tubaikh, JA (2010). "Chapter 3.2 Alveolar lung diseases". Internal Medicine. Springer. p. 113. ISBN 978-3642037085.
- Amarnani, Raj; Yeoh, Su-Ann; Denneny, Emma K.; Wincup, Chris (2021-01-18). "Lupus and the Lungs: The Assessment and Management of Pulmonary Manifestations of Systemic Lupus Erythematosus". Frontiers in Medicine. 7: 610257. doi:10.3389/fmed.2020.610257. ISSN 2296-858X. PMC 7847931. PMID 33537331.
- Marques, C.; Plaisier, E.; Cacoub, P.; Cadranel, J.; Saadoun, D. (2020-01-01). "Mise au point sur la maladie des anticorps anti-membrane basale glomérulaire ou syndrome de Goodpasture". La Revue de Médecine Interne (in French). 41 (1): 14–20. doi:10.1016/j.revmed.2019.10.338. ISSN 0248-8663. PMID 31776042. S2CID 241253029.
- Saha, Biplab K. (2021-01-01). "Idiopathic pulmonary hemosiderosis: A state of the art review". Respiratory Medicine. 176: 106234. doi:10.1016/j.rmed.2020.106234. ISSN 0954-6111. PMID 33246295. S2CID 227191691.
- Jouneau, Stéphane; Ménard, Cédric; Lederlin, Mathieu (2020-05-03). "Pulmonary alveolar proteinosis". Respirology. 25 (8): 816–826. doi:10.1111/resp.13831. ISSN 1323-7799. PMID 32363736. S2CID 218492929.
- Reyes, Felix M.; Le, Jacqueline K. (2020), "Lung Exam", StatPearls, StatPearls Publishing, PMID 29083650, retrieved 2020-04-19
- Fan, Eddy; Brodie, Daniel; Slutsky, Arthur S. (2018-02-20). "Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment". JAMA. 319 (7): 698–710. doi:10.1001/jama.2017.21907. ISSN 0098-7484. PMID 29466596. S2CID 3451752.
- Lodeserto, Frank J.; Lettich, Thomas M.; Rezaie, Salim R. (2018-11-26). "High-flow Nasal Cannula: Mechanisms of Action and Adult and Pediatric Indications". Cureus. 10 (11): e3639. doi:10.7759/cureus.3639. ISSN 2168-8184. PMC 6358040. PMID 30740281.
- Bello, Giuseppe; De Santis, Paolo; Antonelli, Massimo (September 2018). "Non-invasive ventilation in cardiogenic pulmonary edema". Annals of Translational Medicine. 6 (18): 355. doi:10.21037/atm.2018.04.39. ISSN 2305-5839. PMC 6186545. PMID 30370282.