Biopsychosocial model
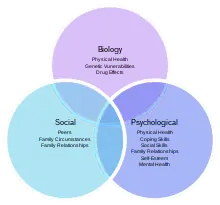
The biopsychosocial model is an inter-disciplinary model that looks at the interconnection between biology, psychology, and socio-environmental factors. The model specifically examines how these aspects play a role in topics ranging from health and disease, to human development. The model was first advocated by George L. Engel in 1977, and has become an alternative to the biomedical dominance of many health care systems.
History
The biopsychosocial model was first proposed by George L. Engel and Jon Romano of the University of Rochester in 1977.[1] As opposed to the biomedical approach, Engel strived for a more holistic approach by recognizing that each patient has their own thoughts, feelings, and history.[2] In developing the model, Engel framed this model for both illnesses and psychological problems.
The biopsychosocial model reflects the development of illness through the complex interaction of biological factors (genetic, biochemical, etc.), psychological factors (mood, personality, behaviour, etc.) and social factors (cultural, familial, socioeconomic, medical, etc.).[2][3] For example, a person may have a genetic predisposition for depression, but they must have social factors such as extreme stress at work and family life and psychological factors such as a perfectionistic tendencies which all trigger this genetic code for depression. A person may have a genetic predisposition for a disease, but social and cognitive factors must trigger the illness.
Specifically, Engel revolutionized medical thinking by re-proposing a separation of body and mind. The idea of mind–body dualism goes back at least to René Descartes, but was forgotten during the biomedical approach. Engel emphasized that the biomedical approach is flawed because the body alone does not contribute to illness.[4] Instead, the individual mind (psychological and social factors) plays a significant role in how an illness is caused and how it is treated. Engel proposes a dialogue between the patient and the doctor in order to find the most effective treatment solution.[5]
Similarly, materialistic and reductionist ideas proposed with the biomedical model are flawed because they cannot be verified on a cellular level (according to Engel).[6] Instead, the proposed model focuses on the research of past psychologists such as Urie Bronfenbrenner, popularized by his belief that social factors play a role in developing illnesses and behaviors. Simply, Engel used Bronfenbrenner's research as a column of his biopsychosocial model and framed this model to display health at the center of social, psychological, and biological aspects.
After publication, the biopsychosocial model was adopted by the World Health Organization in 2002 as a basis for the International Classification of Function (ICF).[7]
Current model
The biopsychosocial model is still widely used as a psychological model. The biological, psychological, and social categories have expanded into bigger categories: specifically, the social aspect has greatly expanded through ideas such as spirituality and culture. Even though many psychologists may not completely accept this model as their own, it is known for interconnecting three important categories.[8] Even if all aspects do not apply to the situation, the biopsychosocial model is widely used to organize one's thoughts. It shows that a person's problems are all connected, and they may be more complex than previously imagined.
Relevant theories and theorists
George L. Engel, who originally developed the biopsychosocial model, is often considered a primary theorist associated with the model. Engel used this model to offer an alternative to the more readily used biomedical model of the time. Engel felt the biopsychosocial model allows physicians to better understand their patients' subjective view of their illness and suffering.[8]
Potential applications
When Engel first proposed the biopsychosocial model it was for the purpose of better understanding health and illness. While this application still holds true the model is relevant to topics such as health, medicine, and development. Firstly, as proposed by Engel, it helps physicians better understand their whole patient. Considering not only physiological and medical aspects but also psychological and sociological well-being.[8] Furthermore, this model is closely tied to health psychology. Health psychology examines the reciprocal influences of biology, psychology, behavioral, and social factors on health and illness.
One application of the biopsychosocial model within health and medicine relates to pain, such that several factors outside an individual's health may affect their perception of pain. For example, a 2019 study linked genetic and biopsychosocial factors to increased post-operative shoulder pain.[9] Future studies are needed to model and further explore the relationship between biopsychosocial factors and pain.[10]
The developmental applications of this model are equally relevant. One particular advantage of applying the biopsychosocial model to developmental psychology is that it allows for an intersection within the nature versus nurture debate. This model provides developmental psychologists a theoretical basis for the interplay of both hereditary and psychosocial factors on an individuals' development.[8]
Criticisms and achievements
There have been a number of criticisms of the biopsychosocial model.[11][12][13] Benning summarized the arguments against the model including that it lacked philosophical coherence, was insensitive to patients' subjective experience, was unfaithful to the general systems theory that Engel claimed it be rooted in, and that it engendered an undisciplined eclecticism that provides no safeguards against either the dominance or the under-representation of any one of the three domains of bio, psycho, or social.[6]
Psychiatrist Hamid Tavakoli argues that the BPS model should be avoided because it unintentionally promotes an artificial distinction between biology and psychology, and merely causes confusion in psychiatric assessments and training programs, and that ultimately it has not helped the cause of trying to de-stigmatize mental health.[14] The perspectives model does not make that arbitrary distinction.[15]
A number of these criticisms have been addressed over recent years. For example, the BPS-Pathways model describes how it is possible to conceptually separate, define, and measure biological, psychological, and social factors, and thereby seek detailed interrelationships among these factors.[16]
References
- "The Biopsychosocial Model Approach" (PDF). Rochester University. Rochester University. Retrieved 18 April 2019.
- Engel, George L. (8 April 1977). "The need for a new medical model: a challenge for biomedicine" (PDF). Science. 196 (4286): 129–36. Bibcode:1977Sci...196..129E. doi:10.1126/science.847460. PMID 847460.
- Engel, George L. (1980). "The clinical application of the biopsychosocial model". American Journal of Psychiatry. 137 (5): 535–544. doi:10.1176/ajp.137.5.535. PMID 7369396.
- Dombeck, Mark. "The Bio-Psycho-Social Model". MentalHelp.Net. American Addiction Centers. Retrieved 18 April 2019.
- Gatchel, Robert J.; Haggard, Robbie (2014). "Biopsychosocial Prescreening for Spinal Cord and Peripheral Nerve Stimulation Devices". Practical Management of Pain. pp. 933–938.e2. doi:10.1016/B978-0-323-08340-9.00068-2. ISBN 978-0-323-08340-9.
- Lehman, Barbara J.; David, Diana M.; Gruber, Jennifer A. (August 2017). "Rethinking the biopsychosocial model of health: Understanding health as a dynamic system". Social and Personality Psychology Compass. 11 (8). e12328. doi:10.1111/spc3.12328.
- Hopwood, Val (2010). "Current context: neurological rehabilitation and neurological physiotherapy". Acupuncture in Neurological Conditions. Churchhill Livingstone. pp. 39–51. doi:10.1016/B978-0-7020-3020-8.00003-5. ISBN 978-0-7020-3020-8.
- Borrell-Carrió, Francesc; Suchman, Anthony; Epstein, Ronald (Nov 2004). "The Biopsychosocial Model 25 Years Later: Principles, Practice, and Scientific Inquiry". Annals of Family Medicine. 2 (6): 576–582. doi:10.1370/afm.245. PMC 1466742. PMID 15576544.
- Simon, Coreyb; Valencia, Carolina; Coronado, Rogelioa; et al. (Dec 2019). "Biopsychosocial Influences on Shoulder Pain: Analyzing the Temporal Ordering of Post-Operative Recovery". The Journal of Pain. 21 (7–8): 808–819. doi:10.1016/j.jpain.2019.11.008. PMC 7321871. PMID 31891763.
- Miaskowski, Christine; Blyth, Fiona; Nicosia, Francesca; Haan, Mary; Keefe, Frances; Smith, Alexander; Ritchie, Christine (1 September 2020). "A Biopsychosocial Model of Chronic Pain for Older Adults". Pain Medicine. 21 (9): 1793–1805. doi:10.1093/pm/pnz329. PMID 31846035.
- Benning, Tony (May 2015). "Limitations of the biopsychosocial model in psychiatry". Advances in Medical Education and Practice. 6: 347–352. doi:10.2147/AMEP.S82937. PMC 4427076. PMID 25999775.
- McLaren, N. (February 1998). "A Critical Review of the Biopsychosocial Model". Australian & New Zealand Journal of Psychiatry. 32 (1): 86–92. doi:10.3109/00048679809062712. PMID 9565189. S2CID 12321002.
- Ghaemi, S. Nassir (July 2009). "The rise and fall of the biopsychosocial model". British Journal of Psychiatry. 195 (1): 3–4. doi:10.1192/bjp.bp.109.063859. PMID 19567886.
- Tavakoli, HR (February 2009). "A closer evaluation of current methods in psychiatric assessments: a challenge for the biopsychosocial model". Psychiatry. 6 (2): 25–30. PMID 19724745.
- McHugh, Paul R. (1998). The perspectives of psychiatry (2nd ed.). Baltimore: Johns Hopkins University Press. ISBN 978-0801860461.
- Karunamuni N, Imayama I, Goonetilleke D. (2020). "Pathways to well-being: Untangling the causal relationships among biopsychosocial variables". Social Science & Medicine. 272: 112846. doi:10.1016/j.socscimed.2020.112846. PMID 32089388. S2CID 211262159.
{{cite journal}}: CS1 maint: multiple names: authors list (link)