Bipolar II disorder
Bipolar II disorder (BP-II) is a mood disorder on the bipolar spectrum, characterized by at least one episode of hypomania and at least one episode of major depression.[1][2][3][4] Diagnosis for BP-II requires that the individual must never have experienced a full manic episode.[5] Otherwise, one manic episode meets the criteria for bipolar I disorder (BP-I).[2]
| Bipolar II disorder | |
|---|---|
| Other names | BP-II, type two bipolar, bipolar type two |
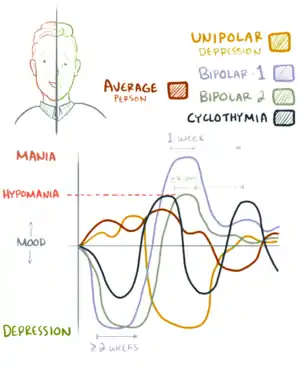 | |
| Graphical representation of Bipolar I, bipolar II and cyclothymia | |
| Specialty | Psychiatry |
| Treatment |
|
| Medication | |
Hypomania is a sustained state of elevated or irritable mood that is less severe than mania yet may still significantly affect the quality of life and result in permanent consequences including reckless spending, damaged relationships and poor judgment.[6]: 1651 Unlike mania, hypomania is not associated with psychosis.[1] The hypomanic episodes associated with BP-II must last for at least four days.[2][7]
Commonly, depressive episodes are more frequent and more intense than hypomanic episodes.[2] Additionally, when compared to BP-I, type II presents more frequent depressive episodes and shorter intervals of well-being.[1][2] The course of BP-II is more chronic and consists of more frequent cycling than the course of BP-I.[1][8] Finally, BP-II is associated with a greater risk of suicidal thoughts and behaviors than BP-I or unipolar depression.[1][8] Although BP-II is commonly perceived to be a milder form of type I, this is not the case. Types I and II present equally severe burdens.[1][9]
BP-II is notoriously difficult to diagnose. Patients usually seek help when they are in a depressed state, or when their hypomanic symptoms manifest themselves in unwanted effects, such as high levels of anxiety, or the seeming inability to focus on tasks. Because many of the symptoms of hypomania are often mistaken for high-functioning behavior or simply attributed to personality, patients are typically not aware of their hypomanic symptoms. In addition, many people with BP-II have periods of normal affect. As a result, when patients seek help, they are very often unable to provide their doctor with all the information needed for an accurate assessment; these individuals are often misdiagnosed with unipolar depression.[1][2][8] BP-II is more common than BP-I, while BP-II and major depressive disorder have about the same rate of diagnosis.[10] Of all individuals initially diagnosed with major depressive disorder, between 40% and 50% will later be diagnosed with either BP-I or BP-II.[1] Substance use disorders (which have high co-morbidity with BP-II) and periods of mixed depression may also make it more difficult to accurately identify BP-II.[2] Despite the difficulties, it is important that BP-II individuals be correctly assessed so that they can receive the proper treatment.[2] Antidepressant use, in the absence of mood stabilizers, is correlated with worsening BP-II symptoms.[1]
Causes
Multiple factors contribute to the development of bipolar spectrum disorders,[11] although there have been very few studies conducted to examine the possible causes of BP-II specifically.[12] While no identifiable single dysfunctions in specific neurotransmitters have been found, preliminary data has shown that calcium signal transmission, the glutamatergic system, and hormonal regulation play a role in the pathophysiology of the disease.[13] The cause of Bipolar disorder can be attributed to misfiring neurotransmitters that overstimulate the amygdala, which in turn causes the prefrontal cortex to stop working properly. The bipolar patient becomes overwhelmed with emotional stimulation with no way of understanding it, which can trigger mania and exacerbate the effects of depression.[14]
Signs and symptoms

Bipolar disorder is characterized by marked swings in mood, activity, and behavior.[15] BP-II is characterized by periods of hypomania, which may occur before, after, or independently of a depressive episode.[16]
Hypomania
Hypomania is the signature characteristic of BP-II, defined by an experience of elevated mood. A patient's mood is typically cheerful, enthusiastic, euphoric, or irritable.[16] In addition, they can present with symptoms of inflated self-esteem or grandiosity, decreased need for sleep, talkativeness or pressured speech, flight of ideas or rapid cycling of thoughts, distractibility, increased goal-directed activity, psychomotor agitation, and/or excessive involvement in activities that have a high potential for painful consequences (engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments.)[17]
Hypomania is distinct from mania. During a typical hypomanic episode, patients may present as upbeat, may show signs of poor judgment or display signs of increased energy despite lack of sleep, but do not meet the full criteria for an acute manic episode.[16] Patients may display elevated confidence, but do not express delusional thoughts as in mania. They can experience increase in goal-directed activity and creativity, but do not reach the severity of aimlessness and disorganization. Speech may be rapid, but interruptible. Patients with hypomania never present with psychotic symptoms and do not reach the severity to require psychiatric hospitalization.[18]
For these reasons, hypomania commonly goes unnoticed. Individuals often will only seek treatment during a depressive episode, and their history of hypomania may go undiagnosed. Although hypomania may increase functioning, episodes require treatment as they may indicate increasing instability and can precipitate a depressive episode.[1][2]
Depressive episodes
It is during depressive episodes that BP-II patients often seek help. Symptoms may be syndromal or subsyndromal.[1]
Depressive episodes in BP-II can present similarly to those experienced in unipolar depressive disorders.[19] Patients characteristically experience a depressed mood and may describe themselves as feeling sad, gloomy, down in the dumps, or hopeless, for most of the day, nearly every day. In children, this can present with an irritable mood. Most patients report significant fatigue, loss of energy, or tiredness. Patients or their family members may note diminished interest in usual activities such as sex, hobbies, or daily routines. Many patients report a change in appetite along with associated weight change. Sleep disturbances may be present, and can manifest as problems falling or staying asleep, frequent awakenings, excessive sleep, or difficulties getting up in the morning. Around half of depressed patients develop changes in psychomotor activity, described as slowness in thinking, speaking, or movement. Conversely, they may also present with agitation, with inability to sit still or wringing their hands. Changes in posture, speech, facial expression, and grooming can be observed. Other signs and symptoms include changes in posture and facial expression, slowed speech, poor hygiene, unkempt appearance, feelings of guilt, shame, or helplessness, diminished ability to concentrate, nihilistic thoughts, and suicidal ideation.[20][15]
Many experts in the field have attempted to find reliable differences between BP-I depressive episodes and episodes of major depressive disorder, but the data is inconsistent. However, some clinicians report that patients who came in with a depressive episode, but were later diagnosed as having bipolar disorder often presented with hypersomnia, increased appetite, psychomotor retardation, and a history of antidepressant-induced hypomania.[19][8] Evidence also suggests that BP-II is strongly associated with atypical depression.[1]
Mood episodes with mixed features
A mixed episode is defined by the presence of a hypomanic or depressive episode that is accompanied by symptoms of the opposite polarity. This is commonly referred to as a mood episode with mixed features (e.g. depression with mixed features or hypomania with mixed features), but can also be referred to as mixed episodes or mixed states.[21] For example, a patient with depression with mixed features may have a depressed mood, but has simultaneous symptoms of rapid speech, increased energy, and flight of ideas. Conversely, a patient with hypomania with mixed features will present with the full criteria for a hypomanic episode, but with concurrent symptoms of decreased appetite, loss of interest, and low energy.[22]
Episodes with mixed features can last up to several months. They occur more frequently in patients with an earlier onset of bipolar disorder, are associated with higher frequency of episodes, and are associated with a greater risk of substance use, anxiety disorders, and suicidality. In addition, they are associated with increased treatment resistance compared to non-mixed episodes.[21]
Relapse
Bipolar disorder is often a lifelong condition, and patients should be followed up regularly for relapse prevention.[23] Although BP-II is thought to be less severe than BP-I in regard to symptom intensity, BP-II is associated with higher frequencies of rapid cycling and depressive episodes.[24] In the case of a relapse, patients may experience new onset sleep disturbance, racing thoughts and/or speech, anxiety, irritability, and increase in emotional intensity. Family and/or friends may notice that patients are arguing more frequently with them, spending more money than usual, are increasing their binging on food, drugs, or alcohol, and may suddenly start taking on many projects at once. These symptoms often occur and are considered early warning signs.[25]
Psychosocial factors in a person's life can trigger a relapse in patients with BP-II. These include stressful life events, criticism from peers or relatives, and a disrupted circadian rhythm. In addition, the addition of antidepressant medications can trigger a hypomanic episode.[26]
Comorbid conditions
Comorbid conditions are extremely common in individuals with BP-II. In fact, individuals are twice as likely to present a comorbid disorder than not.[2] These include anxiety, eating, personality (cluster B), and substance use disorders.[2][8] For BP-II, the most conservative estimate of lifetime prevalence of alcohol or other substance use disorders is 20%. In patients with comorbid substance use disorder and BP-II, episodes have a longer duration and treatment compliance decreases. Preliminary studies suggest that comorbid substance use is also linked to increased risk of suicidality.[27]
Diagnosis

BP-II is diagnosed according to the criteria established in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).[17] In addition, alternative diagnostic criteria is established in the World Health Organization's International Classification of Diseases-10th Revision (ICD-10).[28] The diagnostic criteria are established from self-reported experiences from patients or their family members, the psychiatric assessment, and the mental status examination. In addition, Screening instruments like the Mood Disorders Questionnaire are helpful tools in determining a patient's status on the bipolar spectrum. In addition, certain features have been shown to increase the chances that depressed patients have a bipolar disorder, including atypical symptoms of depression like hypersomnia and hyperphagia, a family history of bipolar disorder, medication-induced hypomania, recurrent or psychotic depression, antidepressant refractory depression, and early or postpartum depression.[29]
DSM-5 criteria
According to the DSM-5, a patient diagnosed with BP-II will have experienced at least one hypomanic episode, at least one major depressive episodes, and no manic episode. Furthermore, the occurrence of the mood episodes are not better explained by schizoaffective disorder, schizophrenia, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorder. The final criteria that must be met is that the mood episodes cause clinically significant distress or impairment in social, occupational, or other important areas of functioning (from the depressive symptoms or the unpredictability of cycling between periods of depression and hypomania).[5]
A hypomanic episode is established if a patient's symptoms last for most of the day each day for at least four days. Furthermore, three or more of the following symptoms must be present: Inflated sense of self-esteem or grandiose thoughts, feeling well rested despite getting low amounts of sleep (3 hours), talkativeness, racing thoughts, distractibility, and increase in goal-directed activity or psychomotor agitation, or excessive involvement in activities with high risk of painful consequences. Per DSM-5 criteria, a major depressive episode consists of the presence of a depressed mood or loss of interest/pleasure in activities (anhedonia). In addition to the former symptoms, five out of the nine following symptoms must occur for more than two weeks (to the extent in which it impairs functioning): weight loss/gain, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue, feelings of worthlessness/inappropriate guilt, decreased concentration, or thoughts of death/suicide.[5]
Specifiers:
- With current or most recent episode hypomanic or depressed
- With partial remission or full remission
- With mild, moderate, or severe severity
- With anxious distress
- With catatonic features
- With mood congruent psychotic features
- With peripartum onset
- With seasonal pattern (applies only to the pattern of major depressive episodes)
- With rapid cycling.
ICD-11
According to the ICD-11, a BP-II patient will have experienced episodic experiences of one or more hypomaniac episodes and one or more major depressive episodes, and no history of a manic episode or mixed episode.[30] These symptoms cannot be explained by other diagnoses such as
- Cyclothymia[30]
- ADHD[30]
- Oppositional Defiant Disorder[30]
- Schizophrenia and other primary psychotic disorders[30]
- Substance-Use Disorder[30]
- Personality Disorders[30]
- Other Mental illness[30]
- Physical issues such as a brain tumor[30]
The specifiers are the same as the DSM-5 with the exception of catatonic features and if symptoms have occurred with or without psychosis about 6 weeks after childbirth[30]
Differential diagnoses
The signs and symptoms of BP-II may overlap significantly with those of other conditions. Thus, a comprehensive history, medication review, and laboratory work are key to diagnosing BP-II and differentiating it from other conditions. The differential diagnosis of BP-II is as follows: unipolar major depression, borderline personality disorder, posttraumatic stress disorder, substance use disorders, and attention deficit hyperactivity disorder.[6]: 1653–7 In clinical practice, the difficulty of diagnosing BP-II depends on the accurate detection of hypomania, which is frequently dismissed by patients. Patients can present with increased productivity and energy with the absence of signs of instability or disturbance. As such, there is a risk that BP-II is misdiagnosed as generalized anxiety disorder or unipolar major depression. An accurate evaluation of differential diagnoses are crucial, as they guide treatment and prognostic implications.
Major differences between BP-I and BP-II have been identified in their clinical features, comorbidity rates and family histories. During depressive episodes, BP-II patients tend to show higher rates of psychomotor agitation, guilt, shame, suicidal ideation, and suicide attempts. BP-II patients have shown higher lifetime comorbidity rates of phobias, anxiety disorders, substance use, and eating disorders. In addition, there is a higher correlation between BP-II patients and family history of psychiatric illness, including major depression and substance-related disorders compared to BP-I.[24] The occurrence rate of psychiatric illness in first degree relatives of BP-II patients was 26.5%, versus 15.4% in BP-I patients.[24][29]
Management
Although BP-II is a prevalent condition associated with morbidity and mortality, there has been an absence of robust clinical trials and systematic reviews that investigate the efficacy of pharmacologic treatments for the hypomanic and depressive phases of BP-II. Thus, the current treatment guidelines for the symptoms of BP-II are derived and extrapolated from the treatment guidelines in BP-I, along with limited randomized controlled trials published in the literature.[31][6]: 1697
The treatment of BP-II consists of the following: treatment of hypomania, treatment of major depression, and maintenance therapy for the prevention of relapse of hypomania or depression. As BP-II is a chronic condition, the goal of treatment is to achieve remission of symptoms and prevention of self-harm in patients.[1] Treatment modalities of BP-II include medication-based pharmacotherapy, along with various forms of psychotherapy.[32]
Medications

The most common pharmacologic agents utilized in the treatment of BP-II includes mood stabilizers, antipsychotics, and antidepressants.[1]
Mood stabilizers
Mood stabilizers used in the treatment of hypomanic and depressive episodes of BP-II include lithium, and the anticonvulsant medications valproate, carbamazepine, lamotrigine, and topiramate.[23]
There is strong evidence that lithium is effective in treating both the depressive and hypomanic symptoms in BP-II, along with the reduction of hypomanic switch in patients treated with antidepressants. Furthermore, lithium is the only mood stabilizer to demonstrate a decrease in suicide and self-harm in patients with mood disorders.[33] Due to lithium's narrow therapeutic index, lithium levels must be monitored regularly for prevention of lithium toxicity.
There is also evidence that the anticonvulsants valproate, lamotrigine, carbamazepine, and topiramate are effective in the reduction of symptoms of hypomanic and depressive episodes of bipolar disorder. Potential mechanisms contributing to these effects include a decrease in brain excitation due to blockage of low-voltage sodium-gated channels, decrease in glutamate and excitatory amino acids, and potentiation of levels of GABA.[34] There is evidence that lamotrigine decreases the risk of relapse in rapid-cycling BP-II. It is more effective in BP-II than BP-I, suggesting that lamotrigine is more effective for the treatment of depressive rather than manic episodes. Doses ranging from 100 to 200 mg have been reported to have the most efficacy, while experimental doses of 400 mg have rendered little response.[35] A large, multicenter trial comparing carbamazepine and lithium over two and a half years found that carbamazepine was superior in terms of preventing future episodes of BP-II, although lithium was superior in individuals with BP-I. There is also some evidence for the use of valproate and topiramate, although the results for the use of gabapentin have been disappointing.
Antipsychotics

Antipsychotics are utilized as a second line option for hypomanic episodes, typically indicated patients who do not respond to mood stabilizers.[36] However, quetiapine is the only antipsychotic that has demonstrated efficacy in multiple meta-analyses of Randomized controlled trials for treating acute BP-II depression, and is a first-line option for patients with BP-II depression.[6]: 1697 [37] Other antipsychotics that are used to treat BP-II include lurasidone, olanzapine, cariprazine, aripiprazole, asenapine, paliperidone, risperidone, ziprasidone, haloperidol, and chlorpromazine. As a class, the first generation antipsychotics are associated with movement disorders, along with anticholinergic side effects compared with second generation antipsychotics.[36]
Antidepressants
There is evidence to support the use of SSRI and SNRI antidepressants in BP-II, but the use of these treatments are controversial.[38] Potential risks of antidepressant pharmacotherapy in patients with bipolar disorder include increased mood cycling, development of rapid cycling, dysphoria, and switch to hypomania.[39] In addition, the evidence for their efficacy in bipolar depression is mixed. Thus, in most cases, antidepressant monotherapy in patients with BP-II is not recommended. However, antidepressants may provide benefit some patients when used in addition to mood stabilizers and antipsychotics, as these drugs reduce the risk of manic/hypomanic switching.[36] However, the risk still exists, and should be used with caution.[31]
Non-pharmaceutical therapies
Although medication therapy is the standard of care for treatment of both BP-I and BP-II, additional non-pharmaceutical therapies can also help those with the illness. Benefits include prevention of relapse and improved maintenance medication adherence. These include psychotherapy (e.g. cognitive behavioral therapy, psychodynamic therapy, psychoanalysis, interpersonal therapy, behavioral therapy, cognitive therapy, and family-focused therapy), social rhythm therapy, art therapy, music therapy, psychoeducation, mindfulness, and light therapy. Meta-analyses in the literature has shown that psychotherapy plus pharmacotherapy was associated with a lower relapse rate compared with patients treated with pharmacotherapy alone.[40] However, relapse can still occur, despite continued medication and therapy.[41] People with bipolar disorder may develop dissociation to match each mood they experience. For some, this is done intentionally, as a means by which to escape trauma or pain from a depressive period, or simply to better organize one's life by setting boundaries for one's perceptions and behaviors.[42]
Prognosis
There is evidence to suggest that BP-II has a more chronic course of illness than BP-I.[43] This constant and pervasive course of the illness leads to an increased risk in suicide and more hypomanic and major depressive episodes with shorter periods between episodes than BP-I patients experience.[43] The natural course of BP-II, when left untreated, leads to patients spending the majority of their lives with some symptoms, primarily stemming from depression.[29] Their recurrent depression results in personal distress and disability.[29]
This disability can present itself in the form of psychosocial impairment, which has been suggested to be worse in BP-II patients than in BP-I patients.[44] Another facet of this illness that is associated with a poorer prognosis is rapid cycling, which denotes the occurrence of four or more major Depressive, Hypomanic, and/or mixed episodes in a 12-month period.[43] Rapid cycling is quite common in those with BP-II, much more so in women than in men (70% vs. 40%), and without treatment leads to added sources of disability and an increased risk of suicide.[29] Women are more prone to rapid cycling between hypomanic episodes and depressive episodes.[45] To improve a patient's prognosis, long-term therapy is most favorably recommended for controlling symptoms, maintaining remission and preventing relapses.[46] With treatment, patients have been shown to present a decreased risk of suicide (especially when treated with lithium) and a reduction of frequency and severity of their episodes, which in turn moves them toward a stable life and reduces the time they spend ill.[47] To maintain their state of balance, therapy is often continued indefinitely, as around 50% of the patients who discontinue it relapse quickly and experience either full-blown episodes or sub-syndromal symptoms that bring significant functional impairments.[46]
Functioning
The deficits in functioning associated with BP-II stem mostly from the recurrent depression that BP-II patients experience. Depressive symptoms are much more disabling than hypomanic symptoms and are potentially as, or more disabling than mania symptoms.[44] Functional impairment has been shown to be directly linked with increasing percentages of depressive symptoms, and because sub-syndromal symptoms are more common—and frequent—in BP-II, they have been implicated heavily as a major cause of psychosocial disability.[29] There is evidence that shows the mild depressive symptoms, or even sub-syndromal symptoms, are responsible for the non-recovery of social functioning, which furthers the idea that residual depressive symptoms are detrimental for functional recovery in patients being treated for BP-II.[48] It has been suggested that symptom interference in relation to social and interpersonal relationships in BP-II is worse than symptom interference in other chronic medical illnesses such as cancer.[48] This social impairment can last for years, even after treatment that has resulted in a resolution of mood symptoms.[48]
The factors related to this persistent social impairment are residual depressive symptoms, limited illness insight (a very common occurrence in patients with BP-II), and impaired executive functioning.[48] Impaired ability in executive functions is directly tied to poor psychosocial functioning, a common side-effect in patients with BP-II.[49]
The impact on a patient's psychosocial functioning stems from the depressive symptoms (more common in BP-II than BP-I).[44] An increase in these symptoms' severity seems to correlate with a significant increase in psychosocial disability.[49] Psychosocial disability can present itself in poor semantic memory, which in turn affects other cognitive domains like verbal memory and (as mentioned earlier) executive functioning leading to a direct and persisting impact on psychosocial functioning.[50]
An abnormal semantic memory organization can manipulate thoughts and lead to the formation of delusions and possibly affect speech and communication problems, which can lead to interpersonal issues.[50] BP-II patients have also been shown to present worse cognitive functioning than those patients with BP-I, though they demonstrate about the same disability when it comes to occupational functioning, interpersonal relationships, and autonomy.[49] This disruption in cognitive functioning takes a toll on their ability to function in the workplace, which leads to high rates of work loss in BP-II patient populations.[44] After treatment and while in remission, BP-II patients tend to report a good psychosocial functioning but they still score less than patients without the disorder.[29] These lasting impacts further suggest that a prolonged period of untreated BP-II can lead to permanent adverse effects on functioning.[48]
Recovery and recurrence
BP-II has a chronic relapsing nature.[46] It has been suggested that BP-II patients have a higher degree of relapse than BP-I patients.[43] Generally, within four years of an episode, around 60% of patients will relapse into another episode.[46] Some patients are symptomatic half the time, either with full on episodes or symptoms that fall just below the threshold of an episode.[46]
Because of the nature of the illness, long-term therapy is the best option and aims to not only control the symptoms but to maintain sustained remission and prevent relapses from occurring.[46] Even with treatment, patients do not always regain full functioning, especially in the social realm.[48] There is a very clear gap between symptomatic recovery and full functional recovery for both BP-I and BP-II patients.[49] As such, and because those with BP-II spend more time with depressive symptoms that do not quite qualify as a major depressive episode, the best chance for recovery is to have therapeutic interventions that focus on the residual depressive symptoms and to aim for improvement in psychosocial and cognitive functioning.[49] Even with treatment, a certain amount of responsibility is placed in the patient's hands; they have to be able to assume responsibility for their illness by accepting their diagnosis, taking the required medication, and seeking help when needed to do well in the future.[25]
Treatment often lasts after remission is achieved, and the treatment that worked is continued during the continuation phase (lasting anywhere from 6–12 months) and maintenance can last 1–2 years or, in some cases, indefinitely.[51] One of the treatments of choice is Lithium, which has been shown to be very beneficial in reducing the frequency and severity of depressive episodes.[47] Lithium prevents mood relapse and works especially well in BP-II patients who experience rapid-cycling.[47] Almost all BP-II patients who take lithium have a decrease in the amount of time they spend ill and a decrease in mood episodes.[47]
Along with medication, other forms of therapy have been shown to be beneficial for BP-II patients. A treatment called a "well-being plan" serves several purposes: it informs the patients, protects them from future episodes, teaches them to add value to their life, and works toward building a strong sense of self to fend off depression and reduce the desire to succumb to the seductive hypomanic highs.[25] The plan has to aim high. Otherwise, patients will relapse into depression.[25] A large part of this plan involves the patient being very aware of warning signs and stress triggers so that they take an active role in their recovery and prevention of relapse.[25]
Mortality
Several studies have shown that the risk of suicide is higher in patients who have BP-II than those with BP-I, and especially higher than patients with major depressive disorder.[29]
In results of a summary of several lifetime study experiments, it was found that 24% of BP-II patients experienced suicidal ideation or suicide attempts compared to 17% in BP-I patients and 12% in major depressive patients.[29][52] Bipolar disorders, in general, are the third leading cause of death in 15- to 24-year-olds.[53] BP-II patients were also found to employ more lethal means and have more complete suicides overall.[29]
BP-II patients have several risk factors that increase their risk of suicide. The illness is very recurrent and results in severe disabilities, interpersonal relationship problems, barriers to academic, financial, and vocational goals, and a loss of social standing in their community, all of which increase the likelihood of suicide.[54] Mixed symptoms and rapid-cycling, both very common in BP-II, are also associated with an increased risk of suicide.[29] The tendency for BP-II to be misdiagnosed and treated ineffectively, or not at all in some cases, leads to an increased risk.[52]
As a result of the high suicide risk for this group, reducing the risk and preventing attempts remains a main part of the treatment; a combination of self-monitoring, close supervision by a therapist, and faithful adherence to their medication regimen will help to reduce the risk and prevent the likelihood of suicide.[54]
Suicide is a common endpoint for many patients with severe psychiatric illness. The mood disorders (depression and bipolar) are by far the most common psychiatric conditions associated with suicide. At least 25% to 50% of patients with bipolar disorder also attempt suicide at least once. Aside from lithium—which is the most demonstrably effective treatment against suicide—little is known about contributions of specific mood-altering treatments to minimizing mortality rates in persons with either major mood disorders or bipolar depression specifically. Suicide is usually a manifestation of severe psychiatric distress that is often associated with a diagnosable and treatable form of depression or other mental illness. In a clinical setting, an assessment of suicidal risk must precede any attempt to treat psychiatric illness.[55]
Epidemiology
The global estimated lifetime prevalence of bipolar disorder among adults range from 1 to 3 percent.[56] The annual incidence is estimated to vary from 0.3 to 1.2 percent worldwide.[19] According to the World Mental Health Survey Initiative, the lifetime prevalence of BP-II was found to be 0.4%, with a 12-month prevalence of 0.3%.[57] Other meta-analyses have found lifetime prevalence of BP-II up to 1.57%.[58] In the United States, the estimated lifetime prevalence of BP-II was found to be 1.1%, with a 12-month prevalence of 0.8%.[57] The mean age of onset for BP-II was 20 years. Thus far, there have been no studies that have conclusively demonstrated that an unequal distribution of bipolar disorders across sex and ethnicity exists.[59]
It must be noted that a vast majority of studies and meta-analysis do not differentiate between BP-I and BP-II, and current epidemiology data may not accurately describe true prevalence and incidence.[60] In addition, BP-II is underdiagnosed in practice, and it is easy to miss milder forms of the condition.[57]
History
In 19th century psychiatry, mania covered a broad range of intensity, and hypomania was equated by some to concepts of 'partial insanity' or monomania. A more specific usage was advanced by the German neuro-psychiatrist Emanuel Ernst Mendel in 1881, who wrote "I recommend (taking under consideration the word used by Hippocrates) to name those types of mania that show a less severe phenomenological picture, 'hypomania'".[61] Narrower operational definitions of hypomania were developed from the 1960s/1970s.
The first diagnostic distinction to be made between manic-depression involving mania and involving hypomania came from Carl Gustav Jung in 1903.[62][63] In his paper, Jung introduced the non-psychotic version of the illness with the statement, "I would like to publish a number of cases whose peculiarity consists in chronic hypomanic behavior" where "it is not a question of real mania at all but of a hypomanic state which cannot be regarded as psychotic."[62][63] Jung illustrated the hypomanic variation with five case histories, each involving hypomanic behavior, occasional bouts of depression, and mixed mood states, which involved personal and interpersonal upheaval for each patient.[62]
In 1975, Jung's original distinction between mania and hypomania gained support. Fieve and Dunner published an article recognizing that only individuals in a manic state require hospitalization. It was proposed that the presentation of either the one state or the other differentiates two distinct diseases; the proposition was initially met with skepticism. However, studies since confirm that BP-II is a phenomenologically distinct disorder.[8]
Empirical evidence, combined with treatment considerations, led the DSM-IV Mood Disorders Work Group to add BP-II as its own entity in the 1994 publication. Only one other mood disorder was added to this edition, indicating the conservative nature of the DSM-IV work group. In May 2013, the DSM-5 was released. Two revisions to the existing BP-II criteria are anticipated. The first expected change will reduce the required duration of a hypomanic state from four to two days. The second change will allow hypomania to be diagnosed without the manifestation of elevated mood; that is, increased energy/activity will be sufficient. The rationale behind the latter revision is that some individuals with BP-II manifest only visible changes in energy. Without presenting elevated mood, these individuals are commonly misdiagnosed with major depressive disorder. Consequently, they receive prescriptions for antidepressants, which unaccompanied by mood stabilizers, may induce rapid cycling or mixed states.[64]
Society and culture
- Heath Black revealed in his autobiography, Black, that he has been diagnosed with BP-II.[65]
- Maria Bamford has been diagnosed with BP-II.[66]
- Geoff Bullock, singer-songwriter, was diagnosed with BP-II.[67]
- Mariah Carey was diagnosed with BP-II in 2001. In 2018, publicly revealed and actively seeking treatment in the form of therapy and medication.[68]
- Charmaine Dragun, former Australian journalist/newsreader. Inquest concluded she had BP-II.[69]
- Joe Gilgun has been diagnosed with BP-II.[70]
- Shane Hmiel has been diagnosed with BP-II.[71]
- Jesse Jackson Jr. has been diagnosed with BP-II.[72]
- Thomas Eagleton received a diagnosis of BP-II from Dr. Frederick K. Goodwin.[73]
- Carrie Fisher had been diagnosed with BP-II.[74]
- Demi Lovato has been diagnosed with BP-II.[75][76]
- Evan Perry, subject of the documentary Boy Interrupted, was diagnosed with BP-II.[77]
- Richard Rossi, filmmaker, musician, and maverick minister was diagnosed with BP-II.[78]
- Rumer has been diagnosed with BP-II.[79]
- Catherine Zeta-Jones received treatment for BP-II after dealing with the stress of her husband's throat cancer. According to her publicist, Zeta-Jones made a decision to check into a mental health facility for a brief stay.[80]
See also
References
- Benazzi F (2007). "Bipolar II disorder: Epidemiology, Diagnosis and Management". CNS Drugs (Therapy in Practice). 21 (9): 727–40. doi:10.2165/00023210-200721090-00003. PMID 17696573. S2CID 28078494.
- Berk M, Dodd S (February 2005). "Bipolar II disorder: a review". Bipolar Disorders. 7 (1): 11–21. doi:10.1111/j.1399-5618.2004.00152.x. PMID 15654928.
- Hurley K (24 November 2020). "Bipolar Disorder and Depression: Understanding the Difference". Psycom. Archived from the original on 2018-09-07. Retrieved 29 January 2021.
- "Bipolar Diagnosis". WebMD. Atlanta, Georgia. 29 January 2021. p. 1. Archived from the original on 2007-03-03. Retrieved 30 January 2021.
- American Psychiatric Association. American Psychiatric Association. DSM-5 Task Force. (2017) [2013]. Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). Washington, D.C.: American Psychiatric Association. p. 139. ISBN 9780890425541. OCLC 1042815534 – via Internet Archive.
- Sadock, Benjamin J.; Sadock, Virginia A.; Ruiz, Pedro (2017). Kaplan & Sadock's comprehensive textbook of psychiatry (10th ed.). Philadelphia: Wolters Kluwer. ISBN 978-1-4963-8915-2. OCLC 988106757.
- Buskist W, Davis SF, eds. (2008). 21st Century Psychology: A Reference Handbook. Thousand Oaks, California: Sage Publications. pp. 290. ISBN 978-1-4129-4968-2 – via Internet Archive.
- Mak AD (2007). "A short review on the diagnostic issues of bipolar spectrum disorders in clinically depressed patients -- Bipolar II disorder". Hong Kong Journal of Psychiatry. 17: 139–144 – via Gale.
- Merikangas KR, Lamers F (January 2012). "The 'true' prevalence of bipolar II disorder". Current Opinion in Psychiatry. 25 (1): 19–23. doi:10.1097/YCO.0b013e32834de3de. PMID 22156934. S2CID 10768397.
- Benazzi, Franco (March 2004). "How to treat bipolar II depression and bipolar II mixed depression?". The International Journal of Neuropsychopharmacology. 7 (1): 105–106. doi:10.1017/S146114570300395X. ISSN 1461-1457. PMID 14731315.
- The National Institute of Mental Health (January 2020). "Bipolar Disorder". National Institute of Mental Health. Risk Factors. Archived from the original on 2007-09-20. Retrieved 31 January 2021.
- Leahy RL (2007). "Bipolar disorder: Causes, contexts, and treatments". Journal of Clinical Psychology. 63 (5): 417–424. doi:10.1002/jclp.20360. ISSN 0021-9762. PMID 17417809.
- Almeida, Hugo Sérgio; Mitjans, Marina; Arias, Barbara; Vieta, Eduard; Ríos, José; Benabarre, Antonio (November 2020). "Genetic differences between bipolar disorder subtypes: A systematic review focused in bipolar disorder type II". Neuroscience and Biobehavioral Reviews. 118: 623–630. doi:10.1016/j.neubiorev.2020.07.033. ISSN 1873-7528. PMID 32755611. S2CID 220923413.
- Carter J (2009). The complete idiot's guide to bipolar disorder. Bobbi Dempsey. New York: Alpha. pp. 63–65. ISBN 9781592578177. OCLC 213308949 – via Google Books.
- Black DW, Andreasen NC (2014). Introductory textbook of psychiatry (Sixth ed.). Washington, DC. pp. 156–157. ISBN 978-1-58562-469-0. OCLC 865641999.
- Black DW, Andreasen NC (2014). Introductory textbook of psychiatry (Sixth ed.). Washington, DC. pp. 157–161. ISBN 978-1-58562-469-0. OCLC 865641999.
- "American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)", SpringerReference, Berlin/Heidelberg: Springer-Verlag, 2011, doi:10.1007/springerreference_179660, retrieved 2022-01-27
- Benazzi, Franco (March 2007). "Bipolar disorder—focus on bipolar II disorder and mixed depression". The Lancet. 369 (9565): 935–945. doi:10.1016/s0140-6736(07)60453-x. ISSN 0140-6736. PMID 17368155. S2CID 10704613.
- Boland, Robert; Verduin, Marcia; Ruiz, Pedro; Sadock, Benjamin (2022). Kaplan & Sadock's synopsis of psychiatry (12 ed.). Philadelphia. p. 366. ISBN 978-1-9751-4556-9. OCLC 1227837243.
- Ebert, Michael; Leckman, James; Petrakis, Ismene (2019). Current diagnosis & treatment. Psychiatry (3 ed.). New York. ISBN 978-0-07-177194-8. OCLC 1057895724.
- Betzler, Felix; Stöver, Laura Apollonia; Sterzer, Philipp; Köhler, Stephan (2017-04-18). "Mixed states in bipolar disorder – changes in DSM-5 and current treatment recommendations". International Journal of Psychiatry in Clinical Practice. 21 (4): 244–258. doi:10.1080/13651501.2017.1311921. ISSN 1365-1501. PMID 28417647. S2CID 19068715.
- Wright, Padraig; Stern, Julia; Phelan, Michael (2012). Core psychiatry. Elsevier. pp. 501–510. ISBN 978-0-7020-3397-1. OCLC 712765641.
- Black DW, Andreasen NC (2014). Introductory textbook of psychiatry (6 ed.). Washington, DC. pp. 184–186. ISBN 978-1-58562-469-0. OCLC 865641999.
- Baek JH, Park DY, Choi J, Kim JS, Choi JS, Ha K, Kwon JS, Lee D, Hong KS (June 2011). "Differences between bipolar I and bipolar II disorders in clinical features, comorbidity, and family history". Journal of Affective Disorders. 131 (1–3): 59–67. doi:10.1016/j.jad.2010.11.020. ISSN 1573-2517. PMID 21195482.
- Orum M (2008). "The Role of Wellbeing Plans in Managing Bipolar II Disorder". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Eyers K (collaborator). Cambridge, England: Cambridge University Press. pp. 151–165. ISBN 978-0-521-87314-7.
- Proudfoot J, Doran J, Manicavasagar V, Parker G (October 2011). "The precipitants of manic/hypomanic episodes in the context of bipolar disorder: a review". Journal of Affective Disorders. 133 (3): 381–7. doi:10.1016/j.jad.2010.10.051. PMID 21106249.
- Cerullo MA, Strakowski SM (October 2007). "The prevalence and significance of substance use disorders in bipolar type I and II disorder". Substance Abuse Treatment, Prevention, and Policy. 2: 29. doi:10.1186/1747-597X-2-29. PMC 2094705. PMID 17908301.
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization. 1992. ISBN 92-4-154422-8. OCLC 28294867.
- Hadjipavlou G, Yatham LN (2008). "Bipolar II Disorder in Context: epidemiology, disability, and economic burden". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Cambridge, England: Cambridge University Press. pp. 61–74. ISBN 978-0-521-87314-7.
- "ICD-11 for Mortality and Morbidity Statistics". icd.who.int. p. Section 6A61. Subtypes listed. Retrieved 2022-05-03.
- El-Mallakh R, Weisler RH, Townsend MH, Ginsberg LD (2006). "Bipolar II disorder: current and future treatment options". Annals of Clinical Psychiatry. 18 (4): 259–66. doi:10.1080/10401230600948480. PMID 17162626.
- Novick, Danielle M.; Swartz, Holly A. (June 2019). "Psychosocial Interventions for Bipolar II Disorder". American Journal of Psychotherapy. 72 (2): 47–57. doi:10.1176/appi.psychotherapy.20190008. ISSN 0002-9564. PMID 31070452. S2CID 148569714.
- Cipriani, A.; Hawton, K.; Stockton, S.; Geddes, J. R. (2013-06-27). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ. 346 (jun27 4): f3646. doi:10.1136/bmj.f3646. ISSN 1756-1833. PMID 23814104. S2CID 25843596.
- "Guideline Watch: Practice Guideline for the Treatment of Patients With Bipolar Disorder, 2nd Edition", APA Practice Guidelines for the Treatment of Psychiatric Disorders: Comprehensive Guidelines and Guideline Watches, Arlington, VA: American Psychiatric Association, vol. 1, 2006, doi:10.1176/appi.books.9780890423363.148430, ISBN 0-89042-336-9, retrieved 2022-01-26
- Hahn CG, Gyulai L, Baldassano CF, Lenox RH (June 2004). "The current understanding of lamotrigine as a mood stabilizer". The Journal of Clinical Psychiatry. 65 (6): 791–804. doi:10.4088/JCP.v65n0610. PMID 15291656.
- Bobo, WV (October 2017). "The Diagnosis and Management of Bipolar I and II Disorders: Clinical Practice Update". Mayo Clinic Proceedings. 92 (10): 1532–1551. doi:10.1016/j.mayocp.2017.06.022. ISSN 1942-5546. PMID 28888714. S2CID 34182938.
- McIntyre RS, Berk M, Brietzke E, Goldstein BI, López-Jaramillo C, Kessing LV, Malhi GS, Nierenberg AA, Rosenblat JD, Majeed A, Vieta E (December 2020). "Bipolar disorders". The Lancet. 396 (10265): 1841–1856. doi:10.1016/S0140-6736(20)31544-0. PMID 33278937. S2CID 227258944.
- Skeppar P, Adolfsson R (1 January 2006). "Bipolar II and the bipolar spectrum". Nordic Journal of Psychiatry. 60 (1): 7–26. doi:10.1080/08039480500504685. PMID 16500795. S2CID 31045895.
- Sandlin EK, Gao Y, El-Mallakh RS (2014). "Pharmacotherapy of bipolar disorder: current status and emerging options". Clinical Practice. 11 (1): 39–48. doi:10.2217/cpr.13.85. S2CID 31900250.
- Scott, Jan; Colom, Francesc; Vieta, Eduard (February 2007). "A meta-analysis of relapse rates with adjunctive psychological therapies compared to usual psychiatric treatment for bipolar disorders". The International Journal of Neuropsychopharmacology. 10 (1): 123–129. doi:10.1017/S1461145706006900. ISSN 1461-1457. PMID 16787554.
- "Understanding Bipolar Disorder -- Treatment". WedMD.com. Retrieved 22 November 2011.
- Smith M (2008). "Survival Strategies for Managing and Prospering with Bipolar II Disorder". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Cambridge, England: Cambridge University Press. pp. 195–203. ISBN 978-0-521-87314-7.
- Randall C (2010). "Chapter 1". Neuropsychological emotion processing abnormalities in bipolar disorder I and II (PhD thesis). University of Nevada. Archived from the original on 8 January 2012. Retrieved 19 October 2011.
- Bridley, Alexis; Daffin Jr., Lee W. (2020). Abnormal Psychology 2nd edition (PDF). Washington State University. pp. 4–12.
- McAllister-Williams RH (March 2006). "Relapse prevention in bipolar disorder: a critical review of current guidelines". Journal of Psychopharmacology. 20 (2 Suppl): 12–6. doi:10.1177/1359786806063071. PMID 16551667. S2CID 20569865.
- Hadjipavlou G (2008). "Mood Stabilisers in treatment of Bipolar II Disorder". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Cambridge, England: Cambridge University Press. pp. 120–132. ISBN 978-0-521-87314-7.
- Wingo AP, Baldessarini RJ, Compton MT, Harvey PD (May 2010). "Correlates of recovery of social functioning in types I and II bipolar disorder patients". Psychiatry Research. 177 (1–2): 131–4. doi:10.1016/j.psychres.2010.02.020. PMC 2859974. PMID 20334933.
- Rosa AR, Bonnín CM, Vázquez GH, Reinares M, Solé B, Tabarés-Seisdedos R, Balanzá-Martínez V, González-Pinto A, Sánchez-Moreno J, Vieta E (December 2010). "Functional impairment in bipolar II disorder: is it as disabling as bipolar I?". Journal of Affective Disorders. 127 (1–3): 71–6. doi:10.1016/j.jad.2010.05.014. PMID 20538343.
- Chang JS, Choi S, Ha K, Ha TH, Cho HS, Choi JE, Cha B, Moon E (June 2011). "Differential pattern of semantic memory organization between bipolar I and II disorders". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 35 (4): 1053–8. doi:10.1016/j.pnpbp.2011.02.020. PMID 21371517. S2CID 42808093.
- Benazzi F (2008). "Management Commentary". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Cambridge, England: Cambridge University Press. pp. 232–236. ISBN 978-0-521-87314-7.
- MacQueen GM, Young LT (March 2001). "Bipolar II disorder: symptoms, course, and response to treatment". Psychiatric Services. 52 (3): 358–61. doi:10.1176/appi.ps.52.3.358. PMID 11239105.
- Fieve RR (2009). Bipolar Breakthrough: The Essential Guide to Going Beyond Moodswings to Harness Your Highs, Escape the Cycles of Recurrent Depression, and Thrive with Bipolar II. New York: Rodale. pp. 232. ISBN 978-1-60529-645-6.
- Manicavasagar V (2008). "The role of psychological interventions in managing Bipolar II Disorder". In Parker G (ed.). Bipolar II Disorder: Modelling, Measuring, and Managing. Cambridge, England: Cambridge University Press. pp. 151–176. ISBN 978-0-521-87314-7.
- Jamison KR (2000). "Suicide and bipolar disorder". The Journal of Clinical Psychiatry. 61 (Suppl 9): 47–51. PMID 10826661.
- Pedersen, Carsten Bøcker; Mors, Ole; Bertelsen, Aksel; Waltoft, Berit Lindum; Agerbo, Esben; McGrath, John J.; Mortensen, Preben Bo; Eaton, William W. (May 2014). "A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders". JAMA Psychiatry. 71 (5): 573–581. doi:10.1001/jamapsychiatry.2014.16. ISSN 2168-6238. PMID 24806211.
- Merikangas, Kathleen R.; Jin, Robert; He, Jian-Ping; Kessler, Ronald C.; Lee, Sing; Sampson, Nancy A.; Viana, Maria Carmen; Andrade, Laura Helena; Hu, Chiyi; Karam, Elie G.; Ladea, Maria (March 2011). "Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative". Archives of General Psychiatry. 68 (3): 241–251. doi:10.1001/archgenpsychiatry.2011.12. ISSN 1538-3636. PMC 3486639. PMID 21383262.
- Clemente, Adauto S.; Diniz, Breno S.; Nicolato, Rodrigo; Kapczinski, Flavio P.; Soares, Jair C.; Firmo, Josélia O.; Castro-Costa, Érico (April 2015). "Bipolar disorder prevalence: a systematic review and meta-analysis of the literature". Revista Brasileira de Psiquiatria (Sao Paulo, Brazil: 1999). 37 (2): 155–161. doi:10.1590/1516-4446-2012-1693. ISSN 1809-452X. PMID 25946396.
- Rowland, Tobias A.; Marwaha, Steven (September 2018). "Epidemiology and risk factors for bipolar disorder". Therapeutic Advances in Psychopharmacology. 8 (9): 251–269. doi:10.1177/2045125318769235. ISSN 2045-1253. PMC 6116765. PMID 30181867.
- Rowland, Tobias A.; Marwaha, Steven (26 April 2018). "Epidemiology and risk factors for bipolar disorder". Therapeutic Advances in Psychopharmacology. 8 (9): 251–269. doi:10.1177/2045125318769235. ISSN 2045-1253. PMC 6116765. PMID 30181867.
- Shorter E (2005-02-17). A historical dictionary of psychiatry. Oxford University Press. p. 132. ISBN 978-0-19-803923-5.
- Thompson, JR (2012). A Jungian Approach to Bipolar Disorder: Rejoining The Split Archetype. Soul Books. Retrieved 16 February 2022.
- Jung CG (1903). "On manic mood disorder". Psychiatric Studies. Vol. 1 Collected works. translated by R.F.C Hull. Routledge and Kegan Paul (1970) (second ed.). pp. 109–111.
- Frances A, Jones KD (August 2012). "Bipolar disorder type II revisited". Bipolar Disorders. 14 (5): 474–7. doi:10.1111/j.1399-5618.2012.01038.x. PMID 22834459.
- Connolly R (6 April 2012). "Hell and Black". The Age.
- Burger, David (June 22, 2011). "Comic Maria Bamford will cross personal boundaries at Utah show". The Salt Lake Tribune.
I was re-diagnosed (after a three-day stay at the hospital) as Bipolar II
- Allen T (29 September 2010). "Geoff Bullock Opens Up". ChristianFaith.com. Retrieved 23 October 2014.
- Cagle, Jess. "Mariah Carey: My Battle with Bipolar Disorder". PEOPLE.com. Retrieved 2018-04-11.
- Bennett, Jennifer (2010-10-20). "Gap suicide 'preventable'". Wentworth Courier. Archived from the original on 2010-10-29. Retrieved 2010-10-25.
- Ewens H (29 August 2019). "You Wouldn't Believe Joe Gilgun's Life Story – So He Spun It into TV". Vice.
- "Shane Hmiel's Story on NASCAR Race-Hub Part 1". YouTube.com. Fox Sports, SPEED, NASCAR Race Hub. July 21, 2011. Archived from the original on 2021-12-12. Retrieved 4 October 2014.
- "Rep. Jackson Jr. treated for bipolar disorder". USA Today. August 13, 2012. Retrieved August 13, 2012.
- Altman LK (July 23, 2012). "Hasty and Ruinous 1972 Pick Colors Today's Hunt for a No. 2". The New York Times. Retrieved June 24, 2017.
- Slaughter, Adele (30 May 2002). "Carie Fisher 'Strikes Back' at Mental Illness". USA Today.
- Cotliar S (20 April 2011). "Demi Lovato: I Have Bipolar Disorder". People.
- Vena J (20 April 2011). "Demi Lovato Has Bipolar Disorder". MTV News.
- Boy Interrupted (DVD). HBO Films. 2009.
- Rossi R (June 5, 2008). "The Lynn Cullen Show" (Interview). Interviewed by Lynn Cullen.
my father was bi-polar one, and I'm bi-polar two.
- Graff, Gary (23 January 2015). "U.K. Singer-Songwriter Rumer on Battling Depression & Bipolar 2 to Create 'Into Colour'". Billboard.
- "Catherine Zeta-Jones treated for bipolar disorder". BBC News. 14 April 2011.