Ceruminous adenocarcinoma
Ceruminous adenocarcinoma is a malignant neoplasm derived from ceruminous glands of the external auditory canal. This tumor is rare, with several names used in the past.[3][4] Synonyms have included cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC),[1][2] and ceruminous mucoepidermoid carcinoma.
| Ceruminous adenocarcinoma | |
|---|---|
| Other names | Cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC),[1][2] ceruminous mucoepidermoid carcinoma |
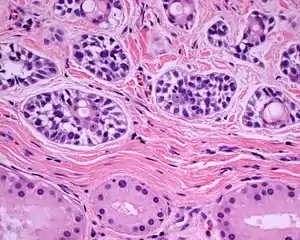 | |
| A high power photomicrograph of a ceruminous type adenoid cystic carcinoma | |
| Specialty | ENT surgery |
Classification
This tumor only affects the outer 1/3 to 1/2 of the external auditory canal as a primary site. If this area is not involved, the diagnosis should be questioned. The most common tumor type is ceruminous adenoid cystic carcinoma and ceruminous adenocarcinoma, NOS.
Signs and symptoms
Pain is the most common symptom, followed by either sensorineural or conductive hearing loss, tinnitus or drainage (discharge). A mass lesion may be present, but it is often slow growing.[3]
Diagnosis
Imaging
Imaging studies are used to define the extent of the tumor and to exclude direct extension from the parotid gland or nasopharynx.[5] The imaging findings are usually non-specific, and cannot give a specific diagnosis.
Pathology
Tumors are polypoid, identified most often in the posterior canal. It is not uncommon to have ulceration of the surface squamous epithelium. Most tumors are about 1.5 cm in greatest dimension, a limitation of the anatomic site rather than of the tumor type itself.[3] The tumors are separated into three main histologic or microscopic types:
- Ceruminous adenocarcinoma, NOS
- Ceruminous adenoid cystic carcinoma
- Ceruminous mucoepidermoid carcinoma
All of the tumors are infiltrative into the soft tissue, benign ceruminous glands, and/or bone. The tumor may expand into the overlying squamous surface epithelium, but it usually does not arise from the surface epithelium. The tumors are cellular, arranged in solid, cystic, cribriform, glandular, and single cell patterns. It is uncommon to see tumor necrosis, but when it is present, it is diagnostic of cancer. The same is true of perineural invasion. Nuclear pleomorphism is usually easily to identify, with the nuclei containing prominent nucleoli. There are usually increased mitotic figures, including atypical forms. There are usually areas of stromal fibrosis. Ceroid (cerumen or ear wax) is not seen in malignancies, although it is seen in benign tumors. The specific features of each tumor type can help with the separation into adenoid cystic carcinoma or mucoepidermoid types.[3]
Immunohistochemistry
Immunohistochemistry will help to show the biphasic appearance of the tumor, highlighting the basal or the luminal cells:
Differential diagnoses
It is important to exclude a tumor which is directly extending into the ear canal from the parotid salivary gland, especially when dealing with an adenoid cystic or mucoepidermoid carcinoma. This can be eliminated by clinical or imaging studies. Otherwise, the histologic differential diagnosis includes a ceruminous adenoma (a benign ceruminous gland tumor)[7][8] or a neuroendocrine adenoma of the middle ear (middle ear adenoma).[9]
Management
Wide, radical, complete surgical excision is the treatment of choice, with free surgical margins to achieve the best outcome and lowest chance of recurrence. Radiation is only used for palliation. In general, there is a good prognosis, although approximately 50% of patients die from disease within 3–10 years of presentation.[3]
Epidemiology
This is a very rare neoplasm accounting for approximately 0.0003% of all tumors and about 2.5% of all external ear neoplasms.[3] Ceruminous adenocarcinomas (CA) is a rare type of tumor and has a very small amount of literature on it. The ages to develop ceruminous adenocarcinomas are between 21 and 92 and being most present around 48.[10] There is no statistical difference between being male and female and developing the tumor[10] and there is no racial inclination.[11] The typical treatment of CA is through surgery and radiation. The type of cut is important with the recurrence rate.[10] Long-term outcomes are better when having the wide cut near the tumor.[10] If the tumor reoccurs there is an 83% chance of mortality and if it does not reoccur there is a 9% chance of mortality.[10] Older people have a lower survival rate than younger ones.[12] The local reoccurrence rate is 49% and the distant metastasis rate is 13%.[11] With local reoccurrence being at 49%, follow-up is very important.[11]
References
- Dong, F.; Gidley, P. W.; Ho, T.; Luna, M. A.; Ginsberg, L. E.; Sturgis, E. M. (2008). "Adenoid Cystic Carcinoma of the External Auditory Canal". The Laryngoscope. 118 (9): 1591–1596. doi:10.1097/MLG.0b013e31817c42a8. PMID 18677277. S2CID 20216496.
- Perzin, K. H.; Gullane, P.; Conley, J. (1982). "Adenoid cystic carcinoma involving the external auditory canal. A clinicopathologic study of 16 cases". Cancer. 50 (12): 2873–2883. doi:10.1002/1097-0142(19821215)50:12<2873::aid-cncr2820501230>3.0.co;2-r. PMID 6291744.
- Crain, N.; Nelson, B. L.; Barnes, E. L.; Thompson, L. D. R. (2008). "Ceruminous Gland Carcinomas: A Clinicopathologic and Immunophenotypic Study of 17 Cases". Head and Neck Pathology. 3 (1): 1–17. doi:10.1007/s12105-008-0095-9. PMC 2807538. PMID 20596983.
- Hicks, G. W. (1983). "Tumors arising from the glandular structures of the external auditory canal". The Laryngoscope. 93 (3): 326–340. doi:10.1288/00005537-198303000-00016. PMID 6300574. S2CID 31253554.
- Aikawa, H.; Tomonari, K.; Okino, Y.; Hori, F.; Ueyama, T.; Suenaga, S.; Bundo, J.; Tsuji, K. (1997). "Adenoid cystic carcinoma of the external auditory canal: Correlation between histological features and MRI appearances". The British Journal of Radiology. 70 (833): 530–532. doi:10.1259/bjr.70.833.9227237. PMID 9227237.
- Ito, K.; Ito, T.; Tsukuda, M.; Kanisawa, M. (1993). "An immunohistochemical study of adenoid cystic carcinoma of the external auditory canal". European Archives of Oto-Rhino-Laryngology. 250 (4): 240–244. doi:10.1007/bf00171533. PMID 7690238. S2CID 11946085.
- Thompson, L. D.; Nelson, B. L.; Barnes, E. L. (2004). "Ceruminous adenomas: A clinicopathologic study of 41 cases with a review of the literature". The American Journal of Surgical Pathology. 28 (3): 308–318. doi:10.1097/00000478-200403000-00003. PMID 15104293. S2CID 27571673.
- Dehner, L. P.; Chen, K. T. (1980). "Primary tumors of the external and middle ear. Benign and malignant glandular neoplasms". Archives of Otolaryngology. 106 (1): 13–19. doi:10.1001/archotol.1980.00790250015004. PMID 6243462.
- Torske, K. R.; Thompson, L. D. R. (2002). "Adenoma versus Carcinoid Tumor of the Middle Ear: A Study of 48 Cases and Review of the Literature". Modern Pathology. 15 (5): 543–555. doi:10.1038/modpathol.3880561. PMID 12011260.
- Saunders, T. F. C.; Monksfield, P. (2014). "A Case of Conservatively Managed Invasive Ceruminoma and a Review of the Literature". Case Reports in Otolaryngology. 2014: 897540. doi:10.1155/2014/897540. ISSN 2090-6765. PMC 4129918. PMID 25143852.
- Wanner, Brian; Rismiller, Kyle; Carr, David R. (2021-06-23). "Treatment and survival outcomes of ceruminous carcinomas of the external auditory canal: a SEER database analysis and literature review". Archives of Dermatological Research. doi:10.1007/s00403-021-02257-4. ISSN 1432-069X. PMID 34160677. S2CID 235600454.
- Ruhl, Douglas S.; Tolisano, Anthony M.; Swiss, Tyler P.; Littlefield, Philip D.; Golden, J. Blake (2016). "Ceruminous adenocarcinoma: An analysis of the Surveillance Epidemiology and End Results (SEER) database". American Journal of Otolaryngology. 37 (2): 70–73. doi:10.1016/j.amjoto.2015.11.005. PMID 26954854.
Further reading
- Lester D. R. Thompson; Bruce M. Wenig (2011). Diagnostic Pathology: Head and Neck: Published by Amirsys. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 7:90–93. ISBN 978-1-931884-61-7.