Contact tracing
In public health, contact tracing is the process of identifying persons who may have been exposed to an infected person ("contacts") and subsequent collection of further data to assess transmission. By tracing the contacts of infected individuals, testing them for infection, and isolating or treating the infected, this public health tool aims to reduce infections in the population. In addition to infection control, contact tracing serves as a means to identify high-risk and medically vulnerable populations who might be exposed to infection and facilitate appropriate medical care.[1] In doing so, public health officials utilize contact tracing to conduct disease surveillance and prevent outbreaks.[2] In cases of diseases of uncertain infectious potential, contact tracing is also sometimes performed to learn about disease characteristics, including infectiousness. Contact tracing is not always the most efficient method of addressing infectious disease. In areas of high disease prevalence, screening or focused testing may be more cost-effective.

In summary the goals of contact tracing include[3]:
- To interrupt ongoing transmission and reduce the spread of an infection
- To alert contacts to the possibility of infection and offer preventive services or prophylactic care
- To offer diagnosis, counseling and treatment to already infected individuals
- If the infection is treatable, to help prevent reinfection of the originally infected patient
- To learn about the epidemiology of a disease in a particular population
- To be used as tool in multifaceted prevention strategy to effectively curb the spread of an infectious disease.
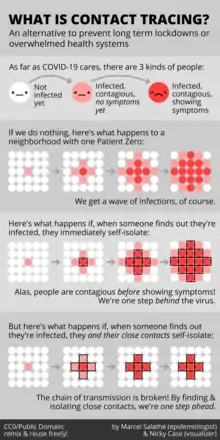 Visual depiction disease spread with and without contact tracing.
Visual depiction disease spread with and without contact tracing.
History
Contact tracing programs were first implemented to track syphilis cases in the 1930s. Initial efforts proved to be difficult given the stigmatization associated with sexually transmitted infections (STIs). Individuals were reluctant to report infections because they were concerned for their privacy. Revealing partner history and details about sexual activity was challenging as it affected relationships among individuals and community members. In addition, public health officials targeted certain populations such as sex workers, minorities, and at-risk populations further eliciting feeling of fear, shame, and guilt in society. With these negative implications of contact tracing, particularly in the space of sexually transmitted infections, public health officials found it difficult to elicit information from exposed individuals. During the HIV epidemic, many affected person were hesitant to report information, which hindered the efforts to understand HIV and curb the spread.[2] To combat some of the negative stigma associated with contact tracing and STIs, health departments sometimes referred to contact tracing as partner notification in the 1980s.[4] Partner notification, also called partner care, is a subset of contact tracing aimed specifically at informing sexual partners of an infected person and addressing their health needs. This definition evolved from identifying infected individuals to including a comprehensive program that encompasses counseling and medical care to treat the infection.[4]
Diseases for which contact tracing is commonly performed include tuberculosis, vaccine-preventable infections like measles, sexually transmitted infections (including HIV), blood-borne infections, Ebola, bacterial infections, and novel virus infections (e.g., SARS-CoV, H1N1, and SARS-CoV-2). Contact tracing has been a pillar of communicable disease control in public health for decades. The eradication of smallpox, for example, was achieved by exhaustive contact tracing to find all infected persons.[5] This was followed by isolation of infected individuals and immunization of the surrounding community and contacts at-risk of contracting smallpox.
Steps in contact tracing


Contact tracing generally involves the following steps:
- An individual is identified as having a communicable disease (often called the index case). This case may be reported to public health or managed by the primary health care provider.
- The index case is interviewed to learn about their movements, whom they have been in close contact with or who their sexual partners have been.
- Depending on the disease and the context of the infection, family members, health care providers, and anyone else who may have knowledge of the case's contacts may also be interviewed.
- Once contacts are identified, public health workers contact them to offer counseling, screening, prophylaxis, and/or treatment.
- Contacts may be isolated (e.g. required to remain at home) or excluded (e.g. prohibited from attending a particular location, like a school) if deemed necessary for disease control.
- If contacts are not individually identifiable (e.g. members of the public who attended the same location), broader communications may be issued, like media advisories.
Although contact tracing can be enhanced by letting patients provide information, medication, and referrals to their contacts, evidence demonstrates that direct public health involvement in notification is most effective.[6]
Relevance of contacts
.jpg.webp)

The types of contacts that are relevant for public health management vary with the communicable disease because of differing modes of transmission. For sexually transmitted infections, sexual contacts of the index case are relevant, as well as any babies born to the index case. For blood-borne infections, blood transfusion recipients, contacts who shared a needle, and anyone else who could have been exposed to the blood of the index case are relevant. For pulmonary tuberculosis, people living in the same household or spending a significant amount of time in the same room as the index case are relevant.[7]
Outbreaks
Although contact tracing is most commonly used for control of diseases, it is also a critical tool for investigating new diseases or unusual outbreaks. For example, as was the case with SARS, contact tracing can be used to determine if probable cases are linked to known cases of the disease, and to determine if secondary transmission is taking place in a particular community.[8]
Contact tracing has also been initiated among flight passengers during the containment phase of larger pandemics, such as the 2009 pandemic H1NI influenza. However, there continue to be large challenges in achieving the goals of contact tracing during such chaotic events.[9] Development of better guidelines and strategies for pandemic contact tracing continues.[10]
Identification of etiology
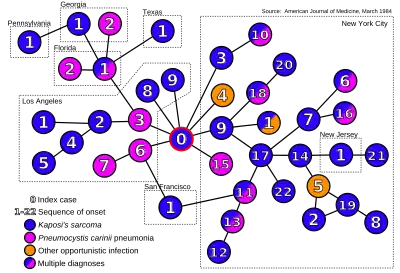
Contact tracing can help identify the etiology of a disease outbreak.[12] In 1984, contact tracing provided the first direct evidence that AIDS may be spread by an infectious agent during sexual contacts.[13][11] The infective agent has since been identified as HIV.[14]
Backward and forward tracing
Backward (or reverse or retrospective) tracing seeks to establish the source of an infection, by looking for contacts before infection.
Forward tracing is the process of looking for contacts after infection, so as to prevent further disease spread.
Backward contact tracing has been advised as a way of finding people with tuberculosis who are missed by routine health services.[15]
For epidemics with high heterogeneity in infectiousness, it might make sense, depending on local contact tracing capacity, to adopt a hybrid strategy of "regular" forward contact tracing combined with contact tracing backwards in time to find the source of infection of the index case itself. Indeed, due to a statistical effect similar to the friendship paradox, the index case is expected to have a much higher number of infected "offspring".
During the COVID-19 pandemic, the adoption by Japan in early spring 2020 of an approach focusing on backward contact tracing was hailed as successful,[16][17][18][19] and other countries which managed to keep the epidemic under control, such as South Korea[20] and Uruguay,[21][22] are said to have also used the approach.[23] There is mounting theoretical support for the adoption of this strategy in the context of COVID, if local resources allow.[24][25][26][27] Journalist and author Laurie Garrett pointed out in late October 2020, however, that the amount of the virus in the U.S. is now so large that no health departments has the resources to contact and trace.[28] Additionally, officials overlooked the effect of mistrust in the government and conspiracy theories regarding the virus on thwarting contact tracing efforts in the U.S.[29]
In September 2020, science writer and sociologist Zeynep Tufekci wrote a long piece in The Atlantic on the lack of attention by many public health authorities to the index of dispersion of the SARS-CoV-2 virus and its implications for contact tracing.[30]
In October 2020, German virologist Christian Drosten called on all citizens of Germany to maintain a diary of their close contacts, in order to facilitate backward tracing and thus help contact tracing teams to find disease clusters.[31]
Technology
Case management
Case management software is often used by contact tracers to maintain records of cases and contact tracing activities.[32] This is typically a cloud database that may have specialized features such as the ability to use SMS or email directly within the software to notify people believed to have been in close contact with someone carrying an infectious disease.[33] Vendors offering contact tracing case management software include Salesforce, Microsoft and Watkyn.[34][35][36]
.jpg.webp)
Mobile phones
Smartphones can provide proximity information useful for contact tracing using GPS, Bluetooth or Wifi signals.[37] Facebook Labs patented the use of Bluetooth on smartphones for this in 2018.[38] On 10 April 2020, Apple and Google, who account for most of the world's mobile operating systems, announced COVID-19 apps for iOS and Android.[39] Relying on Bluetooth Low Energy (BLE) wireless radio signals for proximity information,[40] the new tools would warn people that they had been in contact with who are infected by SARS-CoV-2.[39][41]
Protocols
Various protocols, such as Pan-European Privacy-Preserving Proximity Tracing (PEPP-PT),[42] Whisper Tracing Protocol,[43] Decentralized Privacy-Preserving Proximity Tracing (DP-PPT/DP-3T),[44][45] TCN Protocol, Contact Event Numbers (CEN), Privacy Sensitive Protocols And Mechanisms for Mobile Contact Tracing (PACT)[46] and others, are being discussed to preserve user privacy.
The DP-3T and TCN protocols are currently used by Switzerland, Austria, Estonia, Finland, Italy, and the UK. While France, Australia, New Zealand, and Singapore use PEPP-PT or BlueTrace based systems.[47]
Ethical and legal issues
Challenges with contact tracing can arise related to issues of medical privacy and confidentiality. Public health practitioners often are mandated reporters, required to act to contain a communicable disease within a broader population and also ethically obliged to warn individuals of their exposure. Simultaneously, infected individuals have a recognized right to medical confidentiality. Public health teams typically disclose the minimum amount of information required to achieve the objectives of contact tracing. For example, contacts are only told that they have been exposed to a particular infection, but not informed of the person who was the source of the exposure.[6]
Some activists and health care providers have expressed concerns that contact tracing may discourage persons from seeking medical treatment for fear of loss of confidentiality and subsequent stigma, discrimination, or abuse. This has been of particular concern regarding contact tracing for HIV. Public health officials have recognized that the goals of contact tracing must be balanced with the maintenance of trust with vulnerable populations and sensitivity to individual situations.[6]
See also
- Disease surveillance
- Government by algorithm
- Intentional contagion of infection
- Mathematical modelling of infectious disease
- Trace evidence
References
- "Coronavirus disease (COVID-19): Contact tracing". www.who.int. Retrieved 2022-11-03.
- Brandt AM (August 2022). "The History of Contact Tracing and the Future of Public Health". American Journal of Public Health. 112 (8): 1097–1099. doi:10.2105/AJPH.2022.306949. PMC 9342804. PMID 35830671.
- CDC (2020-02-11). "Health Departments". Centers for Disease Control and Prevention. Retrieved 2022-11-03.
- "Reflections on the History of Contact Tracing". O'Neill. 2020-07-13. Retrieved 2022-11-03.
- Scutchfield FD (2003). Principles of public health practice. Clifton Park, New York: Delmar Learning. p. 71. ISBN 0-76682843-3.
- Ontario Provincial Infectious Diseases Advisory Committee (2009). Sexually transmitted infections best practices and contact tracing best practice recommendations. Toronto, Canada: Ontario Ministry of Health and Long-Term Care. ISBN 978-1-42497946-2.
- Australasian Contact Tracing Manual. Darlinghurst, New South Wales, Australia: Australasian Society for HIV Medicine. 2010. ISBN 978-1-920773-95-3.
- "Severe Acute Respiratory Syndrome (SARS) – multi-country outbreak". Global Alert and Response. WHO. Archived from the original on 2003-06-18. Retrieved 2013-05-28.
- Swaan CM, Appels R, Kretzschmar ME, van Steenbergen JE (December 2011). "Timeliness of contact tracing among flight passengers for influenza A/H1N1 2009". BMC Infectious Diseases. 11 (1): 355. doi:10.1186/1471-2334-11-355. PMC 3265549. PMID 22204494.
- Ferretti L, Wymant C, Kendall M, Zhao L, Nurtay A, Abeler-Dörner L, et al. (May 2020). "Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing". Science. 368 (6491): eabb6936. doi:10.1126/science.abb6936. PMC 7164555. PMID 32234805.
- Auerbach DM, Darrow WW, Jaffe HW, Curran JW (March 1984). "Cluster of cases of the acquired immune deficiency syndrome. Patients linked by sexual contact". The American Journal of Medicine. 76 (3): 487–492. doi:10.1016/0002-9343(84)90668-5. PMID 6608269.
- Riley S, Fraser C, Donnelly CA, Ghani AC, Abu-Raddad LJ, Hedley AJ, et al. (June 2003). "Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions". Science. 300 (5627): 1961–1966. Bibcode:2003Sci...300.1961R. doi:10.1126/science.1086478. PMID 12766206.
- Klovdahl AS (1985-01-01). "Social networks and the spread of infectious diseases: the AIDS example". Social Science & Medicine. 21 (11): 1203–1216. doi:10.1016/0277-9536(85)90269-2. PMID 3006260.
- Blattner W, Gallo RC, Temin HM (July 1988). "HIV causes AIDS". Science. 241 (4865): 515–516. Bibcode:1988Sci...241..515B. doi:10.1126/science.3399881. PMID 3399881.
- "StopTB Field guide 6: Using Contact Investigation to Improve TB Case Detection" (PDF). Stop TB Partnership. 2018.
- "The 'Japan model' that tackled coronavirus". Financial Times.
- Nishimura Y (2020-07-07). "Opinion | How Japan Beat Coronavirus Without Lockdowns". The Wall Street Journal. ISSN 0099-9660. Retrieved 2020-10-19.
- Oshitani H (November 2020). "Cluster-Based Approach to Coronavirus Disease 2019 (COVID-19) Response in Japan, from February to April 2020". Japanese Journal of Infectious Diseases. 73 (6): 491–493. doi:10.7883/yoken.JJID.2020.363. PMID 32611985. S2CID 220310375.
- "[Addendum] Japan's Cluster-based Approach" (PDF). Ministry of Health, Labour and Welfare. 2020-05-28.
- Lee SW, Yuh WT, Yang JM, Cho YS, Yoo IK, Koh HY, et al. (August 2020). "Nationwide Results of COVID-19 Contact Tracing in South Korea: Individual Participant Data From an Epidemiological Survey". JMIR Medical Informatics. 8 (8): e20992. doi:10.2196/20992. PMC 7470235. PMID 32784189.
- Taylor L (September 2020). "Uruguay is winning against covid-19. This is how". BMJ. 370: m3575. doi:10.1136/bmj.m3575. PMID 32948599. S2CID 221778076.
- Moreno P, Moratorio G, Iraola G, Fajardo Á, Aldunate F, Pereira-Gómez M, et al. (2020-07-27). "An effective COVID-19 response in South America: the Uruguayan Conundrum". medRxiv (Preprint): 2020.07.24.20161802. doi:10.1101/2020.07.24.20161802. S2CID 220793010.
- Crozier A, Mckee M, Rajan S (November 2020). "Fixing England's COVID-19 response: learning from international experience". Journal of the Royal Society of Medicine. 113 (11): 422–427. doi:10.1177/0141076820965533. PMC 7686527. PMID 33058751. S2CID 222839822.
- Bradshaw WJ, Alley EC, Huggins JH, Lloyd AL, Esvelt KM (2020). "Bidirectional contact tracing dramatically improves COVID-19 control". medRxiv. doi:10.1101/2020.05.06.20093369. S2CID 218561613.
- Endo A, Leclerc QJ, Knight GM, Medley GF, Atkins KE, Funk S, Kucharski AJ (2020). "Implication of backward contact tracing in the presence of overdispersed transmission in COVID-19 outbreaks". Wellcome Open Research. 5: 239. doi:10.12688/WELLCOMEOPENRES.16344.1. PMC 7610176. PMID 33154980.
- Lambert A (2021). "A mathematical assessment of the efficiency of quarantining and contact tracing in curbing the COVID-19 epidemic". Mathematical Modelling of Natural Phenomena. 16: 53. doi:10.1101/2020.05.04.20091009. S2CID 218964036.
- Kojaku S, Hébert-Dufresne L, Mones E, Lehmann S, Ahn YY (May 2021). "The effectiveness of backward contact tracing in networks". Nature Physics. 17 (5): 652–658. arXiv:2005.02362. Bibcode:2021NatPh..17..652K. doi:10.1038/s41567-021-01187-2. PMC 8340850. PMID 34367312.
- "Laurie Garrett: The amount of virus in the U.S. Is so large that 'no one has health departments large enough to do contact tracing'". MSNBC.
- Mueller B (2020-10-03). "Contact Tracing, Key to Reining In the Virus, Falls Flat in the West". The New York Times. ISSN 0362-4331. Retrieved 2021-04-19.
- Tufekci Z (2020-09-30). "This Overlooked Variable Is the Key to the Pandemic". The Atlantic. Retrieved 2020-10-19.
- Scharpenberg J (2020-10-13). "Drosten fordert Corona-Tagebuch zur besseren Kontaktnachverfolgung". www.waz.de (in German). Retrieved 2020-10-21.
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 2020-06-17. Retrieved 2020-07-18.
- "ContactPath by Watkyn Launches to Reduce the Spread of COVID-19". prnewswire.com. Retrieved 2020-07-14.
- "Marc Benioff says 35 states are now using Salesforce's contact tracing technology for coronavirus". cnbc.com. 2020-06-25. Retrieved 2020-07-14.
- "Greater Manchester plans case management for contact tracing". ukauthority.com. Retrieved 2020-07-14.
- "Contact Tracing Platform Developed in QuickBase". insightfromanalytics.com. 2020-07-14. Retrieved 2020-07-14.
- "Privacy-preserving controls for sharing mHealth data - ProQuest". search.proquest.com. Retrieved 2020-07-01.
- WO 2019139630, "Proximity-based trust", issued 2018-01-16, assigned to Facebook Inc.
- Sherr I, Nieva R (2020-04-10). "Apple and Google are building coronavirus tracking tech into iOS and Android – The two companies are working together, representing most of the phones used around the world". CNET. Archived from the original on 2020-04-10. Retrieved 2020-04-10.
- "Contact Tracing – Bluetooth Specification" (PDF). covid19-static.cdn-apple.com (Preliminary ed.). 2020-04-10. Archived (PDF) from the original on 2020-04-10. Retrieved 2020-04-10.
- Heberlein M (2020-01-04). "Kommentar: Mit Corona-App zurück zum halbwegs normalen Leben". Tagesschau.de (in German). Retrieved 2020-04-05.
- Natasha L (2020-04-01). "An EU coalition of techies is backing a 'privacy-preserving' standard for COVID-19 contacts tracing". TechCrunch. Archived from the original on 2020-04-10. Retrieved 2020-04-11.
- "Latest weapon in tracing and tracking coronavirus infections: your smartphone". SFChronicle.com. 2020-04-23. Retrieved 2020-05-06.
- Lomas N (2020-04-06). "EU privacy experts push a decentralized approach to COVID-19 contacts tracing". TechCrunch. Archived from the original on 2020-04-10. Retrieved 2020-04-11.
- Troncoso C, Payer M, Hubaux JP, Salathé M, Larus J, Bugnion E, et al. (2020-05-25). "Decentralized privacy-preserving proximity tracing". arXiv. arXiv:2005.12273.
- Chan J, Foster D, Gollakota S, Horvitz E, Jaeger J, Kakade S, et al. (2020-04-07). "PACT: Privacy Sensitive Protocols And Mechanisms for Mobile Contact Tracing". arXiv:2004.03544v1 [cs.CR].
- "Contact tracing apps: How to fight COVID-19 and protect your privacy". Proton Mail Blog. 2020-05-15. Retrieved 2020-07-02.