Drusen
Drusen, from the German word for node or geode (singular, "Druse"), are tiny yellow or white accumulations of extracellular material that build up between Bruch's membrane and the retinal pigment epithelium of the eye. The presence of a few small ("hard") drusen is normal with advancing age, and most people over 40 have some hard drusen.[1] However, the presence of larger and more numerous drusen in the macula is a common early sign of age-related macular degeneration (AMD).
| Drusen | |
|---|---|
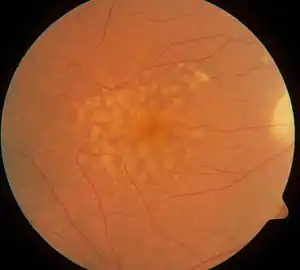 | |
| Macular soft drusen in the right eye of a 70-year-old male. | |
| Specialty | Ophthalmology |
Classification
Drusen are associated with aging and macular degeneration are distinct from another clinical entity, optic disc drusen, which is present on the optic nerve head.[2] Both age-related drusen and optic disc drusen can be observed by ophthalmoscopy. Optical coherence tomography scans of the orbits or head, calcification at the head of the optic nerve without change in size of globe strongly suggests drusen in a middle-age or elderly patient.
Whether drusen promote AMD or are symptomatic of an underlying process that causes both drusen and AMD is not known, but they are indicators of increased risk of the complications of AMD.[3]
'Hard drusen' may coalesce into 'soft drusen' which is a manifestation of macular degeneration.[4]
Pathophysiology
Around 1850, three authors, Carl Wedl, Franciscus Donders, and Heinrich Müller, gave drusen different labels. Drusen, the hallmark of AMD, were first described in 1854 by Wedl.[5] Wedl named them colloid bodies of the choroid and thought that they were incompletely developed cells. Franciscus Donders[6] called them "Colloidkugeln" (colloid spheres). Later, Heinrich Müller named them by the German word for geode, based on their glittering appearance.[7] He was convinced that drusen originated from the nuclei of the pigment cells, which he believed to belong to the choroid.[8] In view of their location between the retinal pigment epithelium (RPE) and its vascular supply, the choriocapillaris, it is possible that drusen deprive the RPE and photoreceptor cells of oxygen and nutrients. In some cases, drusen develop above the so-called pillars of the choriocapillaris that is the area between two micro vessels;[9] although important variations are observed between different subtypes of AMD.

The source of the proteins and lipids in drusen is also not clear, with potential contributions by both the RPE and the choroid. Several trace elements are present in drusen,[10] probably the most concentrated being zinc.[11] The protein composition of drusen includes apolipoproteins and oxidized proteins, likely originating from blood, RPE, and photoreceptors.[12] Drusen composition also includes members of the complement system. Zinc in drusen has been suggested to play a role in drusen formation by precipitating and inhibiting the elements of the complement cascade, especially complement factor H.[11]
The presence of molecules that regulate inflammation in drusen has led some investigators to conclude that these deposits are product of the immune system.[13]
Diagnosis
Usually being asymptomatic, drusen are typically found during routine eye exams where the pupils have been dilated.[14]
Treatment
Laser treatment of drusen has been studied. While it is possible to eliminate drusen with this treatment strategy, it has been shown that this fails to reduce the risk of developing the choroidal neovascularisation which causes the blindness associated with age-related macular degeneration.[15]
See also
Notes
- Silvestri G, Williams MA, McAuley C, Oakes K, Sillery E, Henderson DC, Ferguson S, Silvestri V, Muldrew KA (2012). "Drusen prevalence and pigmentary changes in Caucasians aged 18-54 years". Eye (Lond). 26 (10): 1357–62. doi:10.1038/eye.2012.165. PMC 3470061. PMID 22899005.
- Davis PL, Jay WM (December 2003). "Optic nerve head drusen". Semin Ophthalmol. 18 (4): 222–42. doi:10.1080/08820530390895244. PMID 15513010. S2CID 8271755.
- "Age-Related Macular Degeneration". National Eye Institute. March 2008. Archived from the original on 2008-05-12. Retrieved 2008-05-21.
- "Macular Degeneration types and risk factors". Archived from the original on 2010-01-10. Retrieved 2010-01-26.
- Wedl C. Grundzüge der pathologischen Histologie Wien: Gerold, C; 1854
- Donders FC (March 1855). "Beitrage zur pathologischen Anatomie des Auges". Graefes Arch Clin Exp Ophthalmol. 1 (2): 106–18. doi:10.1007/BF02720791. S2CID 45074362.
- Müller H (January 1856). "Anatomische Beiträge zur Ophthalmologie – Untersuchungen über die Glashäute des Auges, insbesondere die Glaslamelle der Chorioidea und ihre senilen Veränderungen". Graefes Arch Clin Exp Ophthalmol. 2 (2): 1–69. doi:10.1007/BF02720657. S2CID 41644271.
- de Jong PT. A Historical Analysis of the Quest for the Origins of Aging Macula Disorder, the Tissues Involved, and Its Terminology. Ophthalmol Eye Dis. 2016;8(Suppl 1):5-14. Published 2016 Nov 1. doi:10.4137/OED.S40523
- Lengyel I, Tufail A, Hosaini HA, Luthert P, Bird AC, Jeffery G (September 2004). "Association of drusen deposition with choroidal intercapillary pillars in the aging human eye". Invest. Ophthalmol. Vis. Sci. 45 (9): 2886–92. doi:10.1167/iovs.03-1083. PMID 15326099.
- van der Schaft TL, de Bruijn WC, Mooy CM, Ketelaars DA, de Jong PT (March 1992). "Element analysis of the early stages of age-related macular degeneration". Arch. Ophthalmol. 110 (3): 389–94. doi:10.1001/archopht.1992.01080150087034. PMID 1543459.
- Lengyel I, Flinn JM, Peto T, et al. (April 2007). "High concentration of zinc in sub-retinal pigment epithelial deposits". Exp. Eye Res. 84 (4): 772–80. doi:10.1016/j.exer.2006.12.015. PMID 17313944.
- Crabb JW, Miyag M, Gu X, Shadrach K, West KA, Sakaguchi H, Kamei M, Hasan A, Yan L, Rayborn ME, Salomon RG, Hollyfield JG (November 12, 2002). "Drusen proteome analysis: An approach to the etiology of age-related macular degeneration". Proc Natl Acad Sci USA. 99 (23): 14682–87. doi:10.1073/pnas.222551899. PMC 137479. PMID 12391305.
- Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF (November 2001). "An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch's membrane interface in aging and age-related macular degeneration". Prog Retin Eye Res. 20 (6): 705–32. doi:10.1016/S1350-9462(01)00010-6. PMID 11587915. S2CID 7737763.
- "Drusen Diagnosis and Treatment". 4 March 2021.
- Virgili G, Michelessi M, Parodi MB, Bacherini D, Evans JR (2015). "Laser treatment of drusen to prevent progression to advanced age-related macular degeneration". Cochrane Database Syst Rev. 2015 (10): CD006537. doi:10.1002/14651858.CD006537.pub3. PMC 4733883. PMID 26493180.
Mishra S, Goel S, Roy SS, Garg B, Parvin M, Saurabh K, Roy R. Multimodal imaging characteristics of refractile drusen. Indian journal of ophthalmology. 2019 Jan;67(1):128.