Colon cancer staging
Colon cancer staging is an estimate of the amount of penetration of a particular cancer. It is performed for diagnostic and research purposes, and to determine the best method of treatment. The systems for staging colorectal cancers depend on the extent of local invasion, the degree of lymph node involvement and whether there is distant metastasis.
Definitive staging can only be done after surgery and histopathology of colorectal carcinoma. An exception to this principle would be after a colonoscopic polypectomy of a malignant pedunculated polyp with minimal invasion. Preoperative staging of rectal cancers may be done with endoscopic ultrasound. Adjunct staging of metastasis include abdominal ultrasound, MRI, CT, PET scanning, and other imaging studies.
TNM staging system
The most common staging system is the TNM (for tumors/nodes/metastases) system, from the American Joint Committee on Cancer.[1] This system assigns a number based on three categories. "T" denotes the degree of invasion of the intestinal wall, "N" the degree of lymphatic node involvement, and "M" the degree of metastasis. Possibly, the overall Joint Committee stage is a shorter format of the TNM stage, and is usually quoted as a number I, II, III, IV derived from the TNM value grouped by prognosis; a higher number indicates a more advanced cancer and likely a worse outcome. Following is the eighth edition from 2017:
Tumor (T)
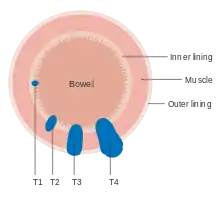
Numbers 0 to 4, with subgroups, are used to describe deepest tumor depth:[2]
- TX: The primary tumor cannot be evaluated.
- T0: No evidence of cancer in the colon or rectum.
- Tis: Carcinoma in situ; Cancer cells are found only in the epithelium or lamina propria
- T1: Growth into the submucosa
- T2: Growth into the muscularis propria
- T3: Growth through the muscularis propria and into the subserosa, or into tissues surrounding the colon or rectum (but not the visceral peritoneum or surrounding organs).
- T4a: Growth into the surface of the visceral peritoneum.
- T4b: The tumor has grown into or has attached to other organs or structures.
Node (N)
Numbers 0 to 2, and subgroups, are used to describe lymph node involvement:[2]
- NX: The regional lymph nodes cannot be evaluated.
- N0: No evidence of spread to regional lymph nodes.
- N1a: Tumor cells found in 1 regional lymph node.
- N1b: Tumor cells found in 2 or 3 regional lymph nodes.
- N1c: There are cancerous nodules near the colon that do not appear to be lymph nodes.
- N2a: Tumor cells found in 4 to 6 regional lymph nodes.
- N2b: Tumor cells found in 7 or more regional lymph nodes.
Metastasis (M)
Numbers 0 and 1, with subgroups, describe the metastasis status:[2]
- M0: No evidence of distant metastasis
- M1a: Spread to 1 other part of the body beyond the colon, rectum or regional lymph nodes.
- M1b: Spread to more than 1 part of the body other than the colon, rectum or regional lymph nodes.
- M1c: Spread to the peritoneal surface.
Overall AJCC stage
| AJCC stage[2] | TNM stage[2] | TNM stage criteria[2] |
|---|---|---|
| Stage 0 | Tis N0 M0 | Tis: Tumor confined to mucosa; cancer-in-situ |
| Stage I | T1 N0 M0 | T1: Tumor invades submucosa |
| T2 N0 M0 | T2: Tumor invades muscularis propria | |
| Stage II-A | T3 N0 M0 | T3: Tumor invades subserosa or beyond (without other organs involved) |
| Stage II-B | T4a N0 M0 | T4a: Tumor perforates the visceral peritoneum |
| Stage II-C | T4b N0 M0 | T4b: Tumor invades adjacent organs |
| Stage III-A |
|
|
| Stage III-B |
|
|
| Stage III-C |
|
|
| Stage IVa | any T, any N, M1a | M1a: Metastasis to 1 other part of the body beyond the colon, rectum or regional lymph nodes. Any T, any N. |
| Stage IVb | any T, any N, M1b | M1b: Metastasis to more than 1 other part of the body beyond the colon, rectum or regional lymph nodes. Any T, any N. |
| Stage IVc | any T, any N, M1c | M1c: Metastasis to the peritoneal surface. Any T, any N. |
Dukes classification

In 1932 the British pathologist Cuthbert Dukes (1890–1977) devised a classification system for colorectal cancer.[3] Several different forms of the Dukes classification were developed.[4][5] However, this system has largely been replaced by the more detailed TNM staging system and is no longer recommended for use in clinical practice.[6]
- Dukes A: Invasion into but not through the bowel wall
- Dukes B: Invasion through the bowel wall penetrating the muscle layer but not involving lymph nodes
- Dukes C: Involvement of lymph nodes
- Dukes D: Widespread metastases[7]
Astler-Coller classification
An adaptation by the Americans Astler and Coller in 1954 further divided stages B and C[8]
- Stage A: Limited to mucosa
- Stage B1: Extending into muscularis propria but not penetrating through it; nodes not involved
- Stage B2: Penetrating through muscularis propria; nodes not involved
- Stage C1: Extending into muscularis propria but not penetrating through it. Nodes involved
- Stage C2: Penetrating through muscularis propria. Nodes involved
- Stage D: Distant metastatic spread
The stage gives valuable information for the prognosis and management of the particular cancer.
Full Dukes classification
Another modification of the original Dukes classification was made in 1935 by Gabriel, Dukes and Bussey.[9] This subdivided stage C. This staging system was noted to be prognostically relevant to rectal and colonic adenocarcinoma.[10] Stage D was added by Turnbull to denote the presence of liver and other distant metastases[11]
- Stage A: Limited to muscularis propria; nodes not involved
- Stage B: Extending beyond muscularis propria; nodes not involved
- Stage C: Nodes involved but highest (apical) node spared
- Stage D: Distant metastatic spread
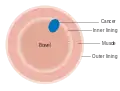 Dukes stage A bowel cancer; the cancer is only in the inner lining of the bowel.
Dukes stage A bowel cancer; the cancer is only in the inner lining of the bowel.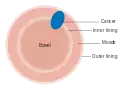 Dukes stage B bowel cancer; the cancer has invaded the muscle.
Dukes stage B bowel cancer; the cancer has invaded the muscle.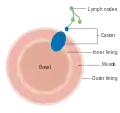 Dukes stage C bowel cancer; the cancer has invaded the nearby lymph nodes.
Dukes stage C bowel cancer; the cancer has invaded the nearby lymph nodes.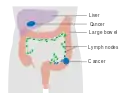 Dukes stage D bowel cancer; the cancer has metastasized.
Dukes stage D bowel cancer; the cancer has metastasized.
References
- "Cancer Staging". American Cancer Society. Retrieved 12 Sep 2020.
- "Colorectal Cancer: Stages". Cancer.net (American Society of Clinical Oncology). Retrieved 2019-09-26. Approved by the Cancer.Net Editorial Board, 11/2018. In turn citing:
Amin, Mahul B.; Greene, Frederick L.; Edge, Stephen B.; Compton, Carolyn C.; Gershenwald, Jeffrey E.; Brookland, Robert K.; Meyer, Laura; Gress, Donna M.; Byrd, David R.; Winchester, David P. (2017). "The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging". CA: A Cancer Journal for Clinicians. 67 (2): 93–99. doi:10.3322/caac.21388. ISSN 0007-9235. - Who Named It, showing correct grammatical usage
- Kyriakos M: The President cancer, the Dukes classification, and confusion, Arch Pathol Lab Med 109:1063, 1985
- Dukes CE. The classification of cancer of the rectum. Journal of Pathological Bacteriology 1932;35:323
- AJCC (American Joint Committee on Cancer) Cancer Staging Manual, 7th ed, Edge, SB, Byrd, DR, Compton, CC, et al (Eds), Springer, New York 2010. p 143.
- Single Best Answers in Surgery, Patten DK et al. Hodder Education 2009. p.107 (ISBN 9780340972359)
- Astler VB, Coller FA: The prognostic significance of direct extension of carcinoma of the colon and rectum. Ann Surg 139:846, 1954
- Gabriel WB, Dukes C, Busset HJR: Lymphatic spread in cancer of the rectum. Br J Surg 23:395–413, 1935
- Grinnell RS: The grading and prognosis of carcinoma of the colon and rectum. Ann Surg 109:500-33, 1939
- Turnbull RB Jr, Kyle K, Watson FR, et al: Cancer of the colon: the influence of the no touch isolation technique on survival rates. Ann Surg 166:420-7, 1967