Eye chart
An eye chart, or optotype, is a chart used to subjectively measure visual acuity. Eye charts are often used by health care professionals, such as optometrists, physicians or nurses, to screen persons for vision impairment. Ophthalmologists, physicians who specialize in the eye, also use eye charts to monitor the visual acuity of their patients in response to various therapies such as medications or surgery.
 Snellen chart used for visual testing. | |
| Uses | Vision testing |
|---|---|
| Related items | |
The chart is placed at a standardized distance away from the person whose vision is being tested. The person then attempts to identify the symbols on the chart, starting with the larger symbols and continuing with progressively smaller symbols until the person cannot identify the symbols. The smallest symbols that can be reliably identified is considered the person's visual acuity.
The Snellen chart is the most widely used. Alternative types of eye charts include the logMAR chart, Landolt C, E chart, Lea test, Golovin–Sivtsev table, the Rosenbaum chart, and the Jaeger chart. As previously mentioned, eye charts measure visual acuity. Eye charts do not provide doctors with information on eye diseases such as glaucoma, problems with the retina, or loss of peripheral vision.[1]
In practice, it is very important to recheck the result using Duochrome test, because it allows to refine the final sphere in refraction. It is more important to pass that test, than have perfect binocular vision in Snellen chart, especially for toric contact lenses that may behave differently from glasses. Otherwise binocular fusion may be worse that it is supposed to be.
History
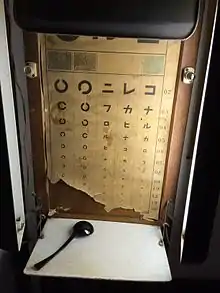
The concept of using eye glasses in order to improve eyesight has been prevalent since the late thirteenth century.[2] As science progressively improved, reputable doctors within the ophthalmology field like Cornelius Donders began to describe a clear definition as to what should be done in order to improve timeless impairments of a patient's vision. Although it slowly became clear what the procedure was in order to benefit a patient through his work, there was no uniform exam in order to prove the impairment in someone’s vision. Around this time, the knowledge within the field of ophthalmology grew immensely.[3] Previous studies led to doctors (worldwide) determining a way in which visual acuity could be examined. German eye doctor, Heinrich Kuehler proposed the first examination in order to test visual acuity.[2] Shortly after, an Austrian doctor, Eduard Jaeger created a chart which tested near vision acuity.[4] Although the general concept of the eye chart was introduced during the 1830s by doctors mentioned previously, the most effective chart to test visual acuity at the time was refined in 1862 by Dutch optometrist Herman Snellen.[5] The conception of his chart began when Snellen became Donder's first assistant.[6] Snellen worked closely with Dr. Donders as he determined vision impairments patients had by having them look at a chart on the wall. Donders eventually passed on his responsibilities to Snellen because he was very occupied with other disciplines of science like physiology.[7] Because of Donders' fame and Snellen’s natural talent towards the field of ophthalmology, many doctors were enticed to visit in order to share ideas with them in Utrecht.[7] As he worked closely through his practice, Snellen created his own chart that measured visual acuity.[8] Snellen’s eye chart became the first of its type, hence it being the most scientifically reliable design in order to test vision distance in that time period.[5] Snellen’s success within his charts was because they differed from past models that measured visual acuity. His chart varied the sizes of stimuli.[9] Snellen’s eye chart opened the door to testing visual acuity, hence it became the global standard.[10] The high demand for this chart was everywhere. Even japanese ophthalmologist Ema Tenko, who studied under Snellen, created an eye chart that was used in Japan.[11] Because of the creation of eye charts, examinations like vision screening (roughly beginning in 1899) within schools took place in order to test children’s eyes.[12] Optotype, another term that could define an eye chart, remains the most common exam in order to test standard vision.[13]
Procedure
Charts display several rows of optotypes, which are standardized symbols for testing vision. Optotypes are usually letters, numbers, or geometric symbols. Each row of the chart depicts optotypes of a different size. Typically the largest optotypes are in the top row. The optotypes become progressively smaller towards the bottom of the chart.
The person removes any glasses or contact lenses, and stands or sits a standardized distance from the chart (e.g., 20 feet for the Snellen chart).[14] The person is then asked to identify the optotypes on the chart, starting with large rows and continuing to smaller rows until the optotypes cannot be reliably identified any more. The row in which the person can reliably identify symbols defines the visual acuity.
One eye is tested at a time. Practically, this is accomplished by covering the other eye with a hand, piece of paper, or a small paddle. After testing without glasses or contact lenses, testing is repeated while the person wears them, if applicable.[15] Often, the use of such refractive lenses will correct visual acuity to normal. Refractive error can be corrected using a pinhole occluder. If the visual acuity improves with the use of pinholes, refractive lenses can be utilized to improve visual acuity. Squinting can achieve the same effect as a pinhole occluder.
With the Snellen chart, the visual acuity is recorded as a fraction with 20 in the numerator (top number) and values ranging from 10 to 600 in the denominator (bottom number). The denominator indicates the distance in feet at which a person with normal vision could stand to correctly identify the same symbols identified by the person tested. For example, a visual acuity of 20/20 is considered normal.
Variations
Numerous types of eye charts exist and are used in various situations. For example, the Snellen chart is designed for use at 6 meters or 20 feet, and is thus appropriate for testing distance vision, while the ETDRS chart is designed for use at 4 meters.[16] There is often also a need to test a subject's vision at near or occupational tasks (such as reading or computer use). For these situations, a Rosenbaum chart or Jaeger chart can be used.[17]
While the Snellen chart remains the default, some authors have argued that the logMAR chart is superior.[18] The logMAR chart presents the same number of symbols on each line, uses a typeface with letters that are equally legible at various sizes, and by varying the symbol size logarithmically, it is easier to use at nonstandard distances. As a consequence of these improvements, the logMAR chart has been proposed as a more reliable tool for measuring visual acuity.
It can be difficult to measure visual acuity in infants, young children, and illiterate adults. Special eye charts such as Lea Symbols can be used. One version uses simple pictures or patterns. Others are printed with the block letter "E" turned in different orientations, the so-called Tumbling E. The patient simply indicates which direction each "E" is facing. The Landolt C chart is similar: rows have circles with different segments missing, and the test-taker describes where each broken piece is located. The last two kinds of charts also reduce the possibility of the patient guessing the images.[19]
Parents and caregivers may test their child's eyesight from home to identify potential vision problems that require an eye care professional. Testing a child age three and older can be accomplished using the Tumbling E chart to play the "pointing game". For this test, the child sits in a chair 10 feet from the chart, gently holding an eye cover over one eye. The parent or caregiver points to each E, starting with the largest E. The child then points in the direction the E is facing (up, down, left, right). The smallest line with Es identified by the child can be recorded. The various directions the E can face should be reviewed with the child prior to home testing. Home tests are not as accurate as exams conducted by professional ophthalmologists. At home eye tests should not replace a visit to a professional eye care physician.[20][21]
Alternatives
Computer-based alternatives to the eye chart have been developed, but are not very common prior to smart phones with high display resolution and DPI becoming popular.[22] They have several potential advantages, such as a more precise measurement, less examiner-induced bias and randomized optotypes.
If the person, particularly a young child, is unable to cooperate with visual acuity testing via an eye chart, practitioners can be alerted to possible deficits in visual acuity by asking parents whether the child appears to see well. A clue is that the child may hold objects close to the face when attempting to focus.[23] Refractive error can be estimated via photography, a technique called photoscreening.[24]
Technical details
Optotype Crowding
Research has shown that optotype "crowding" reduces visual acuity at the fovea (as opposed to eccentric visual acuity) once the optotype characters are closer than 4.4 bar widths apart.[25] This is referred to as the "critical spacing" for optotype letters at the fovea. For periphery visual acuity, the critical spacing is much greater, such that optotype characters closer than 15-20 bar widths apart negatively affect visual acuity.[26]
References
- Vimont, Celia. "All About the Eye Chart". American Academy of Ophthalmology. American Academy of Ophthalmology. Retrieved 6 November 2020.
- Vogel, Wolfgang H., and Andreas Berke. Brief History of Vision and Ocular Medicine. Kugler Publications, 2009.
- Schett, A., and C. R. Keeler. The Ophthalmoscope. Wayenborgh Publishing, 2018.
- Azzam, Daniel, and Yasmyne Ronquillo. “Snellen Chart.” StatPearls, StatPearls Publishing, 2021. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK558961/.
- Rothenstein, Julian, and Mel Gooding, editors. A2Z+: Alphabets & Signs. Princeton Architectural Press, 2018.
- Schett, A., and C. R. Keeler. The Ophthalmoscope. Wayenborgh Publishing, 2018.
- Snyder, Charles. Our Ophthalmic Heritage. 1967. Little, Brown and Company.
- Vimont, Celia. “All About the Eye Chart.” American Academy of Ophthalmology, 25 Feb. 2021, https://www.aao.org/eye-health/tips-prevention/eye-chart-facts-history.
- Wade, Nicholas, and Mike Swanston. Visual Perception: An Introduction, 3rd Edition. Psychology Press, 2013.
- Goes, Frank Joseph. The Eye in History. JP Medical Ltd, 2013.
- Mishima, S. The History of Ophthalmology in Japan. Wayenborgh Publishing, 2018.
- Appelboom, Tina M. “A History of Vision Screening.” Journal of School of Health 55, no. 4 (April 1985): 138-141
- Nottingham Chaplin, P. Kay, and Geoffrey E. Bradford. “A Historical Review of Distance Vision Screening Eye Charts: What to Toss, What to Keep, and What to Replace.” NASN School Nurse, vol. 26, no. 4, July 2011, pp. 221–228, doi:10.1177/1942602X11411094.
- "Medline Plus, Visual Acuity Test".
- "All About the Eye Chart". American Academy of Ophthalmology. 2021-02-25. Retrieved 2021-10-27.
- "VALIDITY OF OUTCOME MEASURES".
- "Home vision tests: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2015-05-09.
- Hussain, Badrul; Saleh, George M; Sivaprasad, Sobha; Hammond, Christopher J (2006). "Changing from Snellen to LogMAR: debate or delay?". Clinical and Experimental Ophthalmology. 34 (1): 6–8. doi:10.1111/j.1442-9071.2006.01135.x. PMID 16451251.
- "Vision screening in infants, children and youth". Paediatrics & Child Health. 14 (4): 246–248. April 2009. doi:10.1093/pch/14.4.246. ISSN 1205-7088. PMC 2690539. PMID 20357924.
- "What Is a Visual Acuity Test?". Optometrists Network. Optometrists Network. Retrieved 6 November 2020.
- Repka, Michael. "Home Eye Test for Children and Adults". American Academy of Ophthalmology. American Academy of Ophthalmology. Retrieved 6 November 2020.
- Claessens, Janneau L. J.; Geuvers, Judith R.; Imhof, Saskia M.; Wisse, Robert P. L. (2021-06-25). "Digital Tools for the Self-Assessment of Visual Acuity: A Systematic Review". Ophthalmology and Therapy. doi:10.1007/s40123-021-00360-3. ISSN 2193-8245. PMC 8225487. PMID 34169468.
- Hagan, JF (2008). Futures: Guidelines for Health Supervision. Elk Grove.
- "Photoscreening – EyeWiki". eyewiki.aao.org. Retrieved 2015-05-09.
- "Amblyopia - EyeWiki". eyewiki.aao.org. Retrieved 2019-05-20.
- Coates, D. R; Chin, J. M; Chung, S. T (2013). "Factors Affecting Crowded Acuity: Eccentricity and Contrast". Optometry and Vision Science. 90 (7): 628–638. doi:10.1097/OPX.0b013e31829908a4. PMC 3837536. PMID 23770657.