Fall prevention
Fall prevention includes any action taken to help reduce the number of accidental falls suffered by susceptible individuals, such as the elderly (idiopathic) and people with neurological (Parkinson's, Multiple sclerosis, stroke survivors, Guillain-Barre, traumatic brain injury, incomplete spinal cord injury) or orthopedic (lower limb or spinal column fractures or arthritis, post-surgery, joint replacement, lower limb amputation, soft tissue injuries) indications.
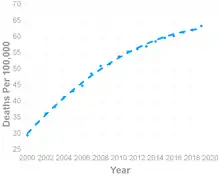
Current approaches to fall prevention are problematic because even though awareness is high among professionals that work with seniors and fall prevention activities are pervasive among community living establishments,[1] fall death rates among older adults have more than doubled.[2] The challenges are believed to be three-fold. First, insufficient evidence exists that any fall risk screening instrument is adequate for predicting falls.[3] While the strongest predictors of fall risk tend to include a history of falls during the past year, gait, and balance abnormalities,[4] existing models show a strong bias and therefore mostly fail to differentiate between adults that are at low risk and high risk of falling.[5][6]
Second, current fall prevention interventions in the United States are limited between short-term individualized therapy provided by a high-cost physical therapist or longer-term wellness activity provided in a low-cost group setting. Neither arrangement is optimum in preventing falls over a large population,[7] especially as these evidence-based physical exercise programs have limited effectiveness[8] (approximately 25%). Even multifactorial interventions,[9] which include extensive physical exercise, medication adjustment, and environmental modification only lower fall risk by 31% after 12 months.[10] Questions around effectiveness of current approaches (physical exercise and multifactorial interventions) have been found in multiple settings, including long-term care facilities and hospitals.[11]
The final challenge is adherence. Average adherence in group-based fall prevention exercise programs is around 66%, mostly due to the highly repetitive nature of the programs and the extremely long duration required for noticeable benefits accrue.[12] Adherence to physical therapy can be even lower.[13] When adherence is below 70%, effectiveness of fall prevention physical exercise programs can drop to less than 10%.[12]
Practitioners are aware that the most successful approach to fall prevention utilizes a multimodal, motor-cognitive training approach[14] that could be introduced to all adults over 65. The scientific basis of this approach is an understanding of how the dual-task paradigm induces neuroplasticity in the brain, especially in aging populations.[15] This is driving a growing body of research that specifically links the cognitive sub-domains of attention and executive function (EF) to gait alterations and fall risk.[16][17][18][19][20]
Cost of falls
Falls and fall-related injuries are among the most common but serious medical problems experienced by older adults. Nearly one-third of older people fall each year, half of which fall more than once per year.[21] Over 3 million Americans over the age of 65 visited hospital emergency departments in 2015 due to fall-related injuries, with over 1.6 million being admitted.[22] Because of decreased bone density due to osteoporosis, mobility, and reflexes, falls often result in hip fractures and other fractures, head injuries, and death in older adults. Accidental injuries are the fifth most common cause of death in older adults.[21] 75% of hip fracture patients do not recover completely and show signs of overall health deterioration.[21]
Strategies and interventions
Motor-cognitive training is increasingly viewed as the gold standard for healthy aging and fall prevention.[23][24] One approach that has been researched is the introduction of semi-immersive virtual reality simulation during treadmill training.[25] Initially conceptualized by the Tel Aviv Sourasky Medical Center with funding from the Michael J Fox Foundation and the European Commission, V-TIME[26] projects a real-time image of participants' feet onto a large screen at eye-level while the participants are walking on a treadmill. The virtual environment introduces multiple physical and cognitive challenges while the participant is in dynamic motion. This one approach to motor-cognitive training was found to repeatedly reduce falls by 50%[27] after 5 weeks of 15 sessions across multiple clinical trials and multiple indications (idiopathic,[28] Parkinson's,[29] Multiple sclerosis[30]). The biological manifestations of this improvement were identified through functional MRI, which showed changes in brain activity patterns for patients that were exposed to combined motor-cognitive training, as opposed to exclusively physical training.[31]
Other preventative measures with positive effects include strength and balance training, home risk assessment,[32] the withdrawal of psychotropic medication, cardiac pacing for those with carotid sinus hypersensitivity, and tai chi. Resistance exercise two or three times a week with ankle weights or elastic bands has been proven in tests to rebuild lost muscle mass and reduce falls in adults of all ages: it was first tested in New Zealand by the Otago Medical School in four controlled trials, in which about 1,000 older adults with an average age 84 participated. Falls among a test group that did the Otago routines three times a week for 12 months was 35% fewer than a control group that did not use the routines.[33] Two similar 12-month tests were conducted in the US using residents in assisted and skilled nursing facilities with one group showing a 54% reduction in falls.[34] After the age of 50, adults experience a decrease in muscle mass (sarcopenia) by approximately 2% every year.[35] A systematic review concluded that resistance training can slow down the rate of loss in muscle mass and strength. It has been recommended that older adults participate in resistance training two to three times a week to weaken the effects of sarcopenia.[35] Assistive technology can also be applied, although it is mostly reactive in case of a fall.[36] Exercise as a single intervention has been shown to prevent falls in community-dwelling older adults. A systematic review suggests that having an exercise regimen that includes challenging balance workouts for three or more hours per week results in a lesser chance of falling.[35] Resistance training has been shown to be beneficial beyond fall prevention, as it also helps improve functional mobility and activities of daily living such as walking endurance, gait speed, and stair climbing.[35] Research explains that this significant increase in performance can be accomplished after the age of 90. For older adults to gain confidence in resistance training, which may ultimately lead to falling prevention effects, they must obtain the recommended amount of daily activity.[35]
The aim of medical management is to identify factors that can contribute to falls and fracture risk such as osteoporosis, multiple medications, balance and gait problems, loss of vision and a history of falls. Beers Criteria is a list of medications that are potentially inappropriate for use in the elderly and some of them increase the risk of falls.[37]
Falls are well known amongst community-dwelling individuals ages 65 and older.[38] The risk of fall-related incidents nearly doubles when individuals are institutionalized.[39] The impact on different falls in certain situation of fall prevention programs on the rate differences of falls in elderly population has not been reported. As well as cognitive impairment, functional impairment, gait, and balance disorders, certain medications can increase fall risk factors for patients. At an advanced age, these risk factors are double and more likely to occur. It's important to identify the risk factors that increase the likelihood of injurious falls. State-level fall prevention strategies can also mitigate fall risk for community-dwelling older adults.[38]
Risk factors of falls
Older adults
Studies have shown that adults over the age of 65 are more prone to falls than younger, healthy adults.[40][41] Most falls in older adults are due to:[42]
- Gait deviations – These are the main changes that occur in the gait patterns of older adults, which may contribute to the incidence of falls. Older adults may experience a 10–20% reduction in gait velocity and reduction in stride length, an increase in stance width and double support phase, or a bent posture.[43][44][45] Studies show that a wider stride does not necessarily increase stability, and may instead increase the likelihood of experiencing falls.[46]
- Limitations in mobility – Loss of mobility increases the risk of falls in situations which, under normal circumstances, would pose a low risk of falling (such as walking up/down stairs).[47]
- Reduced muscle strength, especially in the lower body, which leads to difficulties standing up.[48][49]
- Poor reaction time – Aging is associated with the gradual slowing of an individual's reaction time.[50]
- Accidents/environmental factors – Falls may occur due to dangerous or unstable surfaces, such as wet surfaces, ice, stairs, or rugs; or inappropriate footwear.
- Balance disorders – vertigo, syncope, unsteadiness, ataxias
- Visual, sensory, motor, and cognitive impairment
- Medications and alcohol consumption – Dizziness, drowsiness and confusion can occur as side effects of some medications. Alcohol consumption causes a delay in reflexes and diminishes balance and fine motor control via its inhibitory effects on nerve pathways in the cerebellum.[51]
- Acute and chronic infections
- Dehydration
Stroke
Individuals who have had a stroke have higher fall rates. Approximately 30% fall at least once a year and 15% fall twice or more.[52] Risk factors for falls in stroke survivors are:[53]
- Gait deviations – Disturbance of gait is a common problem post-stroke and a common contributor of falls, predicting a continual functional decline. Velocity, cadence, stride time, stride length, and temporal symmetry index are reduced and result in significant gait deterioration.[54] Reduced propulsion at push-off, decreased leg flexion during the swing phase, reduced stability during the stance phase, and reduced automaticity of walking occur.[52]
- Reduced muscle tone and weakness
- Side effects of drugs
- Hypoglycemia
- Hypotension
- Communication disorders
- Hemianopia
- Visuospatial agnosia
Parkinson's disease
Most people with Parkinson's disease (PD) fall and many experience recurrent falls.[55] A study reported that over 50% of persons with PD fell recurrently.[56] Direct and indirect causes of falls in patients with PD:[57]
- Gait deviations – Decreased gait velocity and stride length due to hypokinetic movement, decreased cadence due to bradykinetic movements. Affected individuals also exhibit flat foot strike.
- Sudden falls
- Freezing and festination episodes
- Postural instability
- Intensified dyskinesia
- Autonomic system disorders – orthostatic hypotension, neurocardiogenic syncope, postural orthostatic tachycardia syndrome
- Neurological and sensory disturbances – muscle weakness of lower limbs, deep sensibility impairment, epileptic seizure, cognitive impairment, visual impairment, balance impairment
- Cardiovascular disease
- Drugs
Multiple sclerosis
There is a high prevalence of falls among persons with multiple sclerosis (MS), with approximately 50% reporting a fall within the past six months.[58] About 30% of those individuals report falling multiple times.
- Gait deviations – Gait variability is elevated in individuals with MS.[59] Stride length, cadence, and velocity decrease, while stance duration and cycle duration increase.[60]
- Foot drop
- Ataxia – vestibular ataxia results in loss of balance. Symptoms are exacerbated when the eyes are closed and the base of support is reduced.
- Reduced proprioception
- Improper or reduced use of assistive devices[61]
- Vision – blurred vision, double vision, loss of peripheral vision
- Cognitive changes – Approximately 50% of affected individuals experience difficulty with their cognition over the course of the disease, which affects planning, organizing, problem-solving, and the ability to accurately perceive the environment. When these problems interfere with walking, it may result in a fall.
- Neurological medications – causes fatigue,[62] weakness, dizziness
Dementia
Studies suggest that men are twice as likely to fall as women.[63] Common causes of falls in dementia include:
- Gait deviations – Slower walking speed, reduced cadence, and step length, increased postural flexion, increased double support time[64]
- Postural instability – Gait changes and impaired balance. People with balance deficits are at more risk of falling than those with a normal gait and intact balance.
- Lack of physical exercise
- Visual impairment - Blurry vision, low vision, and loss of peripheral vision. Eyesight cannot be fixed or corrected by glasses.
- Fatigue
- Medications – psychotropic drugs have effects on balance, reaction time and other sensorimotor functions, orthostatic hypotension, and extrapyramidal symptoms.
Fear of falling (basophobia)
Basophobia is a term used in many circumstances to describe the fear of falling in either normal or special situations. It refers to uncomfortable sensations that may be experienced by older people. These sensations can include lower-body weakness or loss of balance, which can induce a frightening sensation of falling that can lead to serious and potentially fatal injuries.[65]
Healthy young individuals
Accidents are the most common cause of falls involving healthy adults, which may be the result of tripping on stairs, improper footwear, dark surroundings, slippery surfaces, uneven ground, or lack of exercise. Studies suggest that women are more prone to falling than men in all age groups.[66] The most common injuries among younger patientd occur in the hands, wrists, knees, and ankles.[66]
Environmental modification





The home environment can present many hazards. Common places for injurious falls include the bathtub and stairs. Changes to the home environment are aimed at reducing hazards and help support a person in daily activities; they include minimizing clutter, installing grab bars in the bathroom, and installing non-slip decals to slippery surfaces.[67] Stairs can be improved by installing handrails on both sides, improving lighting, and adding colour contrast between steps. Improvement in lighting and luminance levels can aid elderly people in assessing and negotiating hazards. Occupational therapists can help clients improve fall prevention behaviours.[68] In addition, they can instruct clients and their family members on factors that contribute to falls, and implement environmental modifications and strategies to decrease the risk of falls.[68] There is currently insufficient scientific evidence to ensure the effectiveness of modification of the home environment to reduce injuries.[69] Evidence suggests that pre-discharge home assessments are associated with a reduced risk of falling.[32]
Safety technology
Important improvements to prevent falls include handrails and grab bars, which should be easy to grip or grasp and should be near any stairs or change in floor level. Floors should always be flat and level, with no exposed corners or edges. Patterned floors can be dangerous if they create misleading or distorted images of the floor surface, and should be avoided.[70]
There are special handles and closed handgrips available in bathrooms and lavatories to help users bend down or over. For example, extra support for users when moving include walking sticks, crutches, and support frames, such as a walker. Flexible handles such as hanging straps can also be useful supports.[71]
Eyeglasses selection and usage
Bifocal spectacles and trifocal eyeglasses are used to provide refractory correction ideal for reading (12–24 inches (30–60 cm) when the wearer looks downward through them. Reading glasses are not ideal for safe walking, where correction for 4.5–5 feet (137–152 cm) would be more appropriate.
Occupational and physical therapy
Studies show that balance, flexibility, strength, and motor-cognitive training not only improve mobility but also reduce the risk of falling. This may be achieved through group and home-based exercise programs or engagement with physical therapy clinics with the appropriate equipment. The majority of older adults do not exercise regularly and 35% of people over the age of 65 do not participate in any leisurely physical activities.
Older adults
In older adults, physical training and perturbation therapy is directed to improving balance recovery responses and preventing falls.[72] Gait-related changes in the elderly provide a greater chance of stability during walking due to slower speed and greater base of support, but they also increase the chance of slipping or tripping and falling.[73] Appropriate joint moment generation is required to create sufficient push-off for balance recovery. Age-related changes in muscles, tendons, and neural structures may contribute to slower reactive responses. Interventions involving resistance training along with perturbation training may prove to be beneficial in improving muscle strength and balance recovery.[74]
Stroke recovery
Stroke exercises help patients regain mobility and strength in their bodies, and must be done regularly in order to regain muscle tone that helps prevent falls.[75]
Exercises for prevention
One of the most important things for fall prevention in elderly populations is to stay physically fit. Specialized facilities and programs like seniors' parks are a good place to keep the elderly in shape and increase their resistance to falling. These facilities contain specialized equipment and training stations where elderly people can exercise. The parks usually have an extended amount of space and different stages reserved for different body exercises. Research suggests that participation in such programs successfully mitigates fall risk in the majority of attendees.[76]
See also
- Morse Fall Scale
- Falling (accident)
- Falls in older adults
- Fall Prevention Center of Excellence
- Light ergonomics
- Lighting for the elderly
- Safety engineering
- Safety equipment
- Home modifications
- Home automation for elderly and disabled people
- Assisted living
- Assistive technology
References
- Harris-Kojetin, L; Sengupta, M (2018-11-11). "Falls Among Assisted Living Residents: Results from the 2016 National Study of Long-Term Care Providers". Innovation in Aging. 2 (Suppl 1): 766. doi:10.1093/geroni/igy023.2833. ISSN 2399-5300. PMC 6228283.
- "Important Facts about Falls | Home and Recreational Safety | CDC Injury Center". www.cdc.gov. 2019-02-01. Retrieved 2021-12-02.
- Gates, Simon; Smith, Lesley A.; Fisher, Joanne D.; Lamb, Sarah E. (2008). "Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults". Journal of Rehabilitation Research and Development. 45 (8): 1105–1116. doi:10.1682/JRRD.2008.04.0057. ISSN 1938-1352. PMID 19235113.
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ (January 2007). "Will my patient fall?". JAMA. 297 (1): 77–86. doi:10.1001/jama.297.1.77. PMID 17200478.
- Park, Seong-Hi (January 2018). "Tools for assessing fall risk in the elderly: a systematic review and meta-analysis". Aging Clinical and Experimental Research. 30 (1): 1–16. doi:10.1007/s40520-017-0749-0. ISSN 1720-8319. PMID 28374345. S2CID 24579938.
- Gade, Gustav Valentin; Jørgensen, Martin Grønbech; Ryg, Jesper; Riis, Johannes; Thomsen, Katja; Masud, Tahir; Andersen, Stig (2021-05-04). "Predicting falls in community-dwelling older adults: a systematic review of prognostic models". BMJ Open. 11 (5): e044170. doi:10.1136/bmjopen-2020-044170. ISSN 2044-6055. PMC 8098967. PMID 33947733.
- Gillespie, LD; Gillespie, WJ; Robertson, MC; Lamb, SE; Cumming, RG; Rowe, BH (December 2003). "Interventions for preventing falls in elderly people". Physiotherapy. 89 (12): 692–693. doi:10.1016/s0031-9406(05)60487-7. ISSN 0031-9406.
- Sherrington, Catherine; Fairhall, Nicola; Kwok, Wing; Wallbank, Geraldine; Tiedemann, Anne; Michaleff, Zoe A.; Ng, Christopher A. C. M.; Bauman, Adrian (2020-11-26). "Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour". The International Journal of Behavioral Nutrition and Physical Activity. 17 (1): 144. doi:10.1186/s12966-020-01041-3. ISSN 1479-5868. PMC 7689963. PMID 33239019.
- Mahoney, Jane E. (2010-07-12). "Why Multifactorial Fall-Prevention Interventions May Not Work". Archives of Internal Medicine. 170 (13): 1117–1119. doi:10.1001/archinternmed.2010.193. ISSN 0003-9926. PMID 20625016.
- Tinetti, Mary E.; Baker, Dorothy I.; McAvay, Gail; Claus, Elizabeth B.; Garrett, Patricia; Gottschalk, Margaret; Koch, Marie L.; Trainor, Kathryn; Horwitz, Ralph I. (1994-09-29). "A Multifactorial Intervention to Reduce the Risk of Falling among Elderly People Living in the Community". New England Journal of Medicine. 331 (13): 821–827. doi:10.1056/NEJM199409293311301. ISSN 0028-4793. PMID 8078528.
- Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N (September 2018). "Interventions for preventing falls in older people in care facilities and hospitals". The Cochrane Database of Systematic Reviews. 9: CD005465. doi:10.1002/14651858.CD005465.pub4. PMC 6148705. PMID 30191554.
- Osho, Oluwaseyi; Owoeye, Oluwatoyosi; Armijo-Olivo, Susan (2018-04-01). "Adherence and Attrition in Fall Prevention Exercise Programs for Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis". Journal of Aging and Physical Activity. 26 (2): 304–326. doi:10.1123/japa.2016-0326. ISSN 1543-267X. PMID 28771111.
- R, Salazar (2019). "2019 Survey Results: Outpatient PT & OT Clinicians & Clinic Owners". Retrieved June 2, 2020.
{{cite web}}: CS1 maint: url-status (link) - Mirelman A, Rochester L, Maidan I, Del Din S, Alcock L, Nieuwhof F, et al. (September 2016). "Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): a randomised controlled trial" (PDF). Lancet. 388 (10050): 1170–82. doi:10.1016/S0140-6736(16)31325-3. PMID 27524393. S2CID 15303981. Archived from the original (PDF) on 2021-07-14. Retrieved 2021-07-14.
- Raichlen DA, Alexander GE (1 January 2020). "Why Your Brain Needs Exercise". Scientific American.
- Hausdorff, Jeffrey M.; Doniger, Glen M.; Springer, Shmuel; Yogev, Galit; Simon, Ely S.; Giladi, Nir (December 2006). "A Common Cognitive Profile in Elderly Fallers and in Patients with Parkinson's Disease: The Prominence of Impaired Executive Function and Attention". Experimental Aging Research. 32 (4): 411–429. doi:10.1080/03610730600875817. ISSN 0361-073X. PMC 1868891. PMID 16982571.
- Mayor, Susan (2016-02-04). "Parkinson's disease diagnosis is preceded by increased risk of falls, study finds". BMJ. 352: i695. doi:10.1136/bmj.i695. ISSN 1756-1833. PMID 26849893. S2CID 40522797.
- Herman, Talia; Mirelman, Anat; Giladi, Nir; Schweiger, Avraham; Hausdorff, Jeffrey M. (2010-05-19). "Executive Control Deficits as a Prodrome to Falls in Healthy Older Adults: A Prospective Study Linking Thinking, Walking, and Falling". The Journals of Gerontology: Series A. 65A (10): 1086–1092. doi:10.1093/gerona/glq077. ISSN 1758-535X. PMC 2949331. PMID 20484336.
- Holtzer, Roee; Friedman, Rachel; Lipton, Richard B.; Katz, Mindy; Xue, Xiaonan; Verghese, Joe (2007). "The relationship between specific cognitive functions and falls in aging". Neuropsychology. 21 (5): 540–548. doi:10.1037/0894-4105.21.5.540. ISSN 1931-1559. PMC 3476056. PMID 17784802.
- Springer, Shmuel; Giladi, Nir; Peretz, Chava; Yogev, Galit; Simon, Ely S.; Hausdorff, Jeffrey M. (2006-03-15). "Dual-tasking effects on gait variability: The role of aging, falls, and executive function". Movement Disorders. 21 (7): 950–957. doi:10.1002/mds.20848. ISSN 0885-3185. PMID 16541455. S2CID 34812135.
- Moylan KC, Binder EF (June 2007). "Falls in older adults: risk assessment, management and prevention". The American Journal of Medicine. 120 (6): 493.e1–6. doi:10.1016/j.amjmed.2006.07.022. PMID 17524747.
- Centers for Disease Control and Prevention. "Non-fatal injury report". WISQARS database. US Government. Archived from the original on 6 March 2018. Retrieved 2 December 2017.
- Herold, Fabian; Hamacher, Dennis; Schega, Lutz; Müller, Notger G. (2018). "Thinking While Moving or Moving While Thinking – Concepts of Motor-Cognitive Training for Cognitive Performance Enhancement". Frontiers in Aging Neuroscience. 10: 228. doi:10.3389/fnagi.2018.00228. ISSN 1663-4365. PMC 6089337. PMID 30127732.
- Chung, Seok Jong; Lee, Jae Jung; Lee, Phil Hyu; Sohn, Young H. (2020). "Emerging Concepts of Motor Reserve in Parkinson's Disease". Journal of Movement Disorders. 13 (3): 171–184. doi:10.14802/jmd.20029. PMC 7502292. PMID 32854486.
- Rapaport L (18 August 2016). "Virtual reality treadmills help prevent falls in elderly". Reuters. Archived from the original on 29 October 2018. Retrieved 6 January 2021.
- Mirelman, Anat; Rochester, Lynn; Reelick, Miriam; Nieuwhof, Freek; Pelosin, Elisa; Abbruzzese, Giovanni; Dockx, Kim; Nieuwboer, Alice; Hausdorff, Jeffrey M (2013-02-06). "V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomized controlled trial". BMC Neurology. 13 (1): 15. doi:10.1186/1471-2377-13-15. ISSN 1471-2377. PMC 3602099. PMID 23388087.
- Mirelman, Anat; Rochester, Lynn; Maidan, Inbal; Del Din, Silvia; Alcock, Lisa; Nieuwhof, Freek; Rikkert, Marcel Olde; Bloem, Bastiaan R; Pelosin, Elisa; Avanzino, Laura; Abbruzzese, Giovanni (September 2016). "Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): a randomised controlled trial". The Lancet. 388 (10050): 1170–1182. doi:10.1016/s0140-6736(16)31325-3. ISSN 0140-6736. PMID 27524393. S2CID 15303981.
- Del Din, Silvia; Galna, Brook; Lord, Sue; Nieuwboer, Alice; Bekkers, Esther M. J.; Pelosin, Elisa; Avanzino, Laura; Bloem, Bastiaan R.; Olde Rikkert, Marcel G. M.; Nieuwhof, Freek; Cereatti, Andrea (2020-05-22). "Falls Risk in Relation to Activity Exposure in High-Risk Older Adults". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 75 (6): 1198–1205. doi:10.1093/gerona/glaa007. ISSN 1758-535X. PMC 7243591. PMID 31942969.
- Pelosin, Elisa; Cerulli, Cecilia; Ogliastro, Carla; Lagravinese, Giovanna; Mori, Laura; Bonassi, Gaia; Mirelman, Anat; Hausdorff, Jeffrey M; Abbruzzese, Giovanni; Marchese, Roberta; Avanzino, Laura (2019-03-15). "A Multimodal Training Modulates Short Afferent Inhibition and Improves Complex Walking in a Cohort of Faller Older Adults With an Increased Prevalence of Parkinson's Disease". The Journals of Gerontology: Series A. 75 (4): 722–728. doi:10.1093/gerona/glz072. ISSN 1079-5006. PMID 30874799.
- Peruzzi, Agnese; Cereatti, Andrea; Della Croce, Ugo; Mirelman, Anat (January 2016). "Effects of a virtual reality and treadmill training on gait of subjects with multiple sclerosis: a pilot study". Multiple Sclerosis and Related Disorders. 5: 91–96. doi:10.1016/j.msard.2015.11.002. ISSN 2211-0348. PMID 26856951.
- Siegel-Itzkovich J (31 October 2017). "Sourasky researchers explain how virtual reality helps prevent falls by Parkinson's patients". The Jerusalem Post. Archived from the original on 27 December 2020. Retrieved 6 January 2021.
- Lockwood KJ, Taylor NF, Harding KE (April 2015). "Pre-discharge home assessment visits in assisting patients' return to community living: A systematic review and meta-analysis". Journal of Rehabilitation Medicine. 47 (4): 289–99. doi:10.2340/16501977-1942. PMID 25782842.
- Campbell AJ, Robertson MC (March 2003). Otago Exercise Programme to prevent falls in older adults (PDF). Otago Medical School. p. 3. ISBN 978-0-478-25194-4. Archived (PDF) from the original on 2021-01-20. Retrieved 2020-12-27.
- "Upgraded SNF restorative program reduces falls". I Advance Senior Care. 28 July 2015. Archived from the original on 13 August 2020. Retrieved 27 December 2020.
- Papa EV, Dong X, Hassan M (13 June 2017). "Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review". Clinical Interventions in Aging. 12: 955–961. doi:10.2147/CIA.S104674. PMC 5479297. PMID 28670114.
- Hill KD, Suttanon P, Lin SI, Tsang WW, Ashari A, Hamid TA, et al. (January 2018). "What works in falls prevention in Asia: a systematic review and meta-analysis of randomized controlled trials". BMC Geriatrics. 18 (1): 3. doi:10.1186/s12877-017-0683-1. PMC 5756346. PMID 29304749.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH (8 December 2003). "Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts". Archives of Internal Medicine. 163 (22): 2716–24. doi:10.1001/archinte.163.22.2716. PMID 14662625.
- "State of Safety: A State-by-State Report". National Safety Council. 2021. Archived from the original on 2021-06-04. Retrieved 2020-12-27.
- dos Reis KM, de Jesus CA (December 2015). "Cohort study of institutionalized elderly people: fall risk factors from the nursing diagnosis". Revista Latino-Americana de Enfermagem. 23 (6): 1130–8. doi:10.1590/0104-1169.0285.2658. PMC 4664014. PMID 26626005.
- Gillespie L (February 2013). Tovey D (ed.). "Preventing falls in older people: the story of a Cochrane review". The Cochrane Database of Systematic Reviews (2): ED000053. doi:10.1002/14651858.ED000053. PMID 23543586.
- Yoshikawa TT, Cobbs EL, Brummel-Smith K (1993). Ambulatory Geriatric Care. Mosby. ISBN 978-0-8016-6543-1.
- O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S (February 1993). "Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly". American Journal of Epidemiology. 137 (3): 342–54. doi:10.1093/oxfordjournals.aje.a116681. PMID 8452142.
- Winter DA, Patla AE, Frank JS, Walt SE (June 1990). "Biomechanical walking pattern changes in the fit and healthy elderly". Physical Therapy. 70 (6): 340–7. doi:10.1093/ptj/70.6.340. PMID 2345777.
- Elble RJ, Thomas SS, Higgins C, Colliver J (February 1991). "Stride-dependent changes in gait of older people". Journal of Neurology. 238 (1): 1–5. doi:10.1007/BF00319700. PMID 2030366. S2CID 20197857.
- Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR (January 2007). "Neurological gait disorders in elderly people: clinical approach and classification". The Lancet. Neurology. 6 (1): 63–74. doi:10.1016/S1474-4422(06)70678-0. PMID 17166803. S2CID 31984607.
- Maki BE (March 1997). "Gait changes in older adults: predictors of falls or indicators of fear". Journal of the American Geriatrics Society. 45 (3): 313–20. doi:10.1111/j.1532-5415.1997.tb00946.x. PMID 9063277. S2CID 31970427.
- Musich S, Wang SS, Ruiz J, Hawkins K, Wicker E (March 2018). "The impact of mobility limitations on health outcomes among older adults". Geriatric Nursing. 39 (2): 162–169. doi:10.1016/j.gerinurse.2017.08.002. PMID 28866316. S2CID 3981042.
- Chatzistergos, Panagiotis E.; Healy, Aoife; Balasubramanian, Gayathri; Sundar, Lakshmi; Ramachandran, Ambady; Chockalingam, Nachiappan (September 2020). "Reliability and validity of an enhanced paper grip test; A simple clinical test for assessing lower limb strength" (PDF). Gait & Posture. 81: 120–125. doi:10.1016/j.gaitpost.2020.07.011. PMID 32711330. S2CID 220773361.
- "Falls". Medline Plus. U.S. National Library of Medicine. Archived from the original on 2021-01-09. Retrieved 2020-12-27.
- "Caídas en personas mayores: riesgo, causas y prevención" [Falls in the elderly: risks, causes and prevention]. Geriatricarea (in Spanish). 16 March 2016. Archived from the original on 24 October 2020. Retrieved 3 December 2020.
- Edith, Sullivan; Margaret, Rosenbloom; Anjali, Deshmukh; John, Desmond; Adolf, Pfefferbaum (1995). "Alcohol and the cerebellum". Alcohol Health and Research World. 19 (2): 138–141. PMC 6875723. PMID 31798074.
- Weerdesteyn V, de Niet M, van Duijnhoven HJ, Geurts AC (2008). "Falls in individuals with stroke". Journal of Rehabilitation Research and Development. 45 (8): 1195–213. doi:10.1682/JRRD.2007.09.0145. hdl:2066/70270. PMID 19235120. ProQuest 215286948.
- Tsur A, Segal Z (April 2010). "Falls in stroke patients: risk factors and risk management". The Israel Medical Association Journal. 12 (4): 216–9. PMID 20803880.
- Yang YR, Chen YC, Lee CS, Cheng SJ, Wang RY (February 2007). "Dual-task-related gait changes in individuals with stroke". Gait & Posture. 25 (2): 185–90. doi:10.1016/j.gaitpost.2006.03.007. PMID 16650766.
- Allen NE, Schwarzel AK, Canning CG (5 March 2013). "Recurrent falls in Parkinson's disease: a systematic review". Parkinson's Disease. 2013: 906274. doi:10.1155/2013/906274. PMC 3606768. PMID 23533953.
- Wood BH, Bilclough JA, Bowron A, Walker RW (June 2002). "Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study". Journal of Neurology, Neurosurgery, and Psychiatry. 72 (6): 721–5. doi:10.1136/jnnp.72.6.721. PMC 1737913. PMID 12023412. S2CID 18378056.
- Koller WC, Silver DE, Lieberman A (December 1994). "An algorithm for the management of Parkinson's disease". Neurology. 44 (12 Suppl 10): S1-52. PMID 7854513.
- Finlayson ML, Peterson EW, Cho CC (September 2006). "Risk factors for falling among people aged 45 to 90 years with multiple sclerosis". Archives of Physical Medicine and Rehabilitation. 87 (9): 1274–9, quiz 1287. doi:10.1016/j.apmr.2006.06.002. PMID 16935067.
- Socie MJ, Sosnoff JJ (2013). "Gait variability and multiple sclerosis". Multiple Sclerosis International. 2013: 645197. doi:10.1155/2013/645197. PMC 3603667. PMID 23533759.
- Severini G, Manca M, Ferraresi G, Caniatti LM, Cosma M, Baldasso F, et al. (June 2017). "Evaluation of Clinical Gait Analysis parameters in patients affected by Multiple Sclerosis: Analysis of kinematics". Clinical Biomechanics. 45: 1–8. doi:10.1016/j.clinbiomech.2017.04.001. PMID 28390935. S2CID 24378620.
- Cattaneo D, De Nuzzo C, Fascia T, Macalli M, Pisoni I, Cardini R (June 2002). "Risks of falls in subjects with multiple sclerosis". Archives of Physical Medicine and Rehabilitation. 83 (6): 864–7. doi:10.1053/apmr.2002.32825. PMID 12048669.
- Krupp LB, Christodoulou C (May 2001). "Fatigue in multiple sclerosis". Current Neurology and Neuroscience Reports. 1 (3): 294–8. doi:10.1007/s11910-001-0033-7. PMID 11898532. S2CID 28222172.
- van Dijk PT, Meulenberg OG, van de Sande HJ, Habbema JD (April 1993). "Falls in dementia patients". The Gerontologist. 33 (2): 200–4. doi:10.1093/geront/33.2.200. PMID 8468012.
- Shaw FE (2003). "Falls in older people with dementia" (PDF). Great Aging. 6 (7): 37–40. Archived (PDF) from the original on 2020-12-05. Retrieved 2020-12-27.
- Olesen J (10 February 2014). "Fear of Falling Phobia - Basiphobia". FEAROF.NET. Archived from the original on 30 November 2020. Retrieved 3 December 2020.
- Talbot LA, Musiol RJ, Witham EK, Metter EJ (August 2005). "Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury". BMC Public Health. 5 (1): 86. doi:10.1186/1471-2458-5-86. PMC 1208908. PMID 16109159.
- Lin JT, Lane JM (January 2008). "Nonpharmacologic management of osteoporosis to minimize fracture risk". Nature Clinical Practice. Rheumatology. 4 (1): 20–5. doi:10.1038/ncprheum0702. PMID 18172445. S2CID 24451002.
- Howard B, Baca R, Bilger M, Cali S, Kotarski A, Parrett K, Skibinski K (2018-07-03). "Investigating Older Adults' Expressed Needs Regarding Falls Prevention". Physical & Occupational Therapy in Geriatrics. 36 (2–3): 201–220. doi:10.1080/02703181.2018.1520380. ISSN 0270-3181. S2CID 81971080.
- Turner S, Arthur G, Lyons RA, Weightman AL, Mann MK, Jones SJ, et al. (February 2011). "Modification of the home environment for the reduction of injuries". The Cochrane Database of Systematic Reviews (2): CD003600. doi:10.1002/14651858.CD003600.pub3. PMC 7003565. PMID 21328262.
- McKinney R (26 March 2020). "Exciting Advancements in Fall Prevention Technology". Safesite. Archived from the original on 26 November 2020. Retrieved 3 December 2020.
- "Prevent Accidents in the Bathroom with These Toilet Safety Rails". AgingInPlace.org. 4 December 2018. Archived from the original on 27 January 2021. Retrieved 3 December 2020.
- Gerards MH, McCrum C, Mansfield A, Meijer K (December 2017). "Perturbation-based balance training for falls reduction among older adults: Current evidence and implications for clinical practice". Geriatrics & Gerontology International. 17 (12): 2294–2303. doi:10.1111/ggi.13082. PMC 5763315. PMID 28621015.
- Pijnappels M, Reeves ND, Maganaris CN, van Dieën JH (April 2008). "Tripping without falling; lower limb strength, a limitation for balance recovery and a target for training in the elderly". Journal of Electromyography and Kinesiology. 18 (2): 188–96. doi:10.1016/j.jelekin.2007.06.004. PMID 17761436.
- Larsson L, Degens H, Li M, Salviati L, Lee YI, Thompson W, et al. (January 2019). "Sarcopenia: Aging-Related Loss of Muscle Mass and Function". Physiological Reviews. 99 (1): 427–511. doi:10.1152/physrev.00061.2017. PMC 6442923. PMID 30427277.
- Rasche P, Mertens A, Bröhl C, Theis S, Seinsch T, Wille M, et al. (8 May 2017). "The "Aachen fall prevention App" - a Smartphone application app for the self-assessment of elderly patients at risk for ground level falls". Patient Safety in Surgery. 11: 14. doi:10.1186/s13037-017-0130-4. PMC 5422970. PMID 28503199.
- "Los Parques de Mayores: Análisis y propuestas de intervención" [The Parks for the Elderly: Analysis and intervention proposals] (PDF) (in Spanish). Seville, Spain: Universidad Pablo de Olavide. Archived (PDF) from the original on 2021-07-14. Retrieved 2020-12-03.
Further reading
- Lord SR, Sherrington C, Menz HB, Close JC (March 2007). Falls in Older People: Risk Factors and Strategies for Prevention. Cambridge University Press. ISBN 978-0-521-68099-8.
External links
- Fall prevention NHS Choices
- Fall prevention for older adults US Centers for Disease Control and Prevention
- Fall Prevention in the Workplace US Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health