Follicular atresia
Follicular atresia refers to the process in which a follicle fails to develop, thus preventing it from ovulating and releasing an egg.[1] It is a normal, naturally occurring progression that occurs as mammalian ovaries age. Approximately 1% of mammalian follicles in ovaries undergo ovulation and the remaining 99% of follicles go through follicular atresia as they cycle through the growth phases. In summary, follicular atresia is a process that leads to the follicular loss and loss of oocytes, and any disturbance or loss of functionality of this process can lead to many other conditions.[2]
Background
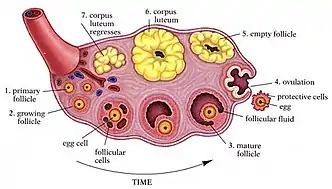
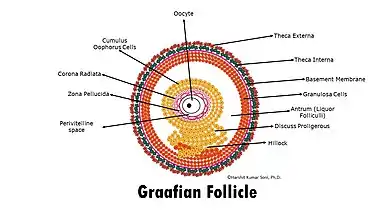
Ovaries are the site of development and breakdown of ovarian follicles which secrete hormones and oocytes. Oocytes are immature eggs and are surrounded by granulosa cells and internal and external theca cells.[3] Oocytes are then able to mature within the follicle through meiosis. In humans with ovaries, this process occurs continuously, as they are born with a finite number of follicles (between 500,000-1,000,000 follicles), and about 99% of follicles undergo atresia.[4] Only one follicle will be mature enough to release an egg and may be fertilized.[5] Typically around 20 follicles mature each month but only a single follicle is ovulated; the follicle from which the oocyte was released becomes the corpus luteum. The corpus luteum is the last stage of the ovarian follicles' lifecycle. It has an important role in secreting estrogen and progesterone to prepare the body for conception. If conception does not occur, then it will be shed and is known as the corpus albicans.[6] It has been observed that this mechanism is important in regulating and maintaining a healthy reproductive system in mammals.
Menopause
Follicular atresia occurs throughout all stages of follicular development, until the follicular reserve is completely exhausted.[7] Exhaustion of the follicular reserve occurs at menopause, which is typically around the age of 51 in humans with ovaries. The dramatic decrease in estrogen and progesterone levels that is characteristic of menopause is caused by follicular atresia. Breakdown of the follicles prevent them from releasing hormones such as estrogen. Progesterone levels also decrease during menopause because without any follicles, there is no development of the corpus luteum, which is the major source of circulating progesterone levels in humans.[8]
Mechanism
Atresia is a complex, hormonally controlled apoptotic process that depends dominantly on granulosa cell apoptosis. Follicular atresia is inhibited by follicle-stimulating hormone (FSH), which promotes follicle development.[9] Once the follicle has developed, it secretes estrogen, which in high levels decreases secretions of FSH.[10] Granulosa cell apoptosis is considered the underlying mechanism of follicular atresia, and has been associated with five ligand-receptor systems involved in cell death:[3][11][12][13][14]
- tumor necrosis factor alpha (TNF alpha) and receptors
- Fas ligand and receptors[15]
- TNF-related apoptosis-inducing ligand (TRAIL; also called APO-2) and receptors
- APO-3 ligand and receptors
- PFG-5 ligand and receptors
Granulosa cell apoptosis is promoted by tumor necrosis factor-alpha (TNFα), although the mechanism of how it occurs is unclear.[16]
Fas antigen, a cell surface receptor protein, that is expressed on granulosa cells, mediates signals that induce apoptosis by binding Fas ligand and therefore plays an important role in follicular atresia.[17] Lack of a functional Fas ligand / Fas receptor system has been linked to abnormal follicle development, and increased numbers of secondary follicles as a result of the inability to induce apoptosis.[18]
TNF-related apoptosis-inducing ligand (TRAIL) activates caspase 3 (CASP3), which in turn interacts with caspases 6, 7, 8, 9, and 10 to induce apoptosis in granulosa cells.[19]
In addition, two intracellular inhibitor proteins, cellular FLICE-like inhibitory protein short form (cFLIPS) and long form (cFLIPL), which are strongly expressed in granulosa cells, may act as anti-apoptotic factors.[11]
Anti-Mullerian hormone (AMH) has been studied to be a key regulator in the ovaries in humans that inhibits follicular atresia. It has been proven that AMH reduces the growth of follicles and its upregulation proposes a potential pathophysiological pathway in PCOS.[20] Using indirect comparators to derive this hypothesis, exploring different patient populations such as individuals who have polycystic ovary syndrome (PCOS) help support the hypothesis that AMH may be a key regulator in inhibiting follicular atresia.[20][21]
It has been proposed that enhanced levels of Nitrogen oxide in rats can prevent atresia of the ovarian follicle, while depressed levels have the opposite effect.[22]
Morphology
From studying dairy cows, two forms of follicular atresia have been identified: antral and basal.
Antral
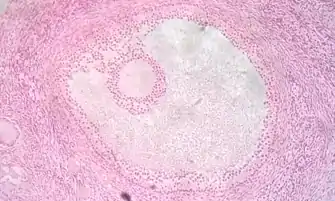
Antral follicular atresia is characterized by the apoptosis of granulosa cells within the antral layers of the granulosa membrane and sometimes within the antrum itself. During this process, the presence of pyknotic nuclei in the antral layers of the membrane can be observed.[23] Apoptosis ensures that the follicle gets eliminated without triggering an inflammatory response.[24] Antral follicular atresia causes no damage to basal granulosa cells. This type of follicular atresia is often considered the classic and most commonly observed form. In most species, it occurs throughout follicular development and is universally seen in large follicles (>5mm diameter).[24]
Basal
Basal follicular atresia is characterized by the destruction of granulosa cells in the basal layer of the granulosa membrane. Macrophages have often been observed, penetrating the basal lamina during this type of follicular atresia. These macrophages phagocytose the basal granulosa cells. An increased deposition of collagen in the theca layer of the follicle can also be observed.[23] Basal follicular atresia causes no damage to antral granulosa cells.This form of follicular atresia has only been observed in small follicles of dairy cows (< 5mm diameter), and has not been reported in any other species.[24]
Related diseases
Undergoing follicular atresia is necessary in order for mammals to maintain a healthy reproductive system. Mammalian ovaries ovulate about 1% of the follicles and the remaining follicles may go through atresia as it cycles through the growth phases.[2] However, disorders in the regulation of follicle breakdown and generation can lead to various pathologies:
Premature ovarian failure
Premature ovarian failure (POF) (also called premature ovarian insufficiency) is the loss of ovarian function before the age of 40 due to follicular dysfunction such as accelerated follicular atresia.[25] POF may present itself with characteristics and symptoms such as loss of menstruation for at least 4 months and also increased serum follicle-stimulating hormone (FSH) concentration (greater than or equal to 40 IU/L).[26] There may be many causes of POF, ranging from genetic disorders to surgery, radiation therapy, and exposure to environmental toxicants. Accelerated follicular atresia due to chromosomal and genomic defects accounts for up to one-half of all POF cases. For example, Fragile X syndrome, Turner syndrome, and various autosomal diseases such as galactosemia have been linked to follicular deficiencies. Smoking has also been found to increase follicular atresia and lead to premature ovarian failure.[27] Some of the short term effects of POF are hot flashes, irregular heart beat/heart palpitations, night sweats, urogenital symptoms, and headaches; some of the more long-term consequences of POF are osteoporosis, infertility, cardiovascular diseases, and possible premature death.[26]
Ovarian follicular cysts
When an ovarian follicle fails to undergo atresia and release an egg, it can grow to form a cyst.[28][29] This may be due to an overproduction of FSH or an inadequate supply of LH. Most follicular cysts are harmless and resolve on their own within several months. However, rarely a cyst will grow to be very large (greater than 7 cm), cause abdominal pain, or rupture, in which case pain relievers or emergency surgery may be required. If the cyst lasts for longer than a few months, a physician may recommend surgical removal or testing to determine if it is cancerous. Ultrasound is a common method of visualizing a cyst to determine treatment.
Ovarian Cancer
Ovarian cancer is highly prevalent amongst humans who have ovaries and leads to many deaths in the United States.[30] Since FSH inhibits follicular atresia, the overproduction of FSH can lead to excessive follicle formation and increased risk of ovarian cancer.[31]
The inability to regulate granulosa cell apoptosis and undergo follicular atresia, due to overexpression of certain genes, has been linked to the development of some hormone-related cancers (such as granulosa cell tumors) and chemo-resistance in mouse models.[32][33]
According to the gonadotropin theory, follicular depletion associated with incessant follicular atresia has also been hypothesized as a potential etiology for ovarian cancer, due to an increase in serum gonadotropins. This leads to an inflammatory environment which promotes cellular turnover and tumor development.[34]
Ovarian cancer is characterized by some generalized symptoms such as bloating or swelling in the abdomen, pelvic pain, gastrointestinal symptoms (i.e. loss of appetite, nausea, constipation, and unexpected weight loss).[35] Many people who are diagnosed with ovarian cancer also report feeling very full fast and many of them having a feeling on unexpected continuous bloating in their abdomen.[36]
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome, or PCOS affects 6-12% of humans with ovaries of reproductive age in the United States, and is one of the common causes of female infertility.[37] The mechanism of PCOS is unknown, but is multifactorial. It has been observed that certain genes related to steroid and androgenic hormone production may contribute to development of the disease in individuals, environmental factors such as insulin resistance and obesity, and passing down of genetics from first degree relatives.[38]
Diagnosis of PCOS is based on meeting two of the three clinical criteria based on the Rotterdam Criteria: chronic anovulation (the ovum is not released from the ovary during menstrual cycle), hyperandrogenism (increased levels of androgen hormones, such as testosterone), and large number of ovarian cysts.[38] Symptoms and characteristics of PCOS include irregular periods or missed periods, excess body hair or thinning hair, weight gain, acne.
PCOS is correlated with other metabolic comorbidities. One of large concern is obesity and insulin resistance. This is of high interest when assessing treatment and management of PCOS. Other risk factors include traditional cardiovascular disease risk factors such as dyslipidemia and hypertension.[39]
Non-pharmacological management and treatment of PCOS include dietary intervention. While there is no one optimal diet or superior diet, as this disease is highly individualized, diets that impact weight loss and insulin resistance have been shown to improve reproductive function.[40] Examples of these diets include the DASH diet (Dietary Approach to Stop Hypertension) and the ketogenic diet. However it is important to consult a medical professional before starting on such diet is safe.
Pharmacological management may be recommended for those who have comorbid conditions, such as obesity, type 2 diabetes, etc. Guidelines suggest possible oral contraceptives in combination with metformin (anti-diabetic medication), and/or anti-androgen agents.[41] As PCOS is a highly individualized condition, each individual's management and goals will look different.
See also
References
- McGee EA, Horne J (2018). "Follicle Atresia". In Skinner MK (ed.). Encyclopedia of Reproduction (Second ed.). Oxford: Academic Press. pp. 87–91. doi:10.1016/b978-0-12-801238-3.64395-7. ISBN 978-0-12-815145-7.
- Liu Z, Li F, Xue J, Wang M, Lai S, Bao H, He S (August 2020). "Esculentoside A rescues granulosa cell apoptosis and folliculogenesis in mice with premature ovarian failure". Aging. 12 (17): 16951–16962. doi:10.18632/aging.103609. PMC 7521512. PMID 32759462.
- Zhou J, Peng X, Mei S (2019). "Autophagy in Ovarian Follicular Development and Atresia". International Journal of Biological Sciences. 15 (4): 726–737. doi:10.7150/ijbs.30369. PMC 6429023. PMID 30906205.
- Wilkosz P, Greggains GD, Tanbo TG, Fedorcsak P (2014). "Female reproductive decline is determined by remaining ovarian reserve and age". PLOS ONE. 9 (10): e108343. Bibcode:2014PLoSO...9j8343W. doi:10.1371/journal.pone.0108343. PMC 4195570. PMID 25310678.
- Zhang J, Liu Y, Yao W, Li Q, Liu H, Pan Z (July 2018). "Initiation of follicular atresia: gene networks during early atresia in pig ovaries". Reproduction. 156 (1): 23–33. doi:10.1530/REP-18-0058. PMID 29743261. S2CID 13689486.
- Kirkendoll SD, Bacha D (2022). "Histology, Corpus Albicans". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 31424854. Retrieved 2022-07-26.
- Banerjee S, Banerjee S, Saraswat G, Bandyopadhyay SA, Kabir SN (2014). "Female reproductive aging is master-planned at the level of ovary". PLOS ONE. 9 (5): e96210. Bibcode:2014PLoSO...996210B. doi:10.1371/journal.pone.0096210. PMC 4008600. PMID 24788203.
- Oliver R, Pillarisetty LS (2022). "Anatomy, Abdomen and Pelvis, Ovary Corpus Luteum". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30969526. Retrieved 2022-08-04.
- Kaipia A, Hsueh AJ (1997). "Regulation of ovarian follicle atresia". Annual Review of Physiology. 59: 349–363. doi:10.1146/annurev.physiol.59.1.349. PMID 9074768.
- Marshall JC, Case GD, Valk TW, Corley KP, Sauder SE, Kelch RP (February 1983). "Selective inhibition of follicle-stimulating hormone secretion by estradiol. Mechanism for modulation of gonadotropin responses to low dose pulses of gonadotropin-releasing hormone". The Journal of Clinical Investigation. 71 (2): 248–257. doi:10.1172/JCI110765. PMC 436863. PMID 6401767.
- Manabe N, Goto Y, Matsuda-Minehata F, Inoue N, Maeda A, Sakamaki K, Miyano T (October 2004). "Regulation mechanism of selective atresia in porcine follicles: regulation of granulosa cell apoptosis during atresia". The Journal of Reproduction and Development. 50 (5): 493–514. doi:10.1262/jrd.50.493. PMID 15514456.
- Matsuda-Minehata F, Goto Y, Inoue N, Manabe N (October 2005). "Changes in expression of anti-apoptotic protein, cFLIP, in granulosa cells during follicular atresia in porcine ovaries". Molecular Reproduction and Development. 72 (2): 145–151. doi:10.1002/mrd.20349. PMID 16010689. S2CID 10644197.
- Matsuda F, Inoue N, Goto Y, Maeda A, Cheng Y, Sakamaki K, Manabe N (October 2008). "cFLIP regulates death receptor-mediated apoptosis in an ovarian granulosa cell line by inhibiting procaspase-8 cleavage". The Journal of Reproduction and Development. 54 (5): 314–320. doi:10.1262/jrd.20051. PMID 18603835.
- Asselin E, Xiao CW, Wang YF, Tsang BK (2000). "Mammalian follicular development and atresia: role of apoptosis". Biological Signals and Receptors. 9 (2): 87–95. doi:10.1159/000014627. PMID 10810203. S2CID 30459318.
- Manabe N, Matsuda-Minehata F, Goto Y, Maeda A, Cheng Y, Nakagawa S, et al. (July 2008). "Role of cell death ligand and receptor system on regulation of follicular atresia in pig ovaries". Reproduction in Domestic Animals. 43 (Suppl 2): 268–272. doi:10.1111/j.1439-0531.2008.01172.x. PMID 18638134.
- Yamamoto Y, Kuwahara A, Taniguchi Y, Yamasaki M, Tanaka Y, Mukai Y, et al. (2015). "Tumor necrosis factor alpha inhibits ovulation and induces granulosa cell death in rat ovaries". Reproductive Medicine and Biology. 14 (3): 107–115. doi:10.1007/s12522-014-0201-5. PMC 4490172. PMID 26161038.
- Yang R, Xu S, Zhao Z, Li J (February 2012). "Fas ligand expression and mediated activation of an apoptosis program in bovine follicular granulosa cells". Gene. 493 (1): 148–154. doi:10.1016/j.gene.2011.11.032. PMID 22155318.
- Porter DA, Harman RM, Cowan RG, Quirk SM (April 2001). "Relationship of Fas ligand expression and atresia during bovine follicle development". Reproduction. 121 (4): 561–566. doi:10.1530/rep.0.1210561. PMID 11277875.
- Naimi A, Movassaghpour AA, Hagh MF, Talebi M, Entezari A, Jadidi-Niaragh F, Solali S (February 2018). "TNF-related apoptosis-inducing ligand (TRAIL) as the potential therapeutic target in hematological malignancies". Biomedicine & Pharmacotherapy. 98: 566–576. doi:10.1016/j.biopha.2017.12.082. PMID 29288972.
- Shrikhande L, Shrikhande B, Shrikhande A (October 2020). "AMH and Its Clinical Implications". Journal of Obstetrics and Gynaecology of India. 70 (5): 337–341. doi:10.1007/s13224-020-01362-0. PMC 7515982. PMID 33041549.
- Garg D, Tal R (July 2016). "The role of AMH in the pathophysiology of polycystic ovarian syndrome". Reproductive Biomedicine Online. 33 (1): 15–28. doi:10.1016/j.rbmo.2016.04.007. PMID 27174394.
- Luo Y, Zhu Y, Basang W, Wang X, Li C, Zhou X (2021). "Roles of Nitric Oxide in the Regulation of Reproduction: A Review". Frontiers in Endocrinology. 12: 752410. doi:10.3389/fendo.2021.752410. PMC 8640491. PMID 34867795.
- Makarevich AV, Földešiová M, Pivko J, Kubovičová E, Chrenek P (December 2018). "Histological characteristics of ovarian follicle atresia in dairy cows with different milk production". Anatomia, Histologia, Embryologia. 47 (6): 510–516. doi:10.1111/ahe.12389. PMID 30022512. S2CID 51697201.
- Townson DH, Combelles CM (2012). "Ovarian Follicular Atresia". In Darwish A (ed.). Basic Gynecology - Some Related Issues. InTech. doi:10.5772/32465. ISBN 978-953-51-0166-6. Retrieved 2022-07-26.
- Gago LA, Ginsburg KA (2004). "Premature Ovarian Failure". In Martini L (ed.). Encyclopedia of Endocrine Diseases. New York: Elsevier. pp. 65–72. doi:10.1016/B0-12-475570-4/01066-0. ISBN 978-0-12-475570-3. Retrieved 2022-07-28.
- Podfigurna-Stopa A, Czyzyk A, Grymowicz M, Smolarczyk R, Katulski K, Czajkowski K, Meczekalski B (September 2016). "Premature ovarian insufficiency: the context of long-term effects". Journal of Endocrinological Investigation. 39 (9): 983–990. doi:10.1007/s40618-016-0467-z. PMC 4987394. PMID 27091671.
- Klinger FG, Rossi V, De Felici M (2015). "Multifaceted programmed cell death in the mammalian fetal ovary". The International Journal of Developmental Biology. 59 (1–3): 51–54. doi:10.1387/ijdb.150063fk. PMID 26374525.
- Cole L (2016). "Chapter 6.8 - Ovarian Cystic Disorders". In Cole L, Kramer PR (eds.). Human Physiology, Biochemistry and Basic Medicine. Boston: Academic Press. pp. 219–221. doi:10.1016/B978-0-12-803699-0.00046-3. ISBN 978-0-12-803699-0. Retrieved 2022-07-28.
- "Follicular Cyst". Definition & Patient Education. Healthline. 2016. Retrieved 2022-07-28.
- Hunn J, Rodriguez GC (March 2012). "Ovarian cancer: etiology, risk factors, and epidemiology". Clinical Obstetrics and Gynecology. 55 (1): 3–23. doi:10.1097/GRF.0b013e31824b4611. PMID 22343225.
- Zhang Z, Jia L, Feng Y, Zheng W (June 2009). "Overexpression of follicle-stimulating hormone receptor facilitates the development of ovarian epithelial cancer". Cancer Letters. 278 (1): 56–64. doi:10.1016/j.canlet.2008.12.024. PMID 19181441.
- Lee K, Pisarska MD, Ko JJ, Kang Y, Yoon S, Ryou SM, et al. (October 2005). "Transcriptional factor FOXL2 interacts with DP103 and induces apoptosis". Biochemical and Biophysical Research Communications. 336 (3): 876–881. doi:10.1016/j.bbrc.2005.08.184. PMID 16153597.
- Kim JH, Yoon S, Park M, Park HO, Ko JJ, Lee K, Bae J (April 2011). "Differential apoptotic activities of wild-type FOXL2 and the adult-type granulosa cell tumor-associated mutant FOXL2 (C134W)". Oncogene. 30 (14): 1653–1663. doi:10.1038/onc.2010.541. PMID 21119601. S2CID 21975528.
- Smith ER, Xu XX (November 2008). "Ovarian ageing, follicle depletion, and cancer: a hypothesis for the aetiology of epithelial ovarian cancer involving follicle depletion". The Lancet. Oncology. 9 (11): 1108–1111. doi:10.1016/S1470-2045(08)70281-X. PMC 2713057. PMID 19012860.
- Okunowo AA, Adaramoye VO (December 2018). "Women's Knowledge on Ovarian Cancer Symptoms and Risk Factors in Nigeria: An Institutional-based Study". Journal of Epidemiology and Global Health. 8 (1–2): 34–41. doi:10.2991/j.jegh.2018.07.002. PMC 7325817. PMID 30859785.
- Pitts MK, Heywood W, Ryall R, Smith AM, Shelley JM, Richters J, Simpson JM (February 2011). "High prevalence of symptoms associated with ovarian cancer among Australian women". The Australian & New Zealand Journal of Obstetrics & Gynaecology. 51 (1): 71–78. doi:10.1111/j.1479-828X.2010.01284.x. PMID 21299513. S2CID 21331891.
- Rasquin Leon LI, Anastasopoulou C, Mayrin JV (2022). "Polycystic Ovarian Disease". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29083730. Retrieved 2022-08-04.
- Zeng LH, Rana S, Hussain L, Asif M, Mehmood MH, Imran I, et al. (2022). "Polycystic Ovary Syndrome: A Disorder of Reproductive Age, Its Pathogenesis, and a Discussion on the Emerging Role of Herbal Remedies". Frontiers in Pharmacology. 13: 874914. doi:10.3389/fphar.2022.874914. PMC 9340349. PMID 35924049.
- Hoeger KM, Dokras A, Piltonen T (March 2021). "Update on PCOS: Consequences, Challenges, and Guiding Treatment". The Journal of Clinical Endocrinology and Metabolism. 106 (3): e1071–e1083. doi:10.1210/clinem/dgaa839. PMID 33211867. S2CID 227078090.
- Che X, Chen Z, Liu M, Mo Z (2021). "Dietary Interventions: A Promising Treatment for Polycystic Ovary Syndrome". Annals of Nutrition & Metabolism. 77 (6): 313–323. doi:10.1159/000519302. PMID 34610596. S2CID 238411748.
- Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. (September 2018). "Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome". Human Reproduction. 33 (9): 1602–1618. doi:10.1093/humrep/dey256. PMC 6112576. PMID 30052961.