Endovascular coiling
Endovascular coiling is an endovascular treatment for intracranial aneurysms and bleeding throughout the body. The procedure reduces blood circulation to the aneurysm through the use of microsurgical detachable platinum wires, with the clinician inserting one or more into the aneurysm until it is determined that blood flow is no longer occurring within the space. It is one of two main treatments for cerebral aneurysms, the other being surgical clipping. Clipping is an alternative to stenting for bleeding.
| Endovascular coiling | |
|---|---|
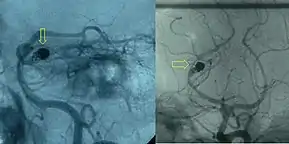 Post-embolization arteriogram showing coiled aneurysm (indicated by yellow arrows) of the posteriorcerebral artery with a residual aneurysmal sac. | |
| Other names | Endovascular embolization |
| Specialty | Interventional neuroradiology |
Medical uses
Endovascular coiling is used to treat cerebral aneurysms. The main goal is prevention of rupture in unruptured aneurysms, and prevention of rebleeding in ruptured aneurysms by limiting blood circulation to the aneurysm space. Clinically, packing density is recommended to be 20-30% or more of the aneurysm's volume, typically requiring deployment of multiple wires.[1] Higher volumes may be difficult due to the delicate nature of the aneurysm; intraoperative rupture rates are as high as 7.6% for this procedure.[2] In ruptured aneurysms, coiling is performed quickly after rupture because of the high risk of rebleeding within the first few weeks after initial rupture. The patients most suitable for endovascular coiling are those with aneurysms with a small neck size (preferably <4 mm), luminal diameter <25 mm and those that are distinct from the parent vessel.[3] Larger aneurysms are subject to compaction of coils, due to both looser packing densities (more coils are needed) and increased blood flow. Coil compaction renders them unsuitable as they are incapable of stemming blood flow.[4] However, technological advances have made coiling of many other aneurysms possible as well.
Results
A number of studies have questioned the efficacy of endovascular coiling over the more traditional surgical clipping. Most concerns involve the chance of later bleeds or other recanalization.[5][6][7] Due to its less invasive nature, endovascular coiling usually presents faster recovery times than surgical clipping, with one study finding a significant decrease in probability of death or dependency compared to a neurosurgical population.[8] Complication rates for coiling as well are generally found to be lower than microsurgery (11.7% and 17.6% for coiling and microsurgery, respectively). Despite this, interoperative rupture rates for coiling have been documented as being as high as 7.6%.[2] Clinical results are found to be similar at a two-month and one year follow-up between coiling and neurosurgery.[9]
Reported recurrence rates are quite varied, with rates between 20 and 50% of aneurysms recurring within one year of coiling, and with the recurrence rate increasing with time.[2][10] These results are similar to those previously reported by other endovascular groups.[11] Other studies have questioned whether new matrix coils work better than bare platinum coils.[12]
The International Subarachnoid Aneurysm Trial tested the efficacy of endovascular coiling against the traditional micro-surgical clipping. The study initially found very favorable results for coiling, however its results and methodology were criticized. Since the study's release in 2002, and again in 2005, some studies have found higher recurrence rates with coiling, while others have concluded that there is no clear consensus between which procedure is preferred.[13]
Risks
Risks of endovascular coiling include stroke, aneurysm rupture during the procedure and aneurysm recurrence and rupture after the procedure.[3] Additionally in some patients coiling may not be successful. In general, coiling is only performed when the risk of aneurysm rupture is higher than the risks of the procedure itself.
Similar to patients who experience neurosurgical procedures, coiling results in an increase in resting energy expenditure, albeit at a slightly reduced rate than their neurosurgery counterpart. This can lead to malnutrition if steps are not taken to compensate for the increased metabolic rate.[14]
Mechanism
The treatment works by promoting blood clotting (thrombosis) in the aneurysm, eventually sealing it from the blood flow. This is accomplished by decreasing the amount of blood flow going into the aneurysm, increasing the residence time of the blood (thereby lowering the velocity) in the aneurysm space and reducing the wall shear stress of the aneurysm wall. This change in the blood flow, or hemodynamics, is ultimately dependent on several factors, including:
- aneurysm type (directly on the parent artery or on a bifurcation of an artery)
- aneurysm position (relative angle of aneurysm to approaching blood flow)
- coil packing density
- angle of parent vessel curvature
- size of aneurysm neck[1][15][2]
While these factors are crucial to the success of the procedure, thrombosis ultimately is dependent on biological processes, with the coiling only providing the appropriate conditions for the process to occur, and hopefully closing the aneurysm.
Procedure

Endovascular coiling is usually performed by an interventional neuroradiologist or neurosurgeon with the patient under general anaesthesia. The whole procedure is performed under fluoroscopic imaging guidance. A guiding catheter is inserted through the femoral artery and advanced to a site close to the aneurysm after which angiography is performed to localize and assess the aneurysm. After this, a microcatheter is navigated into the aneurysm.
The treatment uses detachable coils made of platinum that are inserted into the aneurysm using the microcatheter. A variety of coils are available, including Guglielmi Detachable Coils (GDC) which are platinum, Matrix coils which are coated with a biopolymer, and hydrogel coated coils. Coils are also available in a variety of diameters, lengths, and cross sections.[16] A coil is first inserted along the aneurysm wall to create a frame, with the core then being filled with more coils.[17] A series of progressively smaller coils may also be used. Success is determined by injecting a contrast dye into parent artery and qualitatively determining if dye is flowing into the aneurysm space during fluoroscopy. If no flow is observed, the procedure is considered completed.[2] In the case of wide-necked aneurysms a stent may be used.[18]
History
Endovascular coiling was a developed through the synthesis of a number of innovations that took place between 1970 and 1990 in the field of electronics, neurosurgery, and interventional radiology.[4] While the procedure itself has been and continues to be compared to surgical clipping, the development of the concept and procedure has resulted in it becoming the gold standard at many centers.[4]
Filling the intravascular compartment
The first documented technique of using metal coils to induce thrombosis was accomplished by Mullan in 1974. Copper coils were inserted into a giant aneurysm through externally puncturing the aneurysm wall via craniotomy. Five patients died, with ten having satisfactory process.[19] It did not gain popularity due to the specialized equipment required, in addition to the technique being unsuitable for many types of aneurysms.[4] Later, in 1980, similar techniques were developed by Alksne and Smith using iron suspended in methyl methcrylate in a limited set of patients. There were no deaths in 22 consecutive cases with low morbidity.[20] This technique also did not gain traction due to advances in clipping.[4]
Endovascular approaches
As a means of avoiding invasive methods, early endovascular interventions involved the usage of detachable and nondetachable balloon catheters to occlude the aneurysm while preserving the parent artery.[21] Despite the innovative approach, the aneurysms were often found to adapt to the shape of the balloon itself resulting in higher incidents of aneurysm rupture. This procedure was deemed "uncontrollable" due to its high morbidity and mortality rate, but it demonstrated that the endovascular approach was feasible for many aneurysms.[4] Endovascular coils would later be used in 1989 by Hilal et al., but these were short, stiff coils that offered no control, preventing dense packing of the aneurysm.[22] Controllable microguidewire systems were later used.[4]
Detachable coil system
In 1983 the use of electrically induced thrombosis for intracranial aneurysms was described for the first time.[23] A stainless steel electrode supplied a positive current to the aneurysm to stimulate electrothrombosis. Minimal occlusion was achieved, but the researchers discovered that the erosion of the electrode due to electrolysis would be useful as a detachment system.[4] Detachable coils were constructed from a platinum coil soldered to a stainless steel delivery wire, first described in 1991 by Guglielmi et al.[3] When combined with a controllable microguide wire system, multiple coils could be inserted to fully pack an aneurysm.[4]
Research
Given the complexity of modeling the vasculature, much research has been devoted towards modeling the hemodynamics of an aneurysm before and after an intervention. Techniques such as particle image velocimetry (PIV) and computational fluid dynamics/finite element analysis (CFD/FEA) have yielded results that have influenced the direction of research, but no model to date has been able to account for all factors present.[2][24][25] Advantages of the in-silico research method include flexibility of selecting variables, but one comparative study has found that simulations tend to over-emphasis results compared to PIV, and are more beneficial for trends than exact values.[25]
Medical images, particularly CT angiography, can be used to generate 3D reconstructions of patient specific anatomy. When combined with CFD/FEA, hemodynamics can be estimated in patient specific simulations, giving the clinician greater predictive tools for surgical planning and outcome evaluation to best promote thrombus formation.[26][27] However, most computer models use many assumptions for simplicity, including rigid walls (non-elastic) for vasculature, substituting a porous medium in place of physical coil representations, and navier-stokes for fluid behavior. However, new predictive models are being developed as computational power increases, including algorithms for simulations of coil behavior in-vivo.[16]
References
- Otani, Tomohiro; Nakamura, Masanori; Fujinaka, Toshiyuki; Hirata, Masayuki; Kuroda, Junko; Shibano, Katsuhiko; Wada, Shigeo (2013-03-26). "Computational fluid dynamics of blood flow in coil-embolized aneurysms: effect of packing density on flow stagnation in an idealized geometry". Medical & Biological Engineering & Computing. 51 (8): 901–910. doi:10.1007/s11517-013-1062-5. ISSN 0140-0118. PMID 23529587. S2CID 7811834.
- Babiker, M. H.; Gonzalez, L. F.; Albuquerque, F.; Collins, D.; Elvikis, A.; Zwart, C.; Roszelle, B.; Frakes, D. H. (2013-04-01). "An In Vitro Study of Pulsatile Fluid Dynamics in Intracranial Aneurysm Models Treated with Embolic Coils and Flow Diverters". IEEE Transactions on Biomedical Engineering. 60 (4): 1150–1159. doi:10.1109/TBME.2012.2228002. ISSN 0018-9294. PMID 23192467. S2CID 206612828.
- Currie, S; Mankad, K; Goddard, A (Jan 2011). "Endovascular treatment of intracranial aneurysms: review of current practice". Postgraduate Medical Journal. 87 (1023): 41–50. doi:10.1136/pgmj.2010.105387. PMID 20937736. S2CID 30220296.
- Guglielmi, Guido (2009-03-13). "History of the genesis of detachable coils". Journal of Neurosurgery. 111 (1): 1–8. doi:10.3171/2009.2.JNS081039. ISSN 0022-3085. PMID 19284239.
- J Neurointerv Surg. 2011 Apr 27. [Epub ahead of print]
- Campi A, Ramzi N, Molyneux AJ, Summers PE, Kerr RS, Sneade M, Yarnold JA, Rischmiller J, Byrne JV (May 2007). "Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT)". Stroke. 38 (5): 1538–44. doi:10.1161/STROKEAHA.106.466987. PMID 17395870.
- Mitchell P, Kerr R, Mendelow AD, Molyneux A. Could late rebleeding overturn the superiority of cranial aneurysm coil embolization over clip ligation seen in ISAT?" Journal of Neurosurgery 108: 437-442, March 2008. But see, J Mocco, L. Nelson Hopkins, "International Subarachnoid Aneurysm Trial analysis", Journal of Neurosurgery, March 2008 / Vol. 108 / No. 3 / Pages 436-436.
- Molyneux, Andrew J; Birks, Jacqueline; Clarke, Alison; Sneade, Mary; Kerr, Richard S C (2015-02-21). "The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT)". The Lancet. 385 (9969): 691–697. doi:10.1016/s0140-6736(14)60975-2. PMC 4356153. PMID 25465111.
- Li, Jian; Su, Long; Ma, Jian; Kang, Ping; Ma, Liujia; Ma, Lianting (2017). "Endovascular coiling versus microsurgical clipping for patients with ruptured very small intracranial aneurysms: Management strategies and clinical outcomes- of 162 cases". World Neurosurgery. 99: 763–769. doi:10.1016/j.wneu.2015.11.079. PMID 26732968.
- Piotin, M; Spelle, L; Mounayer, C; Salles-Rezende, MT; Giansante-Abud, D; Vanzin-Santos, R; Moret, J (May 2007). "Intracranial aneurysms: treatment with bare platinum coils—aneurysm packing, complex coils, and angiographic recurrence". Radiology. 243 (2): 500–8. doi:10.1148/radiol.2431060006. PMID 17293572.
- Raymond, J; Guilbert, F; Weill, A; Georganos, SA; Juravsky, L; Lambert, A; Lamoureux, J; Chagnon, M; Roy, D (June 2003). "Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils". Stroke. 34 (6): 1398–1403. doi:10.1161/01.STR.0000073841.88563.E9. PMID 12775880.
- Piotin M, Spelle L, Mounayer C, Loureiros C, Ghorbani A, Moret J. Intracranial aneurysms coiling with matrix. Immediate results in 152 patients and midterm anatomic follow-up from 115 patients. Stroke November 2008 (e-pub ahead of print)
- Raja PV, Huang J, Germanwala AV, Gailloud P, Murphy KP, Tamargo RJ (2008). "Microsurgical clipping and endovascular coiling of intracranial aneurysms: A critical review of the literature". Neurosurgery. 62 (6): 1187–1202. doi:10.1227/01.neu.0000333291.67362.0b. PMID 18824986. S2CID 21058347.
- Nagano, Ayano; Yamada, Yoshitaka; Miyake, Hiroji; Domen, Kazuhisa; Koyama, Tetsuo (April 2016). "Increased Resting Energy Expenditure after Endovascular Coiling for Subarachnoid Hemorrhage". Journal of Stroke and Cerebrovascular Diseases. 25 (4): 813–818. doi:10.1016/j.jstrokecerebrovasdis.2015.12.008. PMID 26796057.
- Hoi, Yiemeng; Meng, Hui; Woodward, Scott H.; Bendok, Bernard R.; Hanel, Ricardo A.; Guterman, Lee R.; Hopkins, L. Nelson (2004-10-01). "Effects of arterial geometry on aneurysm growth: three-dimensional computational fluid dynamics study". Journal of Neurosurgery. 101 (4): 676–681. doi:10.3171/jns.2004.101.4.0676. ISSN 0022-3085. PMID 15481725. S2CID 6565151.
- Morales, H. G.; Kim, M.; Vivas, E. E.; Villa-Uriol, M.-C.; Larrabide, I.; Sola, T.; Guimaraens, L.; Frangi, A. F. (2011-11-01). "How Do Coil Configuration and Packing Density Influence Intra-Aneurysmal Hemodynamics?". American Journal of Neuroradiology. 32 (10): 1935–1941. doi:10.3174/ajnr.A2635. ISSN 0195-6108. PMC 7965998. PMID 21885712.
- Morales, Hernan (2012). Endovascular coiling and its influence on intra-aneurysmal hemodynamics by image-based modeling. Barcelona, Spain. p. 19. ISBN 978-84-615-9824-3.
- Oushy, Soliman; Rinaldo, Lorenzo; Brinjikji, Waleed; Cloft, Harry; Lanzino, Giuseppe (June 2020). "Recent advances in stent-assisted coiling of cerebral aneurysms". Expert Review of Medical Devices. 17 (6): 519–532. doi:10.1080/17434440.2020.1778463. ISSN 1745-2422. PMID 32500761. S2CID 219328499.
- Mullan, S. (1974-12-01). "Experiences with surgical thrombosis of intracranial berry aneurysms and carotid cavernous fistulas". Journal of Neurosurgery. 41 (6): 657–670. doi:10.3171/jns.1974.41.6.0657. ISSN 0022-3085. PMID 4609023.
- Alksne, J. F.; Smith, R. W. (1980-06-01). "Stereotaxic occlusion of 22 consecutive anterior communicating artery aneurysms". Journal of Neurosurgery. 52 (6): 790–793. doi:10.3171/jns.1980.52.6.0790. ISSN 0022-3085. PMID 6991648.
- Serbinenko, F. A. (1974-08-01). "Balloon catheterization and occlusion of major cerebral vessels". Journal of Neurosurgery. 41 (2): 125–145. doi:10.3171/jns.1974.41.2.0125. ISSN 0022-3085. PMID 4841872.
- Group, British Medical Journal Publishing (1963-03-16). "Obliteration of Intracranial Aneurysms by Pilojection". Br Med J. 1 (5332): 700. doi:10.1136/bmj.1.5332.700-a. ISSN 0007-1447. S2CID 30623125.
- Guglielmi, G; Guerrisi, G; Guidetti, B (1983). "L'elettrotrombosi intravasale nelle malformazioni vascolari sperimentalmente provocate". Proceedings of III Congress of the Italian Society of Neuroradiology. Bari: Associazione Italiana di Neuroradiologia: 139–146.
- Wong, George K. C.; Poon, W. S. (2011-10-01). "Current status of computational fluid dynamics for cerebral aneurysms: the clinician's perspective". Journal of Clinical Neuroscience. 18 (10): 1285–1288. doi:10.1016/j.jocn.2011.02.014. ISSN 1532-2653. PMID 21795051. S2CID 22669620.
- Ford, Matthew D.; Nikolov, Hristo N.; Milner, Jaques S.; Lownie, Stephen P.; DeMont, Edwin M.; Kalata, Wojciech; Loth, Francis; Holdsworth, David W.; Steinman, David A. (2008-04-03). "PIV-Measured Versus CFD-Predicted Flow Dynamics in Anatomically Realistic Cerebral Aneurysm Models". Journal of Biomechanical Engineering. 130 (2): 021015–021015–9. doi:10.1115/1.2900724. ISSN 0148-0731. PMID 18412502. S2CID 31375424.
- Kakalis, N. M. P.; Mitsos, A. P.; Byrne, J. V.; Ventikos, Y. (2008-06-01). "The Haemodynamics of Endovascular Aneurysm Treatment: A Computational Modelling Approach for Estimating the Influence of Multiple Coil Deployment". IEEE Transactions on Medical Imaging. 27 (6): 814–824. doi:10.1109/TMI.2008.915549. ISSN 0278-0062. PMID 18541488. S2CID 27015964.
- Cheng, Xiao Qing; Chen, Qian; Zhou, Chang Sheng; Li, Jian Rui; Zhang, Zong Jun; Zhang, Long Jiang; Huang, Wei; Lu, Guang Ming (April 2016). "Whole-brain CT perfusion combined with CT angiography for ischemic complications following microsurgical clipping and endovascular coiling of ruptured intracranial aneurysms". Journal of Clinical Neuroscience. 26: 50–56. doi:10.1016/j.jocn.2015.05.067. PMID 26775148. S2CID 24464063.