Mueller–Weiss syndrome
Mueller–Weiss syndrome, also known as Mueller–Weiss disease, is a rare[2] idiopathic degenerative disease of the adult navicular bone characterized by progressive collapse and fragmentation, leading to mid- and hindfoot pain and deformity.[3][1] It is most commonly seen in females, ages 40–60.[4] Characteristic imaging shows lateral navicular collapse.[5] This disease had been historically considered to be a form of adult onset osteonecrosis, with blood flow cutoff to the navicular.[1][6]
| Mueller–Weiss syndrome | |
|---|---|
| Other names | Mueller–Weiss disease, Müller–Weiss syndrome, Brailsford disease[1] |
| Specialty | Orthopedics |
| Symptoms | Midfoot pain |
| Usual onset | Sub-acute |
| Treatment | Medication, surgery |

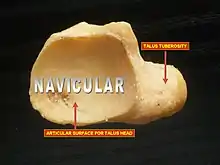
Navicular
The navicular, deriving its name from its boat–like shape, is a small but critical bone. It connects the ankle with the bones of the foot. It articulates with five tarsal bones (talus, cuboid, and three cuneiform bones) forming slightly mobile syndesmotic (fibrous) joints and has a significant function in maintaining the arch and the dynamic biomechanics of walking. The middle third of the bone lacks blood vessel penetration and it bears the majority of the load applied to the tarsal bones during weight bearing. Its vascular and biomechanical properties make it susceptible to injury. This may partly explain a higher risk of stress fractures and osteonecrosis in this location. Athletes who run, cut and pivot are particularly susceptible to injuries in this area. It is known as the keystone of the foot[7] and injuries to it can be "exasperating."[8]
History
In 1927 Walther Mueller, a Leipzig orthopedic surgeon, reported a case that had severe damage to the navicular bone with compression and fragmentation.
I have recently had occasion to observe changes in the os naviculare pedis in the adult, which may have some similarities with the Köhler-like disease of the adolescents, which is not yet known in this form.
In 1929 Konrad Weiss,[9] an Austrian radiologist, reported two patients with similar findings. The disease was named after them, though there had been a 1925 report by Georg Schmidt of a similar case, but with no images provided. Mueller believed the problem was congenital; Weiss believed it was an osteonecrotic process as the radiological findings were similar to Keinbock's disease, another osteonecrotic condition.[10][9] Since then controversy has persisted around the cause and pathogenesis of the disease.[11][1] In 1939 James Frederick Brailsford, an English radiologist, described nine cases in adult women.[9] Mueller–Weiss syndrome is also known as Brailsford disease.
Pathogenesis and pathomechanics
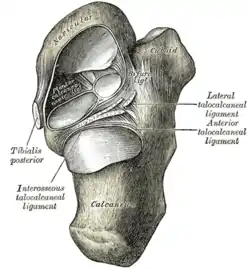
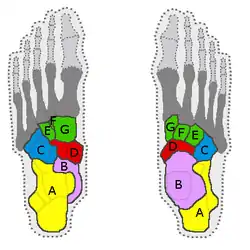
Mueller–Weiss syndrome had been traditionally considered a spontaneous osteonecrosis of the navicular bone, but there is no certain pathogenetic explanation. Pathologic evidence of osteonecrosis (empty lacunae)[12] is seen in only a minority of pathological specimens.[13][14] It is frequently bilateral and associated with increased body mass.[15] Factors that have been thought to play a role include trauma, delayed ossification of the navicular and chronic biomechanical factors that put stress on the navicular.[16][15] Multiple pathogenetic theories have been proposed over the years.[11] Pathomechanic abnormalities involve shifting of the foot bones, which leads to a paradoxic flat foot, with a varus deformity instead of a valgus.[1] Multiple ligaments and the posterior tibial tendon attach to the navicular. These perform a significant function in acting as a dynamic stabilizer and maintaining bipedal biomechanics.[8]
Regardless of the exact cause, the pathogenesis of Mueller-Weiss syndrome is probably multifactorial and related to chronic loading on a suboptimally ossified navicular—a bone that is predisposed to central ischemia owing to its centripetal vascular perfusion arch.[8]
Presentation
The onset is sub-acute; subsequent foot discomfort may progress to disabling pain with prolonged standing. It is considered a pain out of proportion, where the symptoms described do not correspond to the other signs, making an early diagnosis more difficult.[15] Pain is in mid- and hindfoot, with tenderness on the top of the midfoot.[11] Depending on the severity there may be a hindfoot varus with a flat arch. Delay in diagnosis is particularly problematic; early diagnosis is critical. It is frequently misdiagnosed, increasing the level and length of pain and disability for affected patients. Other conditions which may mimic or have features of Mueller–Weiss include Paget's disease of bone, osteomyelitis, healing fractures, lupus, rheumatoid arthritis and Charcot arthropathy.[17]
Radiological findings
Weight-bearing radiography of the foot is the mainstay in diagnosis. MRI can be useful early in the disease to separate MWS from mimics and demonstrate bone marrow changes and effusion in adjacent joints; this will help making a diagnosis before changes on conventional weight-bearing X-rays.[18] Despite its distinctive radiological features, Mueller–Weiss syndrome is often a diagnosis of exclusion[15] and is felt to be under-diagnosed.[6][19]
Characteristic findings of conventional radiology include:
- Normal earliest in the disease
- Lateral collapse of the navicular
- Dorsomedial subluxation of the remnant navicular
- Lateral deviation of the talus
Severe disease may demonstrate:
- Pes planus (flat foot)
- Osteoarthritis of the talonavicular joint with or without the involvement of other midfoot joints[19]
Treatment
Treatment should be commenced as early as possible. Initial treatment is conservative, with modalities including immobilization with orthoses (such as a walking boot) or short leg casts,[4] activity modification, injections, physical therapy, radio frequency ablation,[20] and anti-inflammatories. Failure of conservative management is more likely in patients with mid-foot abduction and radiologically noted talonavicular arthritis.[4][21] Surgical options are reserved for greater than six months of severe pain. There is no gold standard of treatment, with many surgical approaches.[17]
Society and culture
Rafael Nadal has had symptoms of Mueller–Weiss in his left foot since the beginning of his tennis career in his late teens,[22] being diagnosed in 2005.[23] He put off surgery as long as he could.[24] He has successfully continued his career after having surgery in 2021, winning the 2022 Australian and French Opens, though continuing to play through pain.[2] In winning the French Open he had two numbing injections and anti-inflammatories before each of his seven matches[20] to alleviate the pain; he won the tournament playing on a numb foot. He said he would not do this again.[22] Regarding his injury:
I am not injured; I am a player living with an injury. It's something that is there, and unfortunately, my day by day is difficult, honestly. It's difficult for me to accept the situation sometimes.[2]
See also
References
- Samim, Mohammad; Moukaddam, Hicham A.; Smitaman, Edward (2016-08-01). "Imaging of Mueller-Weiss Syndrome: A Review of Clinical Presentations and Imaging Spectrum". American Journal of Roentgenology. 207 (2): W8–W18. doi:10.2214/AJR.15.15843. ISSN 0361-803X. PMID 27145453.
- Roy, Neelabhra. "What is Mueller-Weiss Syndrome, the foot injury Rafael Nadal suffers from?". www.sportskeeda.com. Archived from the original on 2022-05-13. Retrieved 2022-06-05.
- Hermena, Shady; Francis, Monica (2021-10-11). "Clinical Presentation, Imaging Features, and Management of Müller–Weiss Disease". Cureus. 13 (10): e18659. doi:10.7759/cureus.18659. ISSN 2168-8184. PMC 8579404. PMID 34786245. S2CID 242284155.
- Joseph, Veena Mariam; Lynser, Donboklang; Khan, Aman Yusuf; Daniala, C. (2021-12-20). "Mueller Weiss syndrome, a less elucidated and unusual cause of midfoot pain: A case report". Indian Journal of Musculoskeletal Radiology. 3 (2): 94–97. doi:10.25259/IJMSR_47_2020. ISSN 2582-3396. S2CID 244495353. Archived from the original on 2022-02-05. Retrieved 2022-06-05.
- Mueller-Weiss Syndrome Archived 2022-06-05 at the Wayback Machine
- "What is Mueller-Weiss Syndrome? Understanding Rafael Nadal's "Rare" and "Incurable" Foot Condition". Louisville Bones. 2022-02-25. Archived from the original on 2022-05-12. Retrieved 2022-06-05.
- "UpToDate". www.uptodate.com. Retrieved 2022-06-09.
- Prapto, Devindra; Dreyer, Mark A. (2022), "Anatomy, Bony Pelvis and Lower Limb, Navicular Bone", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31613455, retrieved 2022-06-07
- Cadogan, Mike; Gomez, Aparicio (2020-11-04). "Mueller–Weiss disease". Life in the Fast Lane • LITFL. Retrieved 2022-06-06.
- "What is Mueller Weiss disease?". ypsl. 2021-10-01. Retrieved 2022-06-06.
- Maciera, Ernesto (March 1, 2004). "Mueller-Weiss Syndrome". Foot and Ankle Clinics. 9: 105–125. Archived from the original on June 5, 2022. Retrieved June 5, 2022.
- Fondi, Cristina; Franchi, Alessandro (2007). "Definition of bone necrosis by the pathologist". Clinical Cases in Mineral and Bone Metabolism. 4 (1): 21–26. ISSN 1724-8914. PMC 2781178. PMID 22460748.
- Monteagudo, Manuel; MacEira, Ernesto (2019). "Management of Müller-Weiss Disease". Foot and Ankle Clinics. 24 (1): 89–105. doi:10.1016/j.fcl.2018.09.006. PMID 30685016. S2CID 59305670.
- Kani, Kimia Khalatbari; Mulcahy, Hyojeong; Chew, Felix S. (2016). "Case 228: Mueller-Weiss Disease". Radiology. 279 (1): 317–321. doi:10.1148/radiol.2016132280. PMID 26989931. S2CID 30160194. Case 228
- "Mueller-Weiss-syndrome | The Foot and Ankle Online Journal". Retrieved 2022-06-08.
- Haller, J.; Sartoris, D. J.; Resnick, D.; Pathria, M. N.; Berthoty, D.; Howard, B.; Nordstrom, D. (1988). "Spontaneous osteonecrosis of the tarsal navicular in adults: imaging findings". American Journal of Roentgenology. 151 (2): 355–358. doi:10.2214/ajr.151.2.355. ISSN 0361-803X. PMID 3260727.
- Volpe, Antonio; Monestier, Luca; Malara, Teresa; Riva, Giacomo; La Barbera, Giuseppe; Surace, Michele Francesco (2020-11-18). "Müller-Weiss disease: Four case reports". World Journal of Orthopedics. 11 (11): 507–515. doi:10.5312/wjo.v11.i11.507. ISSN 2218-5836. PMC 7672802. PMID 33269217.
- Mueller–Weiss syndrome, A Topical Review
- Joseph, Veena Mariam; Lynser, Donboklang; Khan, Aman Yusuf; Daniala, C. (2021-12-20). "Mueller Weiss syndrome, a less elucidated and unusual cause of midfoot pain: A case report". Indian Journal of Musculoskeletal Radiology. 3 (2): 94–97. doi:10.25259/IJMSR_47_2020. ISSN 2582-3396. S2CID 244495353.
- Prajwal Hegde (Jun 7, 2022). "Rafael Nadal seeks 'long-term' relief to fix his injuries | Tennis News - Times of India". The Times of India. Retrieved 2022-06-11.
- Harnroongroj, Thos; Tharmviboonsri, Theerawoot; Chuckpaiwong, Bavornrit (2021). "Müller-Weiss Disease: The Descriptive Factors of Failure Conservative Treatment". Foot & Ankle International. 42 (8): 1022–1030. doi:10.1177/10711007211002826. ISSN 1944-7876. PMID 33843318. S2CID 233214015.
- Clarey, Christopher (2022-06-06). "Nadal Has a Chance at Winning All 4 Grand Slams, if His Foot Cooperates". The New York Times. ISSN 0362-4331. Retrieved 2022-06-07.
- Russell, Lauren (2022-06-28). "Rafael Nadal: Star's 'rare' condition causing 'strange sensations' ahead of Wimbledon". Express.co.uk. Retrieved 2022-07-07.
- Train, Rob (2022-06-05). "What is Müller-Weiss syndrome, Rafa Nadal's chronic injury in his left foot?". Diario AS. Retrieved 2022-06-07.