Nager acrofacial dysostosis
Nager acrofacial dysostosis, also known as Nager syndrome, is a genetic disorder which displays several or all of the following characteristics: underdevelopment of the cheek and jaw area, down-sloping of the opening of the eyes, lack or absence of the lower eyelashes, kidney or stomach reflux, hammer toes, shortened soft palate, lack of development of the internal and external ear, possible cleft palate, underdevelopment or absence of the thumb, hearing loss (see hearing loss with craniofacial syndromes) and shortened forearms, as well as poor movement in the elbow, and may be characterized by accessory tragi.[3] Occasionally, affected individuals develop vertebral anomalies such as scoliosis.
| Nager acrofacial dysostosis | |
|---|---|
| Other names | Nager syndrome, mandibulofacial dysostosis with preaxial limb anomalies[1] |
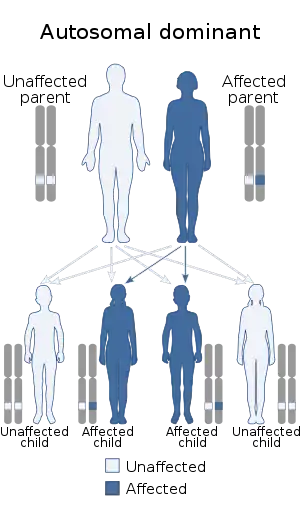 | |
| Nager acrofacial dysostosis is inherited in an autosomal dominant manner.[2] | |
The inheritance pattern is autosomal, but there are arguments as to whether it is autosomal dominant or autosomal recessive. Most cases tend to be sporadic. Nager syndrome shares many characteristics with five other craniofacial syndromes: Miller, Treacher Collins, Pierre Robin, Genee–Wiedemann and Franceschetti–Zwahlen–Klein.
Genetics
While Nager syndrome is thought to be most often caused by haploinsufficiency of the spliceosomal factor SF3B4,[4] in over one third of patients tested, the SF3B4 mutation is not found.[5] Genetic sequencing shows that the syndrome can be caused by either autosomal recessive or autosomal dominant inheritance. [6]
Treatment
Due to craniofacial development, it is recommended that families work closely with craniofacial specialists as soon as Nager is recognized or suspected. Children born with Nager may need intubation immediately after birth, requiring tube feeding and a tracheotomy tube to help with breathing. Surgical intervention is commonly necessary to increase mandibular mobility. As the child grows and develops, further surgery is usually required on the lower jaw and is often done in tandem with orthodontic treatments.[7] Further treatment depends upon the symptoms of the individual patient and may include oral surgery, plastic surgery, audiological intervention to manage hearing loss, speech therapy, and surgery on the limbs to aid with mobility limitations.[8]
See also
References
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Nager syndrome". www.orpha.net. Retrieved 27 April 2019.
- "OMIM Entry - # 154400 - ACROFACIAL DYSOSTOSIS 1, NAGER TYPE; AFD1". omim.org. Retrieved 19 August 2017.
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- Bernier FP, Caluseriu O, Ng S, Schwartzentruber J, Buckingham KJ, Innes AM, Jabs EW, Innis JW, Schuette JL, Gorski JL, Byers PH, Andelfinger G, Siu V, Lauzon J, Fernandez BA, McMillin M, Scott RH, Racher H, Majewski J, Nickerson DA, Shendure J, Bamshad MJ, Parboosingh JS (Apr 26, 2012). "Haploinsufficiency of SF3B4, a Component of the Pre-mRNA Spliceosomal Complex, Causes Nager Syndrome". American Journal of Human Genetics. 90 (5): 925–33. doi:10.1016/j.ajhg.2012.04.004. PMC 3376638. PMID 22541558.
- Zhao, Jue; Yang, Liwei (June 14, 2020). "Broad-spectrum next-generation sequencing-based diagnosis of a case of Nager syndrome". Journal of Clinical Laboratory Analysis. 34 (9): e23426. doi:10.1002/jcla.23426. PMC 7521291. PMID 32537850.
- Ibrahim, Rahaf; Eid, Nader (October 2021). "Possible autosomal recessive inheritance in a neonate with Nager syndrome: Case report". Annals of Medicine and Surgery. 70: 102896. doi:10.1016/j.amsu.2021.102896. PMC 8519802. PMID 34691433.
- "Plastic & Reconstructive Surgery: Nager syndrome". UCSF Benioff Children's Hospitals. Retrieved 31 October 2021.
- "Nager Syndrome". National Organization for Rare Disorders. Retrieved 31 October 2021.
External links