Pulmonary surfactant (medication)
Pulmonary surfactant is used as a medication to treat and prevent respiratory distress syndrome in newborn babies.[1]
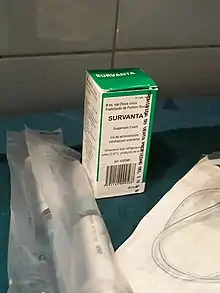 Beractant, surrounded by devices for its application. | |
| Clinical data | |
|---|---|
| Pronunciation | Curosurf, Survanta, others |
| Other names | Beractant, Poractant alfa, others |
| AHFS/Drugs.com | Monograph |
| License data | |
| ATC code | |
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
| UNII | |
Prevention is generally done in babies born at a gestational age of less than 32 weeks.[1] It is given by the endotracheal tube.[1] Onset of effects is rapid.[2] A number of doses may be needed.[2]
Side effects may include slow heart rate and low oxygen levels.[1] Its use is also linked with intracranial bleeding.[1] Pulmonary surfactant may be isolated from the lungs of cows or pigs or made artificially.[1][3][4]
Pulmonary surfactant was discovered in the 1950s and a manufactured version was approved for medical use in the United States in 1990.[3] It is on the World Health Organization's List of Essential Medicines.[5]
Medical uses
Pulmonary surfactant is used to treat and prevent respiratory distress syndrome in newborn babies.[1] Prevention is generally done in babies born less than 32 weeks gestational age.[1] Tentative evidence supports use in drowning.[6]
Surfactant administration can also be effective in meconium aspiration syndrome where it has been shown to help lower length of stay.[7][8]
For patients with acute respiratory distress syndrome (ARDS), surfactant has not been shown to reduce mortality. However, it may be beneficial in those with COVID-19 associated ARDS.[9][10]
Types
There are a number of types of pulmonary surfactants available. Like their natural counterparts, pulmonary surfactant preparations consist of phospholipids (mainly DPPC) combined with spreading agents such as SP-B and SP-C.[11] Ex-situ measurements of surface tension and interfacial rheology can help to understand the functionality of pulmonary surfactants.[12]
Synthetic pulmonary surfactants:
- Colfosceril palmitate (Exosurf) – a mixture of DPPC with hexadecanol and tyloxapol added as spreading agents
- Pumactant (Artificial Lung Expanding Compound or ALEC) – a mixture of DPPC and PG
- Lucinactant (KL-4) – composed of DPPC, palmitoyl-oleoyl phosphatidylglycerol, and palmitic acid, combined with a 21 amino acid synthetic peptide (sinapultide) that mimics the C-terminal helical domain of SP-B.[13]
- Ventricute - DPPC, rSP-C
- Lucinactant (trade name Surfaxin) is a liquid medication that contains DPPC, POPG as the sodium salt, and palmitic acid.
Animal-derived surfactants:
- Beractant (Survanta) – extracted from minced cow lung with additional DPPC, palmitic acid and tripalmitin, manufactured by Abbvie
- (Beraksurf) – extracted from minced cow lung with additional DPPC, palmitic acid and tripalmitin, manufactured by Tekzima
- Calfactant (Infasurf) – extracted from calf lung lavage fluid, manufactured by ONY Biotech.
- Poractant alfa (Curosurf) – extracted from material derived from minced pig lung
- Surfactant TA (Surfacten) – derived from cows, manufactured by Tokyo Tanabe Co. [14]
- Bovactant SF-RI (Alveofact) – extracted from cow lung lavage fluid, manufactured by Boehringer Ingelheim
History
Researcher John Clements identified surfactants and their role in the 1950s. Mary Ellen Avery soon after showed that the lungs of premature infants could not produce surfactants.[15]
Exosurf, Curosurf, Infasurf, and Survanta were the initial surfactants FDA approved for use in the U.S.[16]
In 2012, the US FDA approved an additional synthetic surfactant, lucinactant (Surfaxin).[17]
References
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 217. ISBN 9780857111562.
- Fanaroff, Avroy A.; Fanaroff, Jonathan M. (2013). Klaus and Fanaroff's Care of the High-Risk Neonate, Expert Consult - Online and Print,6: Klaus and Fanaroff's Care of the High-Risk Neonate. Elsevier Health Sciences. p. 252. ISBN 978-1416040019. Archived from the original on 2017-01-09.
- Lantos, John D.; Meadow, William L. (2006). Neonatal Bioethics: The Moral Challenges of Medical Innovation. JHU Press. pp. 54–56. ISBN 9780801883446. Archived from the original on 2017-01-09.
- Slonim, Anthony D.; Pollack, Murray M. (2006). Pediatric Critical Care Medicine. Lippincott Williams & Wilkins. pp. 724–725. ISBN 9780781794695. Archived from the original on 2017-01-09.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- Brady, Bill; Charlton, Nathan P.; Lawner, Benjamin J.; Sutherland, Sara F. (2012). Cardiac Arrest, An Issue of Emergency Medicine Clinics. Elsevier Health Sciences. p. 175. ISBN 978-1455742769. Archived from the original on 2017-01-09.
- El Shahed, Amr I.; Dargaville, Peter A.; Ohlsson, Arne; Soll, Roger (2014-12-14). "Surfactant for meconium aspiration syndrome in term and late preterm infants". The Cochrane Database of Systematic Reviews (12): CD002054. doi:10.1002/14651858.CD002054.pub3. ISSN 1469-493X. PMC 7027383. PMID 25504256.
- Walsh, Brian (2019). Neonatal and Pediatric Respiratory Care. Elsevier. pp. 244–261.
- Davidson, Warren J; Dorscheid, Del; Spragg, Roger; Schulzer, Michael; Mak, Edwin; Ayas, Najib T (2006). "Exogenous pulmonary surfactant for the treatment of adult patients with acute respiratory distress syndrome: results of a meta-analysis". Critical Care. 10 (2): R41. doi:10.1186/cc4851. ISSN 1364-8535. PMC 1550886. PMID 16542488.
- Heching, Moshe; Lev, Shaul; Shitenberg, Dorit; Dicker, Dror; Kramer, Mordechai R. (2021-07-01). "Surfactant for the Treatment of ARDS in a Patient With COVID-19". Chest. 160 (1): e9–e12. doi:10.1016/j.chest.2021.01.028. ISSN 0012-3692. PMC 7825915. PMID 33493441.
- Nkadi, Paul O.; Merritt, T. Allen; Pillers, De-Ann M. (2009). "An overview of pulmonary surfactant in the neonate: Genetics, metabolism, and the role of surfactant in health and disease". Molecular Genetics and Metabolism. 97 (2): 95–101. doi:10.1016/j.ymgme.2009.01.015. ISSN 1096-7192. PMC 2880575. PMID 19299177.
- Bertsch, Pascal; Bergfreund, Jotam; Windhab, Erich J.; Fischer, Peter (August 2021). "Physiological fluid interfaces: Functional microenvironments, drug delivery targets, and first line of defense". Acta Biomaterialia. 130: 32–53. doi:10.1016/j.actbio.2021.05.051. PMID 34077806. S2CID 235323337.
- "KL4 Surfactant Technology - Windtree Therapeutics, Inc". Windtree Therapeutics, Inc. Archived from the original on July 29, 2018. Retrieved 29 November 2017.
- Office, European Patent. "T 0723/94 (Surfactant composition/TOKYO TANABE CO) of 18.2.1999". www.epo.org. Retrieved 2022-04-30.
- Palca, Joe (3 August 2015). "How A Scientist's Slick Discovery Helped Save Preemies' Lives". NPR. Archived from the original on 3 August 2015. Retrieved 3 August 2015.
- Taeusch, H William; Lu, Karen; Ramierez-Schrempp, Daniela (2002). "Improving pulmonary surfactants" (PDF). Acta Pharmacologica Sinica. 23 Suppl: 11–5. Archived (PDF) from the original on 2015-03-01.
- "Drug Approval Package: Brand Name (Generic Name) NDA #". www.accessdata.fda.gov. Retrieved 2022-04-30.
External links
- "Poractant alfa". Drug Information Portal. U.S. National Library of Medicine.
- "Beractant". Drug Information Portal. U.S. National Library of Medicine.
- "Calfactant". Drug Information Portal. U.S. National Library of Medicine.