Testicular atrophy
Testicular atrophy is a medical condition in which one or both testicles (or "testes") diminish in size and may be accompanied by reduced testicular function.[1] Testicular atrophy is not related to the temporary shrinkage of the surrounding scrotum, which might occur in response to cold temperature.[1]

As the testicles are involved in testosterone and sperm production, the signs and symptoms of testicular atrophy overlap with those related to infertility or low testosterone levels.[2] In a prepubescent person with testicular atrophy, there may be underdevelopment of secondary sex characteristics (e.g. lack of penis growth).[3] In sexually developed individuals, testicular atrophy may be accompanied with lower sex drive and increased breast tissue.[2] Additional signs and symptoms vary and can depend on the specific cause of the testicle shrinkage. Some causes include age,[2] alcohol use,[4] hormone therapy,[3][5][6] direct damage to the testicles,[7][8] and infection.[9][10]
Diagnosis of testicular atrophy includes physical examination of the testicles as well as imaging to measure testicular volume.[8][11] A testosterone blood level is also taken to assess function of the testicles.[2] Additional tests may be ordered depending on the suspected cause(s) of the shrinkage.[1] Treatment and potential reversibility of testicular atrophy are also dependent on the cause.[1]
Signs and symptoms
There are different signs and symptoms associated with testicular atrophy depending on the person's age.[1] Symptoms before puberty are centered more around the stunting of sexual characteristics associated with hormonal changes, while symptoms after puberty include a wider range of factors. Other signs and symptoms may stem from underlying conditions which cause testicular atrophy. The most perceptible sign of testicular atrophy is shrinkage of the testicle(s).[12]
Signs and symptoms before puberty include:
- lack of development of pubic hair[1][12]
- lack of development of facial hair[1][12]
- lack of penis growth[1][12]
- lower testosterone[13]
Testosterone is a hormone that is found primarily in a portion of the male-assigned reproductive system called the testes and is normally measured in nanograms per deciliter. Testosterone is in charge of the growth and production of many sexual attributes in people with testes, including facial hair, pubic hair, penis size, vocal and muscle mass changes, regulation of sex drive, and sperm production. Normal testosterone levels in people with testes who have not yet hit puberty are less than 20 nanograms per deciliter. Low testosterone can be defined as hypogonadism in people with testes. Hypogonadism in people with testes is established as the hormonal inhibition of testosterone that can either be inherited or acquired at a later stage in life. Under the circumstances of pre-pubescent hypogonadism, many sexual developmental characteristics may be altered. Testosterone affects hair growth by regulating the follicle itself, which in turn affects the specific growth phases of the hair follicle. As a person with testes hits puberty, androgen, a steroid sex hormone, is produced at an increased rate, which creates terminal hair follicles. Terminal hair follicles create thicker and more pigmented hair which is also regulated by testosterone production. Testosterone also impacts pre-pubescent penis size by providing penile tissue with girth and density. The drop in testosterone values is mainly due to significant impairment of Leydig cells brought upon by hypogonadism. Leydig cells are located in the testes and serve to create testosterone and androgen. Once they are damaged, the production of testosterone is stunted.[14]
Signs and symptoms after puberty include:
- reduced sex drive[1]
- tender testicles[1]
- trouble conceiving[1]
- reduction of pubic or facial hair[1][12]
- decreased muscle mass[1]
- lower testosterone[13]
Typical testosterone levels of people with testes after puberty range from 300 to 1,200 nanograms per deciliter. Low testosterone values in people with testes post-puberty would be considered any value under 300 nanograms per deciliter. Decreased testosterone values caused by testicular atrophy can lead to and explain many of the signs and symptoms listed above, including a reduced sex drive, infertility, soft testicles, reduction of hair, and lower muscle mass throughout the body. Testosterone plays an important role in physiologically stimulating sex drive in people with testes. If testosterone levels drop below normal values, libido (sexual drive) is reduced, which can lead to the development of erectile dysfunction (a condition in which the penis is not able to get or stay erect).[15] This can indirectly affect fertility as well. In addition, testosterone is important in muscle mass formation. It increases the amount of lean muscle mass in the body. Testosterone encourages metabolic activity in the body, which in turn stimulates protein synthesis. Protein synthesis is highly important for the development and enlargement of muscle. Therefore, a lack of testosterone would alter this metabolic process, leading to a decrease in muscle mass.[16]
Signs and symptoms of testicular atrophy that are due to a secondary medical condition include:
Secondary medical conditions that may cause the signs and symptoms listed above include testicular cancer, chronic alcohol use, sexually transmitted infections, COVID-19, orchitis, varicoceles, or torsion of the testes.[9][12]
Causes
Age
Shrinkage of the testicles is common with advanced age, as overall reproductive function declines.[2][3]
Alcohol use
High alcohol usage lowers testosterone levels by direct damage to the Leydig cells (which produce testosterone) and by affecting hormones involved in signaling to the Leydig cells to produce testosterone.[4] As a result, testicular atrophy is a common feature among individuals with high alcohol use.[4] Testicular malformations and low testosterone levels is also commonly found in people with alcoholic cirrhosis as the negative effect of alcohol use is worsened by the liver damage itself.[4] Excessive alcohol intake can cause inflammation and the degradation of cells in the liver, which can then cause testicular abnormalities (including testicular atrophy).[17]
Anabolic steroid use and hormone therapy
Anabolic steroid use and testosterone replacement therapy (TRT) have been found to cause testicular atrophy through similar mechanisms.[3][2][18] Anabolic steroids and TRT are both used (either by prescription or illicitly) to mimic the effects of testosterone produced by the body, such as building muscle and maintaining sex drive.[18][2][3] However, they also inhibit the body's own production of sperm and testosterone, which can lead to shrinkage of the testicles.[18][5]
Testicular atrophy is also a side effect of estrogen therapy.[6]
COVID-19
COVID-19 can lead to reduced testosterone production and testicular abnormalities due to changes in the secretion of gonadotropins, which are hormones involved in regulating testosterone production. These hormonal effects may be due to inflammation and oxidative stress caused by COVID-19. This might inform whether healthcare providers decide to monitor those who have survived COVID-19 for hormonal changes and potential fertility issues.[9][19]
Orchitis
Orchitis, or inflammation of the testicles due to a bacterial or viral infection, can lead to testicular atrophy.[10] Mumps has historically been significantly associated with orchitis and testicular atrophy, but has become rare in countries that have high mumps vaccination rates.[10]
Varicoceles and testicular torsion
Varicoceles and testicular torsion are conditions in which direct damage to the testicles can potentially lead to testicular atrophy.[7][8] Varicoceles are pooling of blood in the veins that deliver blood away from the testicles and are relatively common, occurring in approximately 15% of adolescent and adults with testicles.[8] Currently, it is not clearly established how often varicoceles actually become a direct cause of issues related to fertility.[8] Testicular torsion is the twisting of the testicle within the scrotum and can rapidly result in damage due to interruption in blood flow to the affected testicle.[7] Unlike varicoceles,[20] testicular torsion is considered a medical emergency.[7]
Other health conditions
There is a possible correlation of cystic fibrosis and its impact to bilateral testicular atrophy. Cystic fibrosis is a disease which causes mucus buildup in various organs.[21] Evidence has shown that cystic fibrosis affects multiple systems in the human body, including the reproductive system. Around 97-98% of people with cystic fibrosis who have testicles are infertile due to a missing vas deferens, the tube in the male-assigned reproductive system that carries sperm out of the testes.[22][23] Additionally, cystic fibrosis can result in the atrophy of male-assigned reproductive organs by causing dehydrated secretions.
Diagnosis
Physical examination
A healthcare provider may initially assess size and shape as well as firmness and texture of the testicles.[1][20][8]
Ultrasonography
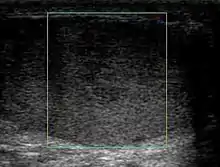
Ultrasonography is used to detect testicular volume. Testicular volume measured to be less than 12 mL is a sign of testicular atrophy.[11] In addition, testicular atrophy can be recognized as greater than 50% loss of testicular volume or a post-operative testicle with less than 25% of the volume of the opposite testicle.[24]
Lab tests
Assessment of testicular function is also dependent on lab tests. Low testosterone is a potential cause of testicular atrophy, and laboratory values of blood samples can confirm low free or bioavailable testosterone.[25]
Due to the high levels of oxidative stress in the semen, there may also be higher levels of sperm DNA fragmentation for people with varicoceles. In some cases, people with testicular damage who do not undergo repair of the varicoceles will have testicular atrophy.[26]
Treatment
Medication
Treatment with selective estrogen receptor modulators (SERMs) alone or in addition to self-administered injections of hCG aim to correct hormonal imbalances caused by anabolic steroid use and can help prevent or reverse testicular atrophy for some people.[5]
Surgery
People who have testicular atrophy due to testicular torsion are immediately referred to surgery regardless of the ultrasound findings, since delays rapidly decrease the rate of recovery. The consequences of not treating will result in decreased fertility and may result in the need of an orchiectomy, a surgical procedure to remove one or both testicles.[27] While immediate treatment can reduce the recovery time for the testes, there is still a chance of the testes to undergo atrophy a second time. Performance of an orchiectomy on individuals diagnosed with testicular atrophy has a possible negative impact on their testosterone levels in the long term. As a result, these individuals are typically monitored for the reoccurrence of testicular atrophy and low testosterone levels.[28]
Lifestyle modifications
In addition to drug therapies and surgical interventions to treat testicular atrophy, lifestyle modifications might also be recommended by healthcare providers.[29] Most lifestyle modifications target factors that contribute to infertility in people with testes. Limiting or abstaining from alcohol intake, smoking, and drugs such as anabolic steroids, cannabis, or opioids can help with infertility. Additionally, diet modifications might be encouraged to reach a more balanced diet, such as a higher intake of fish, fruits, vegetables, nuts, seeds, whole grains, and healthier oils, such as olive oil and canola oil.[30] Reducing intake of red meats, processed meats, and saturated and trans fats can also lead to improved fertility outcomes. Poor diet can otherwise lead to oxidative stress, which causes sperm damage, leading to lower testicular volume and lower sperm quality. Ensuring enough vitamin and mineral intake might also be recommended, since omega-3 fatty acids, antioxidant vitamins, zinc, and selenium might help reduce the damage by oxidative stress and reduce inflammation. Zinc intake can be boosted with meats and nuts, and selenium intake can be boosted with whole grains.[31]
See also
- Testicular nubbin
References
- Citroner G (2017). Biggers A (ed.). "Testicular Atrophy: Symptoms, Causes, and Treatment". Healthline. Retrieved 25 July 2022.
- Ramos L, Patel AS, Ramasamy R (2018). "Testosterone replacement therapy for physician assistants and nurse practitioners". Translational Andrology and Urology. 7 (Suppl 1): S63–S71. doi:10.21037/tau.2017.12.09. PMC 5881199. PMID 29644169.
- Seal LJ (2013). "Male hypogonadism and testosterone replacement therapy". Medicine. 41 (10): 557–561. doi:10.1016/j.mpmed.2013.07.010 – via Elsevier ScienceDirect.
- Karagiannis A, Harsoulis F (2005). "Gonadal dysfunction in systemic diseases". European Journal of Endocrinology. 152 (4): 501–513. doi:10.1530/eje.1.01886. PMID 15817904.
- Rahnema CD, Lipshultz LI, Crosnoe LE, Kovac JR, Kim ED (2014). "Anabolic steroid-induced hypogonadism: diagnosis and treatment". Fertility and Sterility. 101 (5): 1271–1279. doi:10.1016/j.fertnstert.2014.02.002. PMID 24636400.
- Cheng PJ, Pastuszak AW, Myers JB, Goodwin IA, Hotaling JM (2019). "Fertility concerns of the transgender patient". Translational Andrology and Urology. 8 (3): 209–218. doi:10.21037/tau.2019.05.09. PMC 6626312. PMID 31380227.
- DaJusta DG, Granberg CF, Villanueva C, Baker LA (2013). "Contemporary review of testicular torsion: new concepts, emerging technologies and potential therapeutics". Journal of Pediatric Urology. 9 (6 Pt A): 723–730. doi:10.1016/j.jpurol.2012.08.012. PMC 3566290. PMID 23044376.
- Garcia-Roig ML, Kirsch AJ (2015). "The dilemma of adolescent varicocele". Pediatric Surgery International. 31 (7): 617–625. doi:10.1007/s00383-015-3698-8. PMID 25895069.
- Selvaraj K, Ravichandran S, Krishnan S, Radhakrishnan RK, Manickam N, Kandasamy M (October 2021). "Testicular Atrophy and Hypothalamic Pathology in COVID-19: Possibility of the Incidence of Male Infertility and HPG Axis Abnormalities". Reproductive Sciences. 28 (10): 2735–2742. doi:10.1007/s43032-020-00441-x. PMC 7790483. PMID 33415647.
- Fijak M, Pilatz A, Hedger MP, Nicolas N, Bhushan S, Michel V, et al. (2018). "Infectious, inflammatory and 'autoimmune' male factor infertility: how do rodent models inform clinical practice?". Human Reproduction Update. 24 (4): 416–441. doi:10.1093/humupd/dmy009. PMC 6016649. PMID 29648649.
- Pedersen MR, Osther PJ, Rafaelsen SR (2018). "Ultrasound Evaluation of Testicular Volume in Patients with Testicular Microlithiasis". Ultrasound International Open. 4 (3): E99–E103. doi:10.1055/a-0643-4524. PMC 6143373. PMID 30250943.
- Fletcher J (2018). Murrell D (ed.). "Testicular atrophy: Causes, diagnosis, and treatment". Medical News Today. Retrieved 25 July 2022.
- Misra M, Lee MM (2005). "Delayed puberty". Pediatric Endocrinology. Mosby. pp. 87–101. doi:10.1016/B978-0-323-01825-8.50035-1. ISBN 978-0-323-01825-8.
- Calabria A (2020). "Male Hypogonadism in Children - Pediatrics". Merck Manuals Professional Edition. Retrieved 1 August 2022.
- Hoffman M (2021). "Low Testosterone and Your Sex Drive". WebMD. Retrieved 2 August 2022.
- Griggs RC, Kingston W, Jozefowicz RF, Herr BE, Forbes G, Halliday D (January 1989). "Effect of testosterone on muscle mass and muscle protein synthesis". Journal of Applied Physiology. 66 (1): 498–503. doi:10.1152/jappl.1989.66.1.498. PMID 2917954.
- Medicover Hospitals (2021). "Testicular Atrophy Symptoms: Causes, Types, Treatments and Home Remedies". Medicover Hospitals. Retrieved 28 July 2022.
- Moss JL, Crosnoe LE, Kim ED (2013). "Effect of rejuvenation hormones on spermatogenesis". Fertility and Sterility. 99 (7): 1814–1820. doi:10.1016/j.fertnstert.2013.04.003. PMID 23663992.
- Mieusset R, Bujan L, Plantavid M, Grandjean H (February 1989). "Increased levels of serum follicle-stimulating hormone and luteinizing hormone associated with intrinsic testicular hyperthermia in oligospermic infertile men". The Journal of Clinical Endocrinology and Metabolism. 68 (2): 419–425. doi:10.1210/jcem-68-2-419. PMID 2493031.
- Macey MR, Owen RC, Ross SS, Coward RM (2018). "Best practice in the diagnosis and treatment of varicocele in children and adolescents". Therapeutic Advances in Urology. 10 (9): 273–282. doi:10.1177/1756287218783900. PMC 6088496. PMID 30116303.
- "About Cystic Fibrosis | Cystic Fibrosis Foundation". Cystic Fibrosis Foundation. Retrieved 1 August 2022.
- Profka E, Rodari G, Giacchetti F, Berrettini A, Manzoni G, Daccò V, et al. (2020). "A case of testicular atrophy associated with cystic fibrosis". Endocrinology, Diabetes & Metabolism Case Reports. 2020: 20–0095. doi:10.1530/EDM-20-0095. PMC 7576656. PMID 33434179.
- "Definition of vas deferens". National Cancer Institute. 2011. Retrieved 1 August 2022.
- Durell J, Johal N, Burge D, Wheeler R, Griffiths M, Kitteringham L, et al. (2016). "Testicular atrophy following paediatric primary orchidopexy: A prospective study". Journal of Pediatric Urology. 12 (4): 243.e1-243.e4. doi:10.1016/j.jpurol.2016.05.023. PMID 27422375.
- Winters SJ (2000). "Laboratory Assessment of Testicular Function". In Feingold KR, Anawalt B, Boyce A, Chrousos G (eds.). Endotext. South Dartmouth (MA): MDText.com, Inc. PMID 25905368. Retrieved 26 July 2022.
- Kavoussi PK, Abdullah N, Gilkey MS, Hunn C, Machen GL, Chen SH, et al. (2021). "The impact of ipsilateral testicular atrophy on semen quality and sperm DNA fragmentation response to varicocele repair". Asian Journal of Andrology. 23 (2): 146–149. doi:10.4103/aja.aja_50_20. PMC 7991813. PMID 32930104.
- Sharp VJ, Kieran K, Arlen AM (2013). "Testicular torsion: diagnosis, evaluation, and management". American Family Physician. 88 (12): 835–840. PMID 24364548.
- Aggarwal D, Parmar K, Sharma AP, Tyagi S, Kumar S, Singh SK, Gupta S (2022). "Long-term impact of testicular torsion and its salvage on semen parameters and gonadal function". Indian Journal of Urology. 38 (2): 135–139. doi:10.4103/iju.iju_328_21. PMC 8992720. PMID 35400863.
- Leisegang K, Dutta S (2021). "Do lifestyle practices impede male fertility?". Andrologia. 53 (1): e13595. doi:10.1111/and.13595. PMID 32330362.
- Skoracka K, Eder P, Łykowska-Szuber L, Dobrowolska A, Krela-Kaźmierczak I (2020). "Diet and Nutritional Factors in Male (In)fertility-Underestimated Factors". Journal of Clinical Medicine. 9 (5): 1400. doi:10.3390/jcm9051400. PMC 7291266. PMID 32397485.
- Olza J, Aranceta-Bartrina J, González-Gross M, Ortega RM, Serra-Majem L, Varela-Moreiras G, Gil Á (2017). "Reported Dietary Intake and Food Sources of Zinc, Selenium, and Vitamins A, E and C in the Spanish Population: Findings from the ANIBES Study". Nutrients. 9 (7): 697. doi:10.3390/nu9070697. PMC 5537812. PMID 28684689.