Transmission-based precautions
Transmission-based precautions are infection-control precautions in health care, in addition to the so-called "standard precautions". They are the latest routine infection prevention and control practices applied for patients who are known or suspected to be infected or colonized with infectious agents, including certain epidemiologically important pathogens, which require additional control measures to effectively prevent transmission.[1][2] Universal precautions are also important to address as far as transmission-based precautions. Universal precautions is the practice of treating all bodily fluids as if it is infected with HIV, HBV, or other blood borne pathogens.[3]
Transmission-based precautions build on the so-called "standard precautions" which institute common practices, such as hand hygiene, respiratory hygiene, personal protective equipment protocols, soiled equipment and injection handling, patient isolation controls and risk assessments to limit spread between patients.[4]
History
The following table shows the history of guidelines for transmission-based precautions in U.S. hospitals as of 2007:[1]
| Year | Document issued | Comment |
| 1970[5] | Isolation Technique for Use in Hospitals, 1st ed. | Introduced seven isolation precaution categories with color-coded cards: Strict, Respiratory, Protective, Enteric, Wound and Skin, Discharge, and Blood. No user decision-making required. Simplicity a strength; over isolation prescribed for some infection. |
| 1975[6] | Isolation Techniques for Use in Hospitals, 2nd ed. | Same conceptual framework as 1st edition. |
| 1983[6] | CDC Guideline for Isolation Precautions in Hospitals | Provided two systems for isolation: category-specific and disease-specific. Protective Isolation eliminated; Blood Precautions expanded to include Body Fluids. Categories included Strict, Contact, Respiratory, AFB, Enteric, Drainage/Secretion, Blood and Body Fluids. Emphasized decision-making by users. |
| 1985-88[7][8] | Universal precautions | Developed in response to HIV/AIDS epidemic. Dictated application of Blood and Body Fluid precautions to all patients, regardless of infection status. Did not apply to feces, nasal secretions, sputum, sweat, tears, urine, or vomitus unless contaminated by visible blood. Added personal protective equipment to protect health care workers from mucous membrane exposures. Handwashing recommended immediately after glove removal. Added specific recommendations for handling needles and other sharp devices; concept became integral to OSHA's 1991 rule on occupational exposure to blood-borne pathogens in healthcare settings. |
| 1987[9] | Body substance isolation | Emphasized avoiding contact with all moist and potentially infectious body substances except sweat even if blood not present. Shared some features with Universal Precautions. Weak on infections transmitted by large droplets or by contact with dry surfaces. Did not emphasize need for special ventilation to contain airborne infections. Handwashing after glove removal not specified in the absence of visible soiling. |
| 1996[10] | Guideline for Isolation Precautions in Hospitals | Prepared by the Healthcare Infection Control Practices Advisory Committee (HICPAC). Melded major features of Universal Precautions and Body Substance Isolation into standard precautions to be used with all patients at all times. Included three transmission-based precaution categories: airborne, droplet, and contact . Listed clinical syndromes that should dictate use of empiric isolation until an etiological diagnosis is established. |
Rationale for use in healthcare setting
Communicable diseases occur as a result of the interaction between a source (or reservoir) of infectious agents, a mode of transmission for the agent, a susceptible host with a portal of entry receptive to the agent, the environment. The control of communicable diseases may involve changing one or more of these components, the first three of which are influenced by the environment. These diseases can have a wide range of effects, varying from silent infection – with no signs or symptoms – to severe illness and death. According to its nature, a certain infectious agent may demonstrate one or more following modes of transmission direct and indirect contact transmission, droplet transmission and airborne transmission.[11]
Transmission-based precautions are used when the route(s) of transmission is (are) not completely interrupted using "standard precautions" alone.
Standard precautions
Standard precautions include:[4]
- Hand hygiene or hand washing to prevent oneself from contracting an illness or disease and preventing the spread of pathogens (e.g. bacteria, viruses, parasites) to other people, thus reducing the potential for transmission. Hand hygiene can be accomplished with different modalities including alcohol-based hand sanitizers, soap and water, or antiseptic hand wash. There are techniques and benefits to using one modality over another. Utilization of alcohol-based hand sanitizer is generally recommended when the hands are not visibly soiled or before and after contact with a person (e.g. patient in a healthcare setting), or object. With proper technique, soap and water is preferred for visibly soiled hands or in situations where hands various pathogens cannot be killed with alcohol-based hand sanitizers (e.g. spore producing organisms like clostridium difficile).[12]
- personal protective equipment (PPE) in cases of infectious material exposure etiquette,
- respiratory hygiene principles,
- patient isolation controls,
- soiled equipment handling,
- and injection handling.
Research
Research studies in the form of randomized controlled trials and simulation studies are needed to determine the most effective types of personal protective equipment for preventing the transmission of infectious diseases to healthcare workers. There is low quality evidence that supports making improvements or modifications to personal protective equipment in order to help decrease contamination.[13] Examples of modifications include adding tabs to masks or gloves to ease removal and designing protective gowns so that gloves are removed at the same time. In addition, there is weak evidence that the following PPE approaches or techniques may lead to reduced contamination and improved compliance with PPE protocols: Wearing double gloves, following specific doffing (removal) procedures such as those from the CDC, and providing people with spoken instructions while removing PPE.[13]
Definitions
Three categories of transmission-based precautions have been designed with respect to the modes of transmission, namely Contact precautions, Droplet precautions, and Airborne precautions. For some diseases with multiple routes of transmission, more than one transmission-based precautions category may be used. When used either singly or in combination, they are always used in addition to standard precautions.[1]
Contact precautions

Contact precautions are intended to prevent transmission of infectious agents, including epidemiologically important microorganisms, which are spread by direct or indirect contact with the patient or the patient's environment. The specific agents and circumstance for which contact precautions are indicated are found in Appendix A of the 2007 CDC Guidance.[1] The application of contact precautions for patients infected or colonized with Multidrug-Resistant Organisms MDROs is described in the 2006 HICPAC/CDC MDRO guideline.[14] Contact precautions also apply where the presence of excessive wound drainage, fecal incontinence, or other discharges from the body suggest an increased potential for extensive environmental contamination and risk of transmission. A single-patient room is preferred for patients who require contact precautions. When a single-patient room is not available, consultation with infection control personnel is recommended to assess the various risks associated with other patient placement options (e.g., cohorting, keeping the patient with an existing roommate). In multi-patient rooms, >3 feet spatial separation between beds is advised to reduce the opportunities for inadvertent sharing of items between the infected/colonized patient and other patients. Healthcare personnel caring for patients on contact precautions wear a gown and gloves for all interactions that may involve contact with the patient or potentially contaminated areas in the patient's environment. Donning PPE upon room entry and discarding before exiting the patient room is done to contain pathogens, especially those that have been implicated in transmission through environmental contamination (e.g., VRE, C. difficile, noroviruses and other intestinal tract pathogens; RSV)[15][16][17][18][19][20][21]
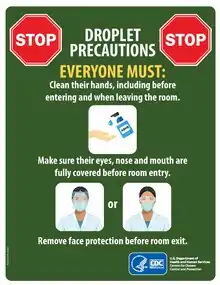
Droplet precautions
As of 2020, the classification systems of routes of respiratory disease transmission are based on a conceptual division of large versus small droplets, as defined in the 1930s.[22]
Droplet precautions are intended to prevent transmission of certain pathogens spread through close respiratory or mucous membrane contact with respiratory secretions, namely respiratory droplets. Because certain pathogens do not remain infectious over long distances in a healthcare facility, special air handling and ventilation are not required to prevent droplet transmission. Infectious agents for which mere droplet precautions are indicated include B. pertussis, influenza virus, adenovirus, rhinovirus, N. meningitidis, and group A streptococcus (for the first 24 hours of antimicrobial therapy). A single patient room is preferred for patients who require droplet precautions. When a single-patient room is not available, consultation with infection control personnel is recommended to assess the various risks associated with other patient placement options (e.g., cohorting, keeping the patient with an existing roommate). Spatial separation of > 3 feet and drawing the curtain between patient beds is especially important for patients in multi-bed rooms with infections transmitted by the droplet route. Healthcare personnel wear a simple mask (a respirator is not necessary) for close contact with an infectious patient, which is generally donned upon room entry. Patients on droplet precautions who must be transported outside of the room should wear a mask if tolerated and follow Respiratory Hygiene/Cough Etiquette.
Airborne precautions
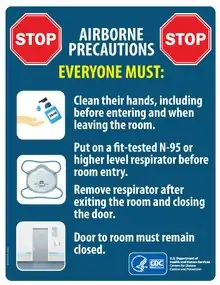
Airborne precautions prevent transmission of infectious agents that remain infectious over long distances when suspended in the air (e.g., rubeola virus [measles], varicella virus [chickenpox], M. tuberculosis, and possibly SARS-CoV). The preferred placement for patients who require airborne precautions is in an airborne infection isolation room (AIIR). An AIIR is a single-patient room that is equipped with special air handling and ventilation capacity that meet the American Institute of Architects/Facility Guidelines Institute (AIA/FGI) standards for AIIRs (i.e., monitored negative pressure relative to the surrounding area,[23] air exchanges per hour for new construction and renovation and 6 air exchanges per hour for existing facilities, air exhausted directly to the outside or recirculated through HEPA filtration before return).[24] The Airborne Infectious Isolation Rooms are designed for prevention against the airborne diseases. They have their predefined Heating, Ventilation and Air conditioning (HVAC) criteria given by CDC, IDPH and ASHRAE Standard 170. CDC regulations only specify 12 ach (air changes per hour) and do not have any criteria on temperature or humidity. Meanwhile, IDPH/ASHRAE Standard 170 has more detailed design criteria for HVAC systems. According to their regulations the isolation rooms must have the ability to maintain the room temperature around 70F to 75F, while keeping the relative humidity (rh) to be minimum of 30% during winters and maximum of 60% during summers. The specified airflow is 12 ach total/ 2 ach OA (Outdoor Air) and the pressure should be negative relative to the adjacent spaces. There are some architectural design requirements for the rooms such as walls should be slab to slab, plaster or drywall ceilings with sliding-self-closing doors are preferred with all the leakages sealed.[25] The guidelines specified by CDC, IDPH/ASHRAE Standard 170 are focused on maintaining room temperatures within specified range, one thing to look into these conditions is how the relative humidity plays a role to effect the cooling systems used for maintaining the stringent temperature requirements. While the places with low relative humidity are perfectly fine with the evaporative cooling systems used in HVAC systems, but as the relative humidity pushes towards the higher ranges i.e. more than 60%, then the evaporative cooling systems fail miserably and have to be replaced with the refrigerated cooling systems. This is to be done to prevent the corrosive action of the moisture saturated on the corrosive surfaces of isolation rooms because evaporative cooling being slow in higher relative humidity areas will allow the more contact time between moisture and corrosive surfaces. For example, during the annual monsoon season in Arizona the cooling is going to be adversely affected due to high relative humidity.[26]
Some states require the availability of such rooms in hospitals, emergency departments, and nursing homes that care for patients with M. tuberculosis. A respiratory protection program that includes education about use of respirators, fit-testing, and user seal checks is required in any facility with AIIRs. In settings where airborne precautions cannot be implemented due to limited engineering resources (e.g., physician offices), masking the patient, placing the patient in a private room (e.g., office examination room) with the door closed, and providing N95 or higher level respirators or masks if respirators are not available for healthcare personnel will reduce the likelihood of airborne transmission until the patient is either transferred to a facility with an AIIR or returned to the home environment, as deemed medically appropriate. Healthcare personnel caring for patients on airborne precautions wear a mask or respirator, depending on the disease-specific recommendations (Appendix A),[1] that is donned prior to room entry. Whenever possible, non-immune HCWs should not care for patients with vaccine-preventable airborne diseases (e.g., measles, chickenpox, and smallpox).
Syndromic and empirical use
Since the infecting agent often is not known at the time of admission to a healthcare facility, transmission-based precautions are used empirically, according to the clinical syndrome and the likely etiologic agents at the time, and then modified when the pathogen is identified or a transmissible infectious etiology is ruled out. Diagnosis of many infections requires laboratory confirmation. Since laboratory tests, especially those that depend on culture techniques, often require two or more days for completion, transmission-based precautions must be implemented while test results are pending based on the clinical presentation and likely pathogens. Use of appropriate transmission-based precautions at the time a patient develops symptoms or signs of transmissible infection, or arrives at a healthcare facility for care, reduces transmission opportunities. While it is not possible to identify prospectively all patients needing transmission-based precautions, certain clinical syndromes and conditions carry a sufficiently high risk to warrant their use empirically while confirmatory tests are pending.[1]
| Clinical syndrome or condition¹ | Potential pathogens² | Empiric precautions (always include standard precautions) |
| Acute diarrhea with a likely infectious cause in an incontinent or diapered patient | Enteric pathogens include enterohemorrhagic Escherichia coli O157:H7, Shigella spp, hepatitis A virus, noroviruses, rotavirus, C. difficile | Contact precautions (pediatrics and adult) |
| Meningitis | Neisseria meningitidis | Droplet precautions for first 24 hrs of antimicrobial therapy; mask and face protection for intubation |
| Meningitis | Enteroviruses M. tuberculosis | Contact precautions for infants and children |
| Meningitis | M. tuberculosis | Airborne precautions if pulmonary infiltrate
Airborne precautions plus contact precautions if potentially infectious draining body fluid present |
| RASH OR EXANTHEMS, GENERALIZED, ETIOLOGY UNKNOWN | ||
| Petechial/ecchymotic with fever (general) | Neisseria meningitidis | Droplet precautions for first 24 hrs of antimicrobial therapy |
| Ebola, Lassa, Marburg viruses | Droplet precautions plus contact precautions, with face/eye protection, emphasizing safety sharps and barrier precautions when blood exposure likely. Use N95 or higher respiratory protection when aerosol-generating procedure performed | |
| Vesicular | Varicella-zoster, herpes simplex, variola | Airborne plus contact precautions; |
| Vesicular | (smallpox), vaccinia viruses | Contact precautions only if herpes simplex, localized zoster in an immunocompetent host or vaccinia viruses most likely |
| Maculopapular with cough, coryza and fever | Rubeola (measles) virus | Airborne precautions |
| RESPIRATORY INFECTIONS | ||
| Cough/fever/upper lobe pulmonary infiltrate in an HIV-negative patient or a patient at low risk for human immunodeficiency virus (HIV) infection | M. tuberculosis, Respiratory viruses, S. pneumoniae, S. aureus (MSSA or MRSA) | Airborne precautions plus contact precautions |
| Cough/fever/pulmonary infiltrate in any lung location in an HIV-infected patient or a patient at high risk for HIV infection | M. tuberculosis, Respiratory viruses, S. pneumoniae, S. aureus (MSSA or MRSA) | Airborne precautions plus contact precautions. Use eye/face protection if aerosol-generating procedure performed or contact with respiratory secretions anticipated.
If tuberculosis is unlikely and there are no AIIRs and/or respirators available, use droplet precautions instead of airborne precautions Tuberculosis more likely in HIV-infected individual than in HIV-negative individual |
| Cough/fever/pulmonary infiltrate in any lung location in a patient with a history of recent travel (10–21 days) to countries with active outbreaks of SARS, avian influenza | M. tuberculosis, severe acute respiratory syndrome virus (SARS-CoV), avian influenza | Airborne plus contact precautions plus eye protection.
If SARS and tuberculosis unlikely, use droplet precautions instead of airborne precautions. |
| Respiratory infections, particularly bronchiolitis and pneumonia, in infants and young children | Respiratory syncytial virus, parainfluenza virus, adenovirus, influenza virus, Human metapneumovirus | Contact plus droplet precautions; droplet precautions may be discontinued when adenovirus and influenza have been ruled out. |
| Skin or Wound Infection | ||
| Abscess or draining wound that cannot be covered | Staphylococcus aureus (MSSA or MRSA), group A streptococcus | Contact precautions. Add droplet precautions for the first 24 hours of appropriate antimicrobial therapy if invasive Group A streptococcal disease is suspected. |
¹ Patients with the syndromes or conditions listed below may present with atypical signs or symptoms (e.g.neonates and adults with pertussis may not have paroxysmal or severe cough). The clinician's index of suspicion should be guided by the prevalence of specific conditions in the community, as well as clinical judgment.
² The organisms listed under the column "Potential pathogens" are not intended to represent the complete, or even most likely, diagnoses, but rather possible etiologic agents that require additional precautions beyond standard precautions until they can be ruled out.
Recommendations for specific infections
Following are recommendations for transmission-based precautions for specific infections per the US Healthcare Infection Control Practices Advisory Committee as of 2007.[1]
| Infection or condition | Precautions type¹ | Precautions duration² | Precautions comments |
| Abscess draining, major | C | DI | No dressing or containment of drainage; until drainage stops or can be contained by dressing |
| Clostridium difficile | C | DI | Discontinue antibiotics if appropriate. Do not share electronic thermometers;[27][28] ensure consistent environmental cleaning and disinfection. Hypochlorite solutions may be required for cleaning if transmission continues.[29] Handwashing with soap and water preferred because of the absence of sporicidal activity of alcohol in waterless antiseptic handrubs[30] |
| Acute viral (acute hemorrhagic) | C | DI | Adenovirus most common; enterovirus,[31][32] Coxsackie virus A[33][34]) also associated with community outbreaks. Highly contagious; outbreaks in eye clinics, pediatric and neonatal settings, institutional settings reported. Eye clinics should follow standard precautions when handling patients with conjunctivitis. Routine use of infection control measures in the handling of instruments and equipment will prevent the occurrence of outbreaks in this and other settings.[35][36][37][38][39][40] |
| Diphtheria pharyngeal | D | CN | Until 2 cultures taken 24 hrs. apart negative |
| Diphtheria cutaneous | C | CN | Until 2 cultures taken 24 hrs. apart negative |
| Furunculosis, staphylococcal Infants and young children | C | DI | |
| Rotavirus | C | DI | Ensure consistent environmental cleaning and disinfection and frequent removal of soiled diapers. Prolonged shedding may occur in both immunocompetent and immunocompromised children and the elderly[41][42] |
| Hepatitis, viral Type A Diapered or incontinent patients | C | Maintain contact precautions in infants and children <3 years of age for duration of hospitalization; for children 3-14 yrs. of age for 2 weeks after onset of symptoms; >14 yrs. of age for 1 week after onset of symptoms.[43][44][45] | |
| Herpes zoster (varicella-zoster) (shingles) Disseminated disease in any patient
Localized disease in immunocompromised patient until disseminated infection ruled out |
A,C | DI | Susceptible HCWs should not enter room if immune caregivers are available; no recommendation for protection of immune HCWs; no recommendation for type of protection, i.e. surgical mask or respirator; for susceptible HCWs. |
| Impetigo | C | U24 hrs | |
| Influenza human (seasonal influenza) | D | 5 days except DI in immunocompromised persons | Single patient room when available or cohort; avoid placement with high-risk patients; mask patient when transported out of room; chemoprophylaxis/vaccine to control/prevent outbreaks.[46] Use gown and gloves according to standard precautions may be especially important in pediatric settings. Duration of precautions for immunocompromised patients cannot be defined; prolonged duration of viral shedding (i.e. for several weeks) has been observed; implications for transmission are unknown.[47] |
| Influenza Avian (e.g. H5N1, H7, H9 strains) | See www.cdc.gov/flu/avian/professional/infect-control.htm for current avian influenza guidance. | ||
| Pandemic influenza (also a human influenza virus) | D | 5 days from onset of symptoms | See http://www.pandemicflu.gov for current pandemic influenza guidance. |
| Lice head (pediculosis) | C | U 24 hrs | |
| Measles (rubeola) | A | 4 days after onset of rash; DI in immune compromised | Susceptible HCWs should not enter room if immune care providers are available; no recommendation for face protection for immune HCW; no recommendation for type of face protection for susceptible HCWs, i.e., mask or respirator.[48][49] For exposed susceptibles, post-exposure vaccine within 72 hrs. or immune globulin within 6 days when available.[50][51][52] Place exposed susceptible patients on Airborne precautions and exclude susceptible health care personnel from duty from day 5 after first exposure to day 21 after last exposure, regardless of post-exposure vaccine.[50] |
| Monkeypox | A,C | A-Until monkeypox confirmed and smallpox excluded C-Until lesions crusted | Use See www.cdc.gov/ncidod/monkeypox for most current recommendations. Transmission in hospital settings unlikely.[53] Pre- and post-exposure smallpox vaccine recommended for exposed HCWs |
| Multidrug-resistant organisms (MDROs), infection or colonization (e.g., MRSA, VRE, VISA/VRSA, ESBLs, resistant S. pneumoniae) | S/C | MDROs judged by the infection control program, based on local, state, regional, or national recommendations, to be of clinical and epidemiologic significance. Contact precautions recommended in settings with evidence of ongoing transmission, acute care settings with increased risk for transmission or wounds that cannot be contained by dressings. See recommendations for management options in Management of Multidrug-Resistant Organisms In Healthcare Settings, 2006.[54] Contact state health department for guidance regarding new or emerging MDRO. | |
| Mumps (infectious parotitis) | D | U 9 days | After onset of swelling; susceptible HCWs should not provide care if immune caregivers are available.
Note: (Recent assessment of outbreaks in healthy 18- to 24-year-olds has indicated that salivary viral shedding occurred early in the course of illness and that 5 days of isolation after onset of parotitis may be appropriate in community settings; however the implications for healthcare personnel and high-risk patient populations remain to be clarified.) |
| Parvovirus B19 (Erythema infectiosum) | D | Maintain precautions for duration of hospitalization when chronic
disease occurs in an immunocompromised patient. For patients with transient aplastic crisis or red-cell crisis, maintain precautions for 7 days. Duration of precautions for immunosuppressed patients with persistently positive PCR not defined, but transmission has occurred.[55] | |
| Pertussis (whooping cough) | D | U 5 days | Single patient room preferred. Cohorting an option. Post-exposure chemoprophylaxis for household contacts and HCWs with prolonged exposure to respiratory secretions.[56] Recommendations for Tdap vaccine in adults under development. |
| Plague (Yersinia pestis) Bubonic | S | ||
| Plague (Yersinia pestis) Pneumonic | D | U 48 hrs | Antimicrobial prophylaxis for exposed HCW.[57] |
| Pneumonia Adenovirus | D,C | DI | Outbreaks in pediatric and institutional settings reported.[58][59][60][61] In immunocompromised hosts, extend duration of droplet and contact precautions due to prolonged shedding of virus[62] |
| Rubella (German measles) ( also see congenital rubella) | D | U 7 days after onset of rash | Susceptible HCWs should not enter room if immune caregivers are available. No recommendation for wearing face protection (e.g., a surgical mask) if immune. Pregnant women who are not immune should not care for these patients.[50][63] Administer vaccine within three days of exposure to non-pregnant susceptible individuals. Place exposed susceptible patients on Droplet Precautions; exclude susceptible healthcare personnel from duty from day 5 after first exposure to day 21 after last exposure, regardless of post-exposure vaccine |
| Severe acute respiratory syndrome (SARS) | A,D,C | DI plus 10 days after resolution offever, provided respiratory symptoms are absent or improving | Airborne Precautions preferred; D if AIIR unavailable. N95 or higher respiratory protection; surgical mask if N95 unavailable; eye protection (goggles, face shield); aerosol-generating procedures and "supershedders" highest risk for transmission via small droplet nuclei and large droplets.[64][65][66] Vigilant environmental disinfection (see www.cdc.gov/ncidod/sars) |
| Smallpox | A,C | DI | Until all scabs have crusted and separated (3–4 weeks). Non-vaccinated HCWs should not provide care when immune HCWs are available; N95 or higher respiratory protection for susceptible and successfully vaccinated individuals; post-exposure vaccine within 4 days of exposure protective.[67][68][69][70][71] |
| Streptococcal disease (group A streptococcus) Skin, wound, or burn major | C,D | U 24 hrs | No dressing or dressing does not contain drainage adequately |
| Tuberculosis (M. tuberculosis) Extrapulmonary, draining lesion) | A,C | Discontinue precautions only when patient is improving clinically, and drainage has ceased or there are three consecutive negative cultures of continued drainage.[72][73] Examine for evidence of active pulmonary tuberculosis. | |
| Tuberculosis (M. tuberculosis) Pulmonary or laryngeal disease, confirmed | A | Discontinue precautions only when patient on effective therapy is improving clinically and has three consecutive sputum smears negative for acid-fast bacilli collected on separate days(MMWR 2005; 54: RR-17 https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm?s_cid=rr5417a1_e ) 12. | |
| Varicella Zoster | A,C | Until lesions dry and crusted | Susceptible HCWs should not enter room if immune caregivers are available; no recommendation for face protection of immune HCWs; no recommendation for type of protection, i.e. surgical mask or respirator for susceptible HCWs. In immunocompromised host with varicella pneumonia, prolong duration of precautions for duration of illness. Post-exposure prophylaxis: provide post-exposure vaccine ASAP but within 120 hours; for susceptible exposed persons for whom vaccine is contraindicated (immunocompromised persons, pregnant women, newborns whose mother's varicella onset is <5 days before delivery or within 48 hrs after delivery) provide VZIG, when available, within 96 hours; if unavailable, use IVIG, Use Airborne Precautions for exposed susceptible persons and exclude exposed susceptible healthcare workers beginning 8 days after first exposure until 21 days after last exposure or 28 if received VZIG, regardless of postexposure vaccination.[74] |
| Viral hemorrhagic fevers due to Lassa, Ebola, Marburg, Crimean-Congo fever viruses | S,D,C | DI | Single-patient room preferred. Emphasize: 1) use of sharps safety devices and safe work practices, 2) hand hygiene; 3) barrier protection against blood and body fluids upon entry into room (single gloves and fluid-resistant or impermeable gown, face/eye protection with masks, goggles or face shields); and 4) appropriate waste handling. Use N95 or higher respirators when performing aerosol-generating procedures. Largest viral load in final stages of illness when hemorrhage may occur; additional PPE, including double gloves, leg and shoe coverings may be used, especially in resource-limited settings where options for cleaning and laundry are limited. Notify public health officials immediately if Ebola is suspected[21][75][76][77] |
1 Type of precautions: A, airborne; C, contact; D, droplet; S, standard; when A, C, and D are specified, also use S.
² Duration of precautions: CN, until off antimicrobial treatment and culture-negative; DI, duration of illness (with wound lesions, DI means until wounds stop draining); DE, until environment completely decontaminated; U, until time specified in hours (hrs) after initiation of effective therapy; Unknown: criteria for establishing eradication of pathogen has not been determined
Discontinuation
Transmission-based precautions remain in effect for limited periods of time (i.e., while the risk for transmission of the infectious agent persists or for the duration of the illness (Appendix A).[1] For most infectious diseases, this duration reflects known patterns of persistence and shedding of infectious agents associated with the natural history of the infectious process and its treatment. For some diseases (e.g., pharyngeal or cutaneous diphtheria, RSV), transmission-based precautions remain in effect until culture or antigen-detection test results document eradication of the pathogen and, for RSV, symptomatic disease is resolved. For other diseases, (e.g., M. tuberculosis) state laws and regulations, and healthcare facility policies, may dictate the duration of precautions 12). In immunocompromised patients, viral shedding can persist for prolonged periods of time (many weeks to months) and transmission to others may occur during that time; therefore, the duration of contact and/or droplet precautions may be prolonged for many weeks.[41][42][47][62][78][79][80] The duration of contact precautions for patients who are colonized or infected with MDROs remains undefined. MRSA is the only MDRO for which effective decolonization regimens are available.[81] However, carriers of MRSA who have negative nasal cultures after a course of systemic or topical therapy may resume shedding MRSA in the weeks that follow therapy.[82][83] Although early guidelines for VRE suggested discontinuation of contact precautions after three stool cultures obtained at weekly intervals proved negative,[21] subsequent experiences have indicated that such screening may fail to detect colonization that can persist for >1 year.[84][85][86][87] Likewise, available data indicate that colonization with VRE, MRSA,[88] and possibly MDR-GNB, can persist for many months, especially in the presence of severe underlying disease, invasive devices, and recurrent courses of antimicrobial agents. It may be prudent to assume that MDRO carriers are colonized permanently and manage them accordingly. Alternatively, an interval free of hospitalizations, antimicrobial therapy, and invasive devices (e.g., 6 or 12 months) before reculturing patients to document clearance of carriage may be used. Determination of the best strategy awaits the results of additional studies. See the 2006 HICPAC/CDC MDRO guideline[14] for discussion of possible criteria to discontinue contact precautions for patients colonized or infected with MDROs.
Application in ambulatory and home care settings
Although transmission-based precautions generally apply in all healthcare settings, exceptions exist. For example, in home care, AIIRs are not available. Furthermore, family members already exposed to diseases such as varicella and tuberculosis would not use masks or respiratory protection, but visiting HCWs would need to use such protection. Similarly, management of patients colonized or infected with MDROs may necessitate contact precautions in acute care hospitals and in some LTCFs when there is continued transmission, but the risk of transmission in ambulatory care and home care, has not been defined. Consistent use of standard precautions may suffice in these settings, but more information is needed.
Patients requiring outpatient services with known airborne or droplet transmitted diseases should be scheduled at the end of the day to minimize exposure to other patients. These patients should also be educated on proper respiratory etiquette - coughing into their elbow and wearing a mask. Healthcare professionals should also wear proper PPE when anticipating contact with these patients.
Patients with known contact transmitted diseases coming into ambulatory clinics should be triaged quickly and placed in a private room. Items used in these rooms should not be taken out of the room unless properly sanitized. Healthcare workers must practice proper hand hygiene when exiting the private room.
Patients placed in long-term care facilities should be placed in single rooms, have access to their own items or use disposable items, and should have limited contact with other residents, in order to reduce the spread of contact transmitted diseases. For patients with airborne and droplet transmitted diseases in long-term care facilities, they should wear masks when around other residents, and proper PPE and standard precautions should be maintained throughout facilities. In addition, residents of long-term care facilities who are identified as at-risk for these diseases should be immunized if possible.
Side effects
When transmission-based precautions are indicated, efforts must be made to counteract possible adverse effects on patients (i.e., anxiety, depression and other mood disturbances,[89][90][91] perceptions of stigma,[92] reduced contact with clinical staff,[93][94][95] and increases in preventable adverse events[96] in order to improve acceptance by the patients and adherence by health care workers).
Footnotes
- Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee, 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings
- Infection prevention and control of epidemic- and pandemic-prone acute respiratory diseases in health care, WHO Interim Guidelines.2007 p. 53
- "Hospital eTool: Healthcare Wide Hazards - (Lack of) Universal Precautions". www.osha.gov. Retrieved 2020-04-14.
- "Standard Precautions for All Patient Care". www.cdc.gov. 2019-03-25. Retrieved 2020-04-14.
- National Communicable Disease Center. Isolation Techniques for Use in Hospitals. 1st ed. Washington, DC: US Government Printing Office;. PHS publication no 2054 1970
- Garner JS, Simmons BP. CDC Guideline for Isolation Precautions in Hospitals. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control; 1983. HHS publication no. (CDC) 83-8314. Infect Control 1983;4:245-325.
- CDC. Update: universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep 1988;37(24):377-82, 87-8.
- CDC. Recommendations for preventing transmission of infection with human T- lymphotropic virus type III/lymphadenopathy-associated virus in the workplace. MMWR Morb Mortal Wkly Rep 1985;34(450:681-6, 91-5.
- Lynch P, Jackson MM, Cummings MJ, Stamm WE. Rethinking the role of isolation practices in the prevention of nosocomial infections. Ann Intern Med 1987;107(2):243-6.
- Garner JS. Guideline for isolation precautions in hospitals. The Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1996;17(1):53-80.(s).
- Bonita, Ruth et al.. Basic epidemiology. 2nd edition. World Health Organization. 226 p., 2006
- "Healthcare Providers". www.cdc.gov. 2020-02-11. Retrieved 2020-04-14.
- Verbeek, Jos H.; Rajamaki, Blair; Ijaz, Sharea; Sauni, Riitta; Toomey, Elaine; Blackwood, Bronagh; Tikka, Christina; Ruotsalainen, Jani H.; Kilinc Balci, F. Selcen (15 May 2020). "Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff". The Cochrane Database of Systematic Reviews. 2020 (5): CD011621. doi:10.1002/14651858.CD011621.pub5. hdl:1983/b7069408-3bf6-457a-9c6f-ecc38c00ee48. ISSN 1469-493X. PMC 8785899. PMID 32412096.
- Management of Multidrug-Resistant Organisms In Healthcare Settings, 2006. 2006. www.cdc.gov/ncidod/dhqp/pdf/ar/mdroGuideline2006.pdf
- Donskey CJ. The role of the intestinal tract as a reservoir and source for transmission of nosocomial pathogens. Clin Infect Dis 2004;39(2):219-26.
- Bhalla A, Pultz NJ, Gries DM, et al. Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect Control Hosp Epidemiol 2004;25(2):164-7.
- Duckro AN, Blom DW, Lyle EA, Weinstein RA, Hayden MK. Transfer of vancomycin-resistant enterococci via health care worker hands. Arch Intern Med 2005;165(3):302-7.
- Hall CB, Douglas RG, Jr. Modes of transmission of respiratory syncytial virus. J Pediatr 1981;99(1):100-3.
- Evans MR, Meldrum R, Lane W, et al. An outbreak of viral gastroenteritis following environmental contamination at a concert hall. Epidemiol Infect 2002;129(2):355-60.
- Wu HM, Fornek M, Kellogg JS, et al. A Norovirus Outbreak at a Long-Term-Care Facility: The Role of Environmental Surface Contamination. Infect Control Hosp Epidemiol 2005;26(10):802-10.
- CDC. Recommendations for preventing the spread of vancomycin resistance. Recommendations of the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm Rep 1995;44 (RR12):1-13.
- Wells WF. On air-borne infection: study II. Droplets and droplet nuclei. American Journal of Hygiene 1934;20:611-8.
- CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep 2005;54(17):1-141.
- AIA. Guidelines for Design and Construction of Hospital and Health Care Facilities. In: American Institute of Architects. Washington, DC: American Institute of Architects Press; 2006.
- "Stevens, Richard William, (1 Oct. 1924–21 March 1997), Partner, Richard Stevens Design Associates, 1987–94", Who Was Who, Oxford University Press, 2007-12-01, doi:10.1093/ww/9780199540884.013.u182117
- "Health hazard evaluation report: HETA-83-341-1557, Bureau of Reclamation, U.S. Department of the Interior, Denver, Colorado". 1985-01-01. doi:10.26616/nioshheta833411557.
{{cite journal}}: Cite journal requires|journal=(help) - Brooks S, Khan A, Stoica D, et al. Reduction in vancomycin-resistant Enterococcus and Clostridium difficile infections following change to tympanic thermometers. Infect Control Hosp Epidemiol 1998;19(5):333-6.
- Jernigan JA, Siegman-Igra Y, Guerrant RC, Farr BM. A randomized crossover study of disposable thermometers for prevention of Clostridium difficile and other nosocomial infections. Infect Control Hosp Epidemiol 1998;19(7):494-9.
- Wilcox MH, Fawley WN, Wigglesworth N, Parnell P, Verity P, Freeman J. Comparison of the effect of detergent versus hypochlorite cleaning on environmental contamination and incidence of Clostridium difficile infection. J Hosp Infect 2003;54(2):109-14.
- Weber DJ, Sickbert-Bennett E, Gergen MF, Rutala WA. Efficacy of selected hand hygiene agents used to remove Bacillus atrophaeus (a surrogate of Bacillus anthracis) from contaminated hands. Jama 2003;289(10):1274-7.
- Avitzur Y, Amir J. Herpetic whitlow infection in a general pediatrician-an occupational hazard. Infection 2002;30(4):234-6.
- Maitreyi RS, Dar L, Muthukumar A, et al. Acute hemorrhagic conjunctivitis due to enterovirus 70 in India. Emerg Infect Dis 1999;5(2):267-9.
- Hall CB. Nosocomial respiratory syncytial virus infections: the "Cold War" has not ended. Clin Infect Dis 2000;31(2):590-6.
- CDC. Acute hemorrhagic conjunctivitis outbreak caused by Coxsackievirus A24--Puerto Rico, 2003. MMWR Morb Mortal Wkly Rep 2004;53(28):632-4.
- Montessori V, Scharf S, Holland S, Werker DH, Roberts FJ, Bryce E. Epidemic keratoconjunctivitis outbreak at a tertiary referral eye care clinic. Am J Infect Control 1998;26(4):399-405
- Buffington J, Chapman LE, Stobierski MG, et al. Epidemic keratoconjunctivitis in a chronic care facility: risk factors and measures for control. J Am Geriatr Soc 1993;41(11):1177-81.
- Jernigan JA, Lowry BS, Hayden FG, et al. Adenovirus type 8 epidemic keratoconjunctivitis in an eye clinic: risk factors and control. J Infect Dis 1993;167(6):1307-13.
- Warren D, Nelson KE, Farrar JA, et al. A large outbreak of epidemic keratoconjunctivitis: problems in controlling nosocomial spread. J Infect Dis 1989;160(6):938-43.
- Chaberny IE, Schnitzler P, Geiss HK, Wendt C. An outbreak of epidemic keratoconjunctivtis in a pediatric unit due to adenovirus type 8. Infect Control Hosp Epidemiol 2003;24(7):514-9.
- Faden H, Wynn RJ, Campagna L, Ryan RM. Outbreak of adenovirus type 30 in a neonatal intensive care unit. J Pediatr 2005;146(4):523-7.
- Wood DJ, David TJ, Chrystie IL, Totterdell B. Chronic enteric virus infection in two T-cell immunodeficient children. J Med Virol 1988;24(4):435-44.
- Mori I, Matsumoto K, Sugimoto K, et al. Prolonged shedding of rotavirus in a geriatric inpatient. J Med Virol 2002;67(4):613-5.
- COID. 2003 Report of the Committee on Infectious Diseases. In: Redbook. Elk Grove Village, IL: American Academy of Pediatrics; 2003.
- Rosenblum LS, Villarino ME, Nainan OV, et al. Hepatitis A outbreak in a neonatal intensive care unit: risk factors for transmission and evidence of prolonged viral excretion among preterm infants. J Infect Dis 1991;164(3):476-82.
- Carl M, Kantor RJ, Webster HM, Fields HA, Maynard JE. Excretion of hepatitis A virus in the stools of hospitalized hepatitis patients. J Med Virol 1982;9(2):125-9.
- CDC. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005;54(RR-8):1-40.
- Weinstock DM, Gubareva LV, Zuccotti G. Prolonged shedding of multidrug-resistant influenza A virus in an immunocompromised patient. N Engl J Med 2003;348(9):867-8.
- Ammari LK, Bell LM, Hodinka RL. Secondary measles vaccine failure in healthcare workers exposed to infected patients. Infect Control Hosp Epidemiol 1993;14(2):81-6.
- Behrman A, Schmid DS, Crivaro A, Watson B. A cluster of primary varicella cases among healthcare workers with false-positive varicella zoster virus titers. Infect Control Hosp Epidemiol 2003;24(3):202-6.
- Bolyard EA, Tablan OC, Williams WW, Pearson ML, Shapiro CN, Deitchmann SD. Guideline for infection control in healthcare personnel, 1998. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1998;19(6):407-63.
- Ruuskanen O, Salmi TT, Halonen P. Measles vaccination after exposure to natural measles. J Pediatr 1978;93(1):43-6.
- CDC. Measles, mumps, and rubella--vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1998;47(RR-8):157.
- Fleischauer AT, Kile JC, Davidson M, et al. Evaluation of human-tohuman transmission of monkeypox from infected patients to health care workers. Clin Infect Dis 2005;40(5):689-94.
- Management of Multidrug-Resistant Organisms In Healthcare Settings, 2006. CDC, 2006.
- Lui SL, Luk WK, Cheung CY, Chan TM, Lai KN, Peiris JS. Nosocomial outbreak of parvovirus B19 infection in a renal transplant unit. Transplantation 2001;71(1):59-64.
- CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep 2005;54(RR-14):1-16.
- Kool JL. Risk of person-to-person transmission of pneumonic plague. Clin Infect Dis 2005;40(8):1166-72.
- Hatherill M, Levin M, Lawrenson J, Hsiao NY, Reynolds L, Argent A. Evolution of an adenovirus outbreak in a multidisciplinary children's hospital. J Paediatr Child Health 2004;40(8):449-54.
- Sanchez MP, Erdman DD, Torok TJ, Freeman CJ, Matyas BT. Outbreak of adenovirus 35 pneumonia among adult residents and staff of a chronic care psychiatric facility. J Infect Dis 1997;176(3):760-3.(s).
- Singh-Naz N, Brown M, Ganeshananthan M. Nosocomial adenovirus infection: molecular epidemiology of an outbreak. Pediatr Infect Dis J 1993;12(11):922-5.
- Uemura T, Kawashitam T, Ostuka Y, Tanaka Y, Kusubae R, Yoshinaga M. A recent outbreak of adenovirus type 7 infection in a chronic inpatient facility for the severely handicapped. Infect Control Hosp Epidemiol 2000;21(9):559-60.
- van Tol MJ, Claas EC, Heemskerk B, et al. Adenovirus infection in children after allogeneic stem cell transplantation: diagnosis, treatment and immunity. Bone Marrow Transplant 2005;35 Suppl 1:S73-6.
- Fliegel PE, Weinstein WM. Rubella outbreak in a prenatal clinic: management and prevention. Am J Infect Control 1982;10(1):29-33.
- Loeb M, McGeer A, Henry B, et al. SARS among critical care nurses, Toronto. Emerg Infect Dis 2004;10(2):251-5.
- Fowler RA, Guest CB, Lapinsky SE, et al. Transmission of severe acute respiratory syndrome during intubation and mechanical ventilation. Am J Respir Crit Care Med 2004;169(11):1198-202.
- Scales D, et al. Illness in intensive-care staff after brief exposure to severe acute respiratory syndrome. Emerg Infect Dis 2003;9(10):1205-10.
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. The epidemiology of smallpox. In: Smallpox and its eradication. Switzerland: World Health Organization; 1988.
- Gelfand HM, Posch J. The recent outbreak of smallpox in Meschede, West Germany. Am J Epidemiol 1971;93(4):234-7.
- CDC. Vaccinia (smallpox) vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2001. MMWR Recomm Rep 2001;50(RR-10):1-25; quiz CE1-7.
- Fulginiti VA, Papier A, Lane JM, Neff JM, Henderson DA. Smallpox vaccination: a review, part I. Background, vaccination technique, normal vaccination and revaccination, and expected normal reactions. Clin Infect Dis 2003;37(2):241-50.
- Dixon CW. Smallpox in Tripolitania, 1946: an epidemiological and clinical study of 500 cases, including trials of penicillin treatment. . J Hyg (Lond) 1948;46:351-77.
- Hutton MD, Stead WW, Cauthen GM, Bloch AB, Ewing WM. Nosocomial transmission of tuberculosis associated with a draining abscess. J Infect Dis 1990;161(2):286-95.
- Frampton MW. An outbreak of tuberculosis among hospital personnel caring for a patient with a skin ulcer. Ann Intern Med 1992;117(4):312-3.
- Watson B, Seward J, Yang A, et al. Postexposure effectiveness of varicella vaccine. Pediatrics 2000;105(1 Pt 1):84-8.
- Borio L, Inglesby T, Peters CJ, et al. Hemorrhagic fever viruses as biological weapons: medical and public health management. JAMA 2002;287(18):2391-405.
- www.bt.cdc.gov/agent/vhf/
- CDC. Emergency Preparedness & Response. wwwbtcdcgov 2003.
- Zambon M, Bull T, Sadler CJ, Goldman JM, Ward KN. Molecular epidemiology of two consecutive outbreaks of parainfluenza 3 in a bone marrow transplant unit. J Clin Microbiol 1998;36(8):2289-93.
- Hall CB, Powell KR, MacDonald NE, et al. Respiratory syncytial viral infection in children with compromised immune function. N Engl J Med 1986;315(2):77-81.
- Lui SL, Luk WK, Cheung CY, Chan TM, Lai KN, Peiris JS. Nosocomial outbreak of parvovirus B19 infection in a renal transplant unit. Transplantation 2001;71(1):59-64
- Boyce JM. MRSA patients: proven methods to treat colonization and infection. J Hosp Infect 2001;48 Suppl A:S9-14.
- Cederna JE, Terpenning MS, Ensberg M, Bradley SF, Kauffman CA. Staphylococcus aureus nasal colonization in a nursing home: eradication with mupirocin. Infect Control Hosp Epidemiol 1990;11(1):13-6.
- Kauffman CA, Terpenning MS, He X, et al. Attempts to eradicate methicillin-resistant Staphylococcus aureus from a long-term-care facility with the use of mupirocin ointment. Am J Med 1993;94(4):371-8.
- Bonten MJ, Slaughter S, Ambergen AW, et al. The role of "colonization pressure" in the spread of vancomycin-resistant enterococci: an important infection control variable. Arch Intern Med 1998;158(10):1127-32.
- Montecalvo MA, de Lencastre H, Carraher M, et al. Natural history of colonization with vancomycin-resistant Enterococcus faecium. Infect Control Hosp Epidemiol 1995;16(12):680-5.
- D'Agata EM, et al. High rate of false-negative results of the rectal swab culture method in detection of gastrointestinal colonization with vancomycin-resistant enterococci. Clin Infect Dis 2002;34(2):167-72.
- Donskey CJ, Hoyen CK, Das SM, Helfand MS, Hecker MT. Recurrence of vancomycin-resistant Enterococcus stool colonization during antibiotic therapy. Infect Control Hosp Epidemiol 2002;23(8):436-40.
- Scanvic A, Denic L, Gaillon S, Giry P, Andremont A, Lucet JC. Duration of colonization by methicillin-resistant Staphylococcus aureus after hospital discharge and risk factors for prolonged carriage. Clin Infect Dis 2001;32(10):1393-8.
- Catalano G, Houston SH, Catalano MC, et al. Anxiety and depression in hospitalized patients in resistant organism isolation. South Med J 2003;96(2):141-5.
- Tarzi S, Kennedy P, Stone S, Evans M. Methicillin-resistant Staphylococcus aureus: psychological impact of hospitalization and isolation in an older adult population. J Hosp Infect 2001;49(4):250-4.
- Kelly-Rossini L, Perlman DC, Mason DJ. The experience of respiratory isolation for HIV-infected persons with tuberculosis. J Assoc Nurses AIDS Care 1996;Jan-Feb; 7(1):29-36.
- Knowles HE. The experience of infectious patients in isolation. Nurs Times 1993;89(30):53-6.
- Evans HL, Shaffer MM, Hughes MG, et al. Contact isolation in surgical patients: a barrier to care? Surgery 2003;134(2):180-8.
- Kirkland KB, Weinstein JM. Adverse effects of contact isolation. Lancet 1999;354(9185):1177-8.
- Saint S, Higgins LA, Nallamothu BK, Chenoweth C. Do physicians examine patients in contact isolation less frequently? A brief report. Am J Infect Control 2003;31(6):354-6.
- Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA 2003;290(14):1899-905.