Two-point discrimination
Two-point discrimination (2PD) is the ability to discern that two nearby objects touching the skin are truly two distinct points, not one. It is often tested with two sharp points during a neurological examination[1]: 632 [2]: 71 and is assumed to reflect how finely innervated an area of skin is.
| Two-point discrimination | |
|---|---|
 Different areas of the body have receptive fields of different sizes, giving some better resolution in two-point discrimination. Areas including the fingertips, lips, and tongue have very high resolution, and therefore are the most sensitive. Other areas like the forearms, calves, and back are the least sensitive. This is illustrated as the distance where the two points can be felt as separate. |
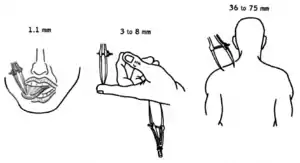
In clinical settings, two-point discrimination is a widely used technique for assessing tactile perception.[3] It relies on the ability and/or willingness of the patient to subjectively report what they are feeling and should be completed with the patient’s eyes closed.[4] The therapist may use calipers or simply a reshaped paperclip to do the testing.[5] The therapist may alternate randomly between touching the patient with one point or with two points on the area being tested (e.g. finger, arm, leg, toe).[4] The patient is asked to report whether one or two points was felt. The smallest distance between two points that still results in the perception of two distinct stimuli is recorded as the patient's two-point threshold.[6] Performance on the two extremities can be compared for discrepancies. Although the test is still commonly used clinically, it has been roundly criticized by many researchers as providing an invalid measure of tactile spatial acuity, and several highly regarded alternative tests have been proposed to replace it.
Normal and impaired performance
Body areas differ both in tactile receptor density and somatosensory cortical representation. Normally, a person should be able to recognize two points separated by 2 to 8 mm on fingertips. On the lips, it is 2 to 4 mm, and on the palms, it is 8 to 12 mm and 30–40 mm on the shins or back (assuming the points are at the same dermatome).[1]: 632 The posterior column-medial lemniscus pathway is responsible for carrying information involving fine, discriminative touch. Therefore, two-point discrimination can be impaired by damage to this pathway or to a peripheral nerve.[6]
Criticisms
Although two-point testing is commonly used clinically, evidence accumulated from many research studies indicates that 2PD is a flawed measure of tactile spatial acuity. Research studies have shown that the two-point test may have low sensitivity, failing to detect or underestimating sensory deficits,[7][8] that it only poorly tracks recovery of function following nerve injury and repair,[9][8][10] that it has poor test-retest reliability,[11] and that it fails to correlate with validated measures of tactile spatial acuity such as grating orientation discrimination.[8][12] Two-point testing has been criticized for yielding highly variable performance both across and within participants, for being reliant on the subjective criterion adopted by the participant for reporting "one" compared to "two," and for resulting in performance that is "too good to be true," as the measured two-point threshold can fall — unrealistically — well below the skin's receptor spacing.[13][14][15][16][17]
It has long been recognized that, if not pressed precisely simultaneously, two points may evoke temporally distinguishable neural activations; two points may be distinguished from one, then, not because two points are perceived spatially, but because two contacts are perceived temporally.[18][15] Furthermore, neurophysiological recordings have shown that two points evoke a different number of action potentials in the receptor population than one point does; two points may be distinguished from one, then, not because two points are actually perceived, but merely because the two-point configuration produces a different overall response magnitude.[19][20] In summary, the two-point task can present both a non-spatial temporal cue and a non-spatial magnitude cue. To an observant participant, these unintended non-spatial cues could signal the presence of two points compared to one, even when the points are placed closer together than the participant's spatial resolution.[16]
On the basis of these observations, several researchers have strongly warned against the use of the 2PD task. Pointing to “the enormous and implausible variability in reported 2PD levels after nerve repair,” the authors of one article “conclude that ... 2PD ... as the sole test for tactile gnosis recovery should be seriously questioned.”[15] Comparing 2PD thresholds to functional recovery in patients following nerve repair, another author states "The conclusion to be drawn from this data is that 2 P.D. is not a valid index of the sensory capacity underlying integrated hand function."[9] The author of a book on nerve repair concludes that 2PD is a “convenient but critically flawed procedure” that “presents nonspatial cues that can be learned to improve performance without physiologic change”.[10] The authors of an article tersely entitled "The two-point threshold: Not a measure of tactile spatial resolution"[20] recommend alternative tests to supplant the 2PD test. The authors of yet another research article concur and strongly recommend “that clinicians and researchers simply set aside the 2PD task and replace it with one that ensures a more purely spatial measure of acuity".[16]
Alternative tests
Several highly regarded tactile tests have been developed as rigorous replacements to the 2PD test.[13][16] In psychophysics research laboratories, a favored test of tactile spatial acuity has for many years been the grating orientation task (GOT).[13] In the GOT, the participant attempts to discern the orientation of parallel grooves pressed either along or across the fingertip. The GOT threshold is the groove width at which the participant performs with some specified level of accuracy (e.g., 75% correct). The GOT is considered to yield a valid measure of tactile spatial acuity and has been used in many research studies, with both manual and automated stimulus delivery protocols.[13][21][22] For example, the GOT has been used to map spatial acuity on different body areas,[23][24] to characterize how tactile spatial acuity is affected by age,[25][26][27] sex,[28] skin characteristics,[29][28] and blindness,[30][31] and to track the changes in tactile spatial acuity that occur during perceptual learning[32][33] and recovery from nerve injury.[8]
Although it is very popular in tactile research labs, the GOT is admittedly less practical for clinical use, as it requires specialized pre-constructed stimulus objects, which span a fixed spatial range, rather than a single continuously adjustable calipers.[14][16] The comparative simplicity and flexibility of the 2PD test have encouraged the continuation of its use by clinicians, despite the test's acknowledged flaws.[15] To remedy this situation, two-point orientation discrimination (2POD) has been proposed as a test that combines the convenience of 2PD with the validity of the GOT.[16] In the 2POD task, the patient attempts to discern the orientation (e.g., along or across the finger) created by two sharp points of contact on the skin; the 2POD threshold is the distance between the points at which the participant performs with some specified level of accuracy (e.g., 75% correct).[16]
As explained above, the validity of the 2PD task has been called into question because it allows the participant to rely on non-spatial cues. By contrast, the GOT and 2POD tasks are considered to yield valid measures of tactile spatial acuity, because in order to perform these tasks, the participant must discern the spatial modulation of the neural discharge of underlying skin receptors and cannot rely on non-spatial cues.[13][21][16] The following figure, from a study that evaluated both 2PD and 2POD on the fingertip, finger base, palm and forearm,[16] demonstrates that 2PD is contaminated by non-spatial cues, whereas 2POD provides an uncontaminated measure of tactile spatial acuity.
| Traditional two-point discrimination (2PD) compared to 2-point orientation discrimination (2POD) |
|---|
_compared_to_traditional_two-point_discrimination_(2PD).jpg.webp) Traditional two-point discrimination compared to two-point orientation discrimination. |
| Tong et al. (2013)[16] tested 24 neurologically healthy participants on four skin sites, using both two-point discrimination (2PD) and two-point orientation discrimination (2POD). All participants were tested on both tasks, using the same fine-tipped calipers and an objective two-interval forced-choice protocol. The order of testing was counterbalanced across participants. Mean proportion correct versus calliper tip separation is shown for (A) 2PD and (B) 2POD. Note that 2PD performance (A) is significantly above chance even at zero mm separation, as found also in previous research;[13] this indicates that 2PD is not a valid measure of tactile spatial acuity. In contrast, 2POD performance (B) falls to chance level (50% correct) as separation approaches zero mm, as required for a valid measure of spatial acuity. On the basis of these results, the authors recommend that clinicians discard the 2PD task and replace it with 2POD. |
References
- Bickley, Lynn; Szilagui, Peter (2007). Bates' Guide to Physical Examination and History Taking (9th ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-6718-7. ASIN B0028IKRYG.
- Blumenfeld, Hal (2002). Neuroanatomy Through Clinical Cases. Sunderland, MA: Sinauer. ISBN 978-0-87893-060-9.
- Shooter, David (2005). "Use of two-point discrimination as a nerve repair assessment tool: Preliminary report". ANZ Journal of Surgery. 75 (10): 866–868. doi:10.1111/j.1445-2197.2005.03557.x. PMID 16176227. S2CID 25300643.
- Blumenfeld, Hal (2010). Neuroanatomy through Clinical Cases. Sunderland, MA: Sinauer Associates, Inc. pp. 71–72. ISBN 978-0-87893-058-6.
- Finnell, John T.; Knopp, Robert; Johnson, Phelps; Holland, Patrick C.; Schubert, Warren (June 2004). "A calibrated paper clip is a reliable measure of two-point discrimination". Academic Emergency Medicine. 11 (6): 710–714. doi:10.1197/j.aem.2003.11.022. ISSN 1069-6563. PMID 15175216.
- O'Sullivan, Susan (2007). Physical Rehabilitation Fifth Edition. Philadelphia: F.A. Davis Company. pp. 136–146. ISBN 978-0-8036-1247-1.
- van Nes SI, Faber CG, Hamers RM, Harschnitz O, Bakkers M, Hermans MC, Meijer RJ, van Doorn PA, Merkies IS, PeriNomS Study, Group (July 2008). "Revising two-point discrimination assessment in normal aging and in patients with polyneuropathies". Journal of Neurology, Neurosurgery, and Psychiatry. 79 (7): 832–4. doi:10.1136/jnnp.2007.139220. PMID 18450792. S2CID 40792906.
- Van Boven, RW; Johnson, KO (February 1994). "A psychophysical study of the mechanisms of sensory recovery following nerve injury in humans". Brain: A Journal of Neurology. 117 (1): 149–67. doi:10.1093/brain/117.1.149. PMID 8149208.
- Marsh, D. (February 1990). "The validation of measures of outcome following suture of divided peripheral nerves supplying the hand". Journal of Hand Surgery (Edinburgh, Scotland). 15 (1): 25–34. doi:10.1016/0266-7681(90)90043-4. ISSN 0266-7681. PMID 2307877.
- Brushart, Thomas M. (2011). Nerve Repair. Chapter 4: Determining Clinical Outcomes. Oxford University Press. ISBN 9780199721603.
- Ehrenbrusthoff, K.; Ryan, C. G.; Grüneberg, C.; Wolf, U.; Krenz, D.; Atkinson, G.; Martin, D. J. (2016). "The intra- and inter-observer reliability of a novel protocol for two-point discrimination in individuals with chronic low back pain". Physiological Measurement. 37 (7): 1074–1088. Bibcode:2016PhyM...37.1074E. doi:10.1088/0967-3334/37/7/1074. ISSN 1361-6579. PMID 27321473.
- Bruns, Patrick; Camargo, Carlos J.; Campanella, Humberto; Esteve, Jaume; Dinse, Hubert R.; Röder, Brigitte (2014-02-04). "Tactile Acuity Charts: A Reliable Measure of Spatial Acuity". PLOS ONE. 9 (2): e87384. Bibcode:2014PLoSO...987384B. doi:10.1371/journal.pone.0087384. ISSN 1932-6203. PMC 3913609. PMID 24504346.
- Johnson, KO; Phillips, JR (December 1981). "Tactile spatial resolution. I. Two-point discrimination, gap detection, grating resolution, and letter recognition". Journal of Neurophysiology. 46 (6): 1177–92. doi:10.1152/jn.1981.46.6.1177. PMID 7320742.
- Stevens, JC; Patterson, MQ (1995). "Dimensions of spatial acuity in the touch sense: changes over the life span". Somatosensory & Motor Research. 12 (1): 29–47. doi:10.3109/08990229509063140. PMID 7571941.
- Lundborg, G; Rosén, B (October 2004). "The two-point discrimination test--time for a re-appraisal?". Journal of Hand Surgery (Edinburgh, Scotland). 29 (5): 418–22. doi:10.1016/j.jhsb.2004.02.008. PMID 15336741. S2CID 34717685.
- Tong, J; Mao, O; Goldreich, D (2013). "Two-point orientation discrimination versus the traditional two-point test for tactile spatial acuity assessment". Frontiers in Human Neuroscience. 7 (579): 579. doi:10.3389/fnhum.2013.00579. PMC 3772339. PMID 24062677.
- Johnson, K.O.; Van Boven, R.W.; Hsiao, S.S. (1994). "The perception of two points is not the spatial resolution threshold," in Touch, Temperature, and Pain in Health and Disease: Mechanisms and Assessments: a Wenner-Gren Center International Symposium, 1st Edn, eds J. Boivie, P. Hansson, and U. Lindblom. Seattle: IASP Press. pp. 389–404.
- Woolley, Helen Bradford Thompson (1903). The Mental Traits of Sex: An Experimental Investigation of the Normal Mind in Men and Women. University of Chicago Press. Chapter 3: Skin and Muscle Senses.
- Vega-Bermudez, F; Johnson, KO (June 1999). "Surround suppression in the responses of primate SA1 and RA mechanoreceptive afferents mapped with a probe array". Journal of Neurophysiology. 81 (6): 2711–9. CiteSeerX 10.1.1.487.7255. doi:10.1152/jn.1999.81.6.2711. PMID 10368391.
- Craig, J. C.; Johnson (2000). "The two-point threshold: Not a measure of tactile spatial resolution". Current Directions in Psychological Science. 9: 29–32. doi:10.1111/1467-8721.00054. S2CID 142991309.
- Craig, J. C. (1999). "Grating orientation as a measure of tactile spatial acuity". Somatosensory & Motor Research. 16 (3): 197–206. doi:10.1080/08990229970456. ISSN 0899-0220. PMID 10527368.
- Goldreich, Daniel; Wong, Michael; Peters, Ryan M.; Kanics, Ingrid M. (2009-06-03). "A Tactile Automated Passive-Finger Stimulator (TAPS)". Journal of Visualized Experiments (28): e1374. doi:10.3791/1374. ISSN 1940-087X. PMC 2726582. PMID 19578327.
- Van Boven, R. W.; Johnson, K. O. (December 1994). "The limit of tactile spatial resolution in humans: grating orientation discrimination at the lip, tongue, and finger". Neurology. 44 (12): 2361–2366. doi:10.1212/wnl.44.12.2361. ISSN 0028-3878. PMID 7991127. S2CID 32255147.
- Craig, J. C.; Lyle, K. B. (February 2001). "A comparison of tactile spatial sensitivity on the palm and fingerpad". Perception & Psychophysics. 63 (2): 337–347. doi:10.3758/bf03194474. ISSN 0031-5117. PMID 11281108.
- Tremblay, François; Wong, Kim; Sanderson, Robin; Coté, Leanne (2003-01-01). "Tactile spatial acuity in elderly persons: assessment with grating domes and relationship with manual dexterity". Somatosensory & Motor Research. 20 (2): 127–132. doi:10.1080/0899022031000105154. ISSN 0899-0220. PMID 12850821. S2CID 30087810.
- Bleyenheuft, Yannick; Cols, Caroline; Arnould, Carlyne; Thonnard, Jean-Louis (2006-01-01). "Age-related changes in tactile spatial resolution from 6 to 16 years old". Somatosensory & Motor Research. 23 (3–4): 83–87. doi:10.1080/08990220600816440. hdl:2078.1/10805. ISSN 0899-0220. PMID 17178543. S2CID 25349399.
- Peters, Ryan M.; Goldreich, Daniel (2013-12-19). "Tactile Spatial Acuity in Childhood: Effects of Age and Fingertip Size". PLOS ONE. 8 (12): e84650. Bibcode:2013PLoSO...884650P. doi:10.1371/journal.pone.0084650. ISSN 1932-6203. PMC 3891499. PMID 24454612.
- Peters, Ryan M.; Hackeman, Erik; Goldreich, Daniel (2009-12-16). "Diminutive Digits Discern Delicate Details: Fingertip Size and the Sex Difference in Tactile Spatial Acuity". Journal of Neuroscience. 29 (50): 15756–15761. doi:10.1523/jneurosci.3684-09.2009. PMC 3849661. PMID 20016091.
- Vega-Bermudez, Francisco; Johnson, Kenneth O. (January 2004). "Fingertip skin conformance accounts, in part, for differences in tactile spatial acuity in young subjects, but not for the decline in spatial acuity with aging". Perception & Psychophysics. 66 (1): 60–67. doi:10.3758/bf03194861. ISSN 0031-5117. PMID 15095940.
- Van Boven, R. W.; Hamilton, R. H.; Kauffman, T.; Keenan, J. P.; Pascual-Leone, A. (2000-06-27). "Tactile spatial resolution in blind braille readers". Neurology. 54 (12): 2230–2236. doi:10.1212/wnl.54.12.2230. ISSN 0028-3878. PMID 10881245. S2CID 12053536.
- Wong, Michael; Gnanakumaran, Vishi; Goldreich, Daniel (2011-05-11). "Tactile Spatial Acuity Enhancement in Blindness: Evidence for Experience-Dependent Mechanisms". Journal of Neuroscience. 31 (19): 7028–7037. doi:10.1523/jneurosci.6461-10.2011. PMC 6703211. PMID 21562264.
- Wong, Michael; Peters, Ryan M.; Goldreich, Daniel (2013-05-29). "A Physical Constraint on Perceptual Learning: Tactile Spatial Acuity Improves with Training to a Limit Set by Finger Size". Journal of Neuroscience. 33 (22): 9345–9352. doi:10.1523/jneurosci.0514-13.2013. PMC 6618562. PMID 23719803.
- Harrar, Vanessa; Spence, Charles; Makin, Tamar R. (2014). "Topographic generalization of tactile perceptual learning". Journal of Experimental Psychology: Human Perception and Performance. 40 (1): 15–23. doi:10.1037/a0033200. PMID 23855526.