Ulnar collateral ligament injury of the elbow
Ulnar collateral ligament injuries can occur during certain activities such as overhead baseball pitching. Acute or chronic disruption and/or attenuation of the ulnar collateral ligament often result in medial elbow pain, valgus instability, neurologic deficiency, and impaired throwing performance. There are both non-surgical and surgical treatment options.[1]
| Ulnar collateral ligament injury of the elbow | |
|---|---|
 | |
| Location of UCL injury | |
| Specialty | Orthopedic |
Signs and symptoms
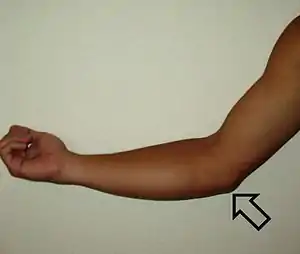
Pain along the inside of the elbow is the main symptom of this condition. Throwing athletes report it occurs most often during the acceleration phase of throwing. Closing the hand and clenching the fist has also been shown to reproduce the painful symptoms. The injury is often associated with an experience of a sharp “pop” in the elbow, followed by pain during a single throw.[2] In addition, swelling and bruising of the elbow, loss of elbow range of motion, and a sudden decrease in throwing velocity are all common symptoms of a UCL injury. If the injury is less severe, pain can be minimal with complete rest.[3]
Causes
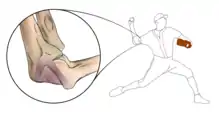
The UCL is important because it stabilizes the elbow from being abducted. If intense or repeated bouts of valgus stress occur on the UCL, injury will most likely transpire. Damage to the ulnar collateral ligament is common among baseball pitchers and javelin throwers because the throwing motion is similar. Physicians believe repetitive movements, especially pitching in baseball, cause adolescents' UCL injuries. Furthermore, physicians have stated that if an adolescent throws over 85 throws for 8 months or more in a year, or throw when exhausted, the adolescent has a significantly higher risk of succumbing to a UCL surgery.[4] Gridiron football, racquet sports, ice hockey and water polo players have also been treated for damage to the ulnar collateral ligament.[5][6] Specific overhead movements like those that occur during baseball pitching, tennis serving or volleyball spiking increase the risk of UCL injury.[7] During the cocking phase of pitching, the shoulder is horizontally abducted, externally rotated and the elbow is flexed. There is slight stress on the UCL in this position but it increases when the shoulder is further externally rotated. The greater the stress the more the UCL is stretched causing strain. During the overhead throwing motion, valgus stress on the medial elbow occurs during arm cocking and acceleration. The initiation of valgus stress occurs at the conclusion of the arm-cocking phase. In the transitional moment from arm cocking to arm acceleration, the shoulder vigorously rotates internally, the forearm is in near full supination, and the elbow flexes from 90° to approximately 125°. From late cocking to ball release, the elbow rapidly extends from approximately 125° to 25° at ball release.[8] This causes tremendous valgus stress and tensile strain on the UCL. Injuries to the ulnar collateral ligament are believed to result from poor throwing mechanics, overuse, high throwing velocities, and throwing certain types of pitches, such as curveballs. Poor mechanics along with high repetition of these overhead movements can cause irritation, micro-tears or ruptures of the UCL. Kinetic chain dysfunction due to poor lower extremity strength, core strength and stability can be associated with UCL injuries as well as capsular stiffness in glenohumeral internal rotation deficit (GIRD), and scapular dyskinesis.[9][10] Injuries to the Ulnar Collateral Ligament in baseball players are rarely due to one-time, traumatic events. Rather, they are more often due to small chronic tears that accumulate over time.
Anatomy
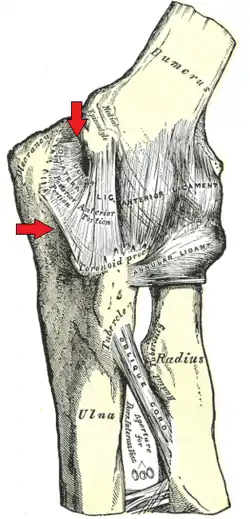
The ulnar collateral ligament (UCL, also known as medial collateral ligament) is located on the medial side of the elbow. The UCL complex comprises three ligaments: the anterior oblique, posterior oblique and transverse ligaments.[11] The anterior oblique ligament (AOL) attaches from the undersurface of the medial epicondyle to the medial ulnar surface slightly below the coronoid process.[12] It is the sturdiest of the three sections within the UCL. The AOL acts as the primary restraint against valgus stress at the elbow during flexion and extension. The posterior oblique originates at the medial epicondyle and inserts along the mid-portion of the medial semilunar notch.[11] It applies more stability against valgus stress when the elbow is flexed rather than extended. The transverse ligament connects to the inferior medial coronoid process of the ulna to the medial tip of the olecranon.[11] Since it is connected to the same bone and not across the elbow joint, the transverse ligament has no contribution to the joint’s stability.
Diagnosis
In most cases, a physician will diagnose an ulnar collateral ligament injury using a patient’s medical history and a physical examination that includes a valgus stress test. The valgus stress test is performed on both arms and a positive test is indicated by pain on the affected arm that is not present on the uninvolved side.[13][14] Physicians often utilize imaging techniques such as ultrasound, x-rays and magnetic resonance imaging or arthroscopic surgery to aid with making a proper diagnosis.
Classification
A slow and chronic deterioration of the ulnar collateral ligament can be due to repetitive stress acting on the ulna. At first, pain can be bearable and can worsen to an extent where it can terminate an athlete’s career. The repetitive stress placed on the ulna causes micro tears in the ligament resulting in the loss of structural integrity over time.[15] The acute rupture is less common compared to the slow deterioration injury. The acute rupture occurs in collisions when the elbow is in flexion such as that in a wrestling match or a tackle in football. The ulnar collateral ligament distributes over fifty percent of the medial support of the elbow.[16][17] This can result in an ulnar collateral ligament injury or a dislocated elbow causing severe damage to the elbow and the radioulnar joints.
Treatments


UCL injuries may or may not require surgery. Non surgical treatment will primarily focus on strengthening the elbow joint to regain strength and stability.[18] First a course of RICE (Rest, ice, compression, elevation) is typically coupled with NSAIDS (Non-steroidal anti-inflammatory drugs) to help alleviate pain and swelling. When the swelling has subsided, individual exercises or physical therapy may be prescribed to strengthen muscles around the elbow joint to compensate for tearing in the UCL.[18] These may include biceps curls (non resistance and resistance), pronating and supinating the forearm, and grip strengthening exercises, performed with low resistance and moderate repetitions no more than three times a week.[19]
Surgical treatment may help restore the ability to perform the overhand throwing motions most commonly associated with UCL injuries. The reconstructive surgery, generally known as Tommy John surgery, was first performed by Dr. Frank Jobe in 1974 and has modified several times over the past 30 years.[20][21] The surgery involves an autograft of the palmaris longus tendon (mostly seen as an accessory tendon) or an allograft of tissue from a cadaver or donor. The new tendon is attached by drilling holes in the medial epicondyle of the humerus and the sublime tubercle of the ulna and lacing the tendon through them in a figure eight.[18][5] The patient may begin physical therapy shortly after. It usually takes about 15 months after the surgery for standard rehabilitation. Rehabilitation following UCL injuries or surgery should follow a sequential and progressive multi-phased approach that involves a gradual and protected return of range-of-motion (ROM). The rehab program should include proprioceptive exercises to stimulate mechanoreceptors as well as arm strengthening, emphasizing proximal scapular stabilization. Low-resistance, high-repetition programs promote an optimal return to uncompensated throwing.[22] Post-operative treatment is related to the restoration of normal scapulohumeral rhythm, which begins with establishing trunk stability, elbow range of motion and strength as well as balance exercises.[22] In study conducted by Dr. Frederick Azar, 78 Tommy John surgeries were performed and analyzed after the surgeries. Of the 78 patients, 8 of them (8.8%) reported complications. Two patients had superficial infections that resolved with oral antibiotics, two patients reported tightness of tenderness at the surgery site, and one had a superficial wound infection at the elbow incision that resolved with oral antibiotics. One patient developed postoperative ulnar nerve damage. Two patients had damages to the posteromedial part of the olecranon and required to have reoperation.[23]
Recent studies have shown that MLB pitchers who undergo Tommy John surgery return to pitch in the MLB 83% of the time and only 3% fail to return to pitch in the MLB or the minor league.[20]
Recently, there has been a recorded increase of Tommy John surgery. The increase is related to the false perception that the surgery improves the stability of the UCL joint. Many athletes believe in this false perception and cause them to lie about their symptoms in hopes to undergo the surgery. In order to combat these rumors, physicians are motivated to educate the public that Tommy John surgeries are only for those who have severe UCL injuries. The surgery will have an insignificant effect if the patient does not have a severe UCL injury.[24]
The tendon chosen is then woven in a figure eight pattern through the humerus and ulna, which holes were first drilled in the bones.[25] After surgery occurs, rehabilitation comes into place and usually takes about a year because a tendon needs time to convert into a ligament.[26]
Epidemiology
According to the International Classification of Diseases, 9th Revision, Clinical Modification, ICD-9-CM, in 2008 the U.S. listed the diagnosis code for UCL injury as 841.1: Sprain ulnar collateral ligament. There were a total of 336 discharges of UCL injuries. Within the total discharges, separated by age groups: 18- to 44-year-olds; 165 people (49.17%). 45- to 64-year-olds; 91 (27.08%). 65- to 84-year-olds, 65 (19.35%) it shows that the ulnar collateral ligament injuries were more commonly found in men than women. There were 213 men compared to 123 women with ulnar collateral ligament injury. Most of these injuries were also paid through private insurance (170: 50.63%) and Medicare (70: 20.85%).[27] The average estimated cost for the surgery also known as Tommy John surgery is $21,563.[28]
References
- Hoffman JK, Protzman NM, Malhotra AD (2015). "Biologic Augmentation of the Ulnar Collateral Ligament in the Elbow of a Professional Baseball Pitcher". Case Reports in Orthopedics. 2015: 130157. doi:10.1155/2015/130157. PMC 4512595. PMID 26240769.
- Ulnar Collateral Ligament Injury at eMedicine
- Anderson B (2010). "Ulnar collateral ligament sprain". Sports Injury Info.
- Fleisig GS, Weber A, Hassell N, Andrews JR (September 2009). "Prevention of elbow injuries in youth baseball pitchers". Current Sports Medicine Reports. 8 (5): 250–4. doi:10.1249/JSR.0b013e3181b7ee5f. PMC 3435945. PMID 19741352.
- Edell D. "UCL Injuries". The Athletic Advisor. Archived from the original on 17 July 2010.
- Mirowitz SA, London SL (November 1992). "Ulnar collateral ligament injury in baseball pitchers: MR imaging evaluation". Radiology. 185 (2): 573–6. doi:10.1148/radiology.185.2.1410375. PMID 1410375.
- Hariri S, Safran MR (October 2010). "Ulnar collateral ligament injury in the overhead athlete". Clinics in Sports Medicine. 29 (4): 619–44. doi:10.1016/j.csm.2010.06.007. PMID 20883901.
- Fleisig GS, Escamilla RF (April 1996). "Biomechanics of the elbow in the throwing athlete". Operative Techniques in Sports Medicine. 4 (2): 62–8. doi:10.1016/S1060-1872(96)80050-5.
- Cascia N, Picha K, Hettrich CM, Uhl TL (2019-06-13). "Considerations of Conservative Treatment After a Partial Ulnar Collateral Ligament Injury in Overhead Athletes: A Systematic Review". Sports Health. 11 (4): 367–374. doi:10.1177/1941738119853589. PMC 6600583. PMID 31194648.
- Redler LH, Degen RM, McDonald LS, Altchek DW, Dines JS (April 2016). "Elbow ulnar collateral ligament injuries in athletes: Can we improve our outcomes?". World Journal of Orthopedics. 7 (4): 229–43. doi:10.5312/wjo.v7.i4.229. PMC 4832224. PMID 27114930.
- Safran M, Ahmad CS, Elattrache NS (November 2005). "Ulnar collateral ligament of the elbow". Arthroscopy. 21 (11): 1381–95. doi:10.1016/j.arthro.2005.07.001. PMID 16325092.
- Zarins B, Andrews JR, Carson WG (1985). Injuries to the throwing arm: based on the proceedings of the national conference. Philadelphia: Saunders. ISBN 0-7216-1416-7.
- "Athletic Injury Examination Special/Stress Tests for the Elbow". The University of West Alabama.
- O'Driscoll SW, Lawton RL, Smith AM (February 2005). "The "moving valgus stress test" for medial collateral ligament tears of the elbow". The American Journal of Sports Medicine. 33 (2): 231–9. doi:10.1177/0363546504267804. PMID 15701609. S2CID 25744733.
- Morrey BF, An KN (1983). "Articular and ligamentous contributions to the stability of the elbow joint". The American Journal of Sports Medicine. 11 (5): 315–9. doi:10.1177/036354658301100506. PMID 6638246. S2CID 25478080.
- Hotchkiss RN, Weiland AJ (1987). "Valgus stability of the elbow". Journal of Orthopaedic Research. 5 (3): 372–7. doi:10.1002/jor.1100050309. PMID 3625360. S2CID 46543114.
- Maloney MD, Mohr KJ, el Attrache NS (October 1999). "Elbow injuries in the throwing athlete. Difficult diagnoses and surgical complications". Clinics in Sports Medicine. 18 (4): 795–809. doi:10.1016/S0278-5919(05)70185-X. PMID 10553236.
- "Patient Guide to UCL Injuries of the Elbow (Ulnar Collateral Ligament)". Johns Hopkins Sports Medicine. Archived from the original on 3 April 2012.
- Ulnar Collateral Ligament Injury~treatment at eMedicine
- Erickson, Brandon J. "The epidemic of Tommy John surgery: the role of the orthopedic surgeon." Am J Orthop (Belle Mead NJ) 44.1 (2015): E36-37.
- Molenaars RJ, Hilgersom NF, Doornberg JN, van den Bekerom MP, Eygendaal D (2017-11-02). "Review of Jobe et al (1986) on reconstruction of the ulnar collateral ligament in athletes". Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine. 3: jisakos–2017–000134. doi:10.1136/jisakos-2017-000134. ISSN 2059-7754.
- Redler LH, Degen RM, McDonald LS, Altchek DW, Dines JS (April 2016). "Elbow ulnar collateral ligament injuries in athletes: Can we improve our outcomes?". World Journal of Orthopedics. 7 (4): 229–43. doi:10.5312/wjo.v7.i4.229. PMC 4832224. PMID 27114930.
- Azar FM, Andrews JR, Wilk KE, Groh D (2000). "Operative treatment of ulnar collateral ligament injuries of the elbow in athletes". The American Journal of Sports Medicine. 28 (1): 16–23. doi:10.1177/03635465000280011401. PMID 10653538. S2CID 11494166.
- Longman J (20 July 2007). "Fit young pitchers see elbow repair as cure-all". The New York Times.
- Bernas GA, Ruberte Thiele RA, Kinnaman KA, Hughes RE, Miller BS, Carpenter JE (December 2009). "Defining safe rehabilitation for ulnar collateral ligament reconstruction of the elbow: a biomechanical study". The American Journal of Sports Medicine. 37 (12): 2392–400. doi:10.1177/0363546509340658. PMID 19684292. S2CID 35255305.
- Ellenbecker TS, Mattalino AJ (1997). The elbow in sport: injury, treatment, and rehabilitation. Champaign, IL: Human Kinetics. ISBN 0-87322-897-9.
- U.S. Department of Health & Human Services: Agency for Healthcare Research and Quality - Advancing Excellence in Health Care. "HCUPnet: A tool for identifying, tracking, and analyzing national hospital statistics". Archived from the original on 2015-03-01. Retrieved 2015-03-01..
- "Ulnar Collateral Ligament Reconstruction Surgery Cost". SurgeryCost.net. Archived from the original on 14 March 2012.