Vas deferens
The vas deferens or ductus deferens is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymis to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.
| Vas deferens | |
|---|---|
 Male anatomy | |
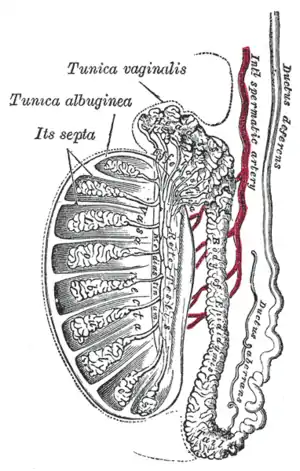 Vertical section of the testis, to show the arrangement of the ducts | |
| Details | |
| Precursor | Wolffian duct |
| Artery | Superior vesical artery, artery of the ductus deferens |
| Lymph | External iliac lymph nodes, internal iliac lymph nodes |
| Identifiers | |
| Latin | Vas deferens (plural: vasa deferentia), Ductus deferens (plural: ductus deferentes) |
| MeSH | D014649 |
| TA98 | A09.3.05.001 |
| TA2 | 3621 |
| FMA | 19234 |
| Anatomical terminology | |
Etymology
Vas deferens is Latin, meaning "carrying-away vessel"; the plural version is vasa deferentia. Ductus deferens is also Latin, meaning "carrying-away duct"; the plural version is ducti deferentes.[1]
Structure
There are two vasa deferentia, connecting the left and right epididymis with the seminal vesicles to form the ejaculatory duct in order to move sperm.[2]
The (human) vas deferens measures 30-35 cm in length, and 2-3 mm in diameter.[3]: 1297
The vas deferens is continuous proximally with the tail of the epididymis.[3]: 1296 The vas deferens exhibits a tortuous, convoluted initial/proximal section (which measures 2-3 cm in length). Distally, it forms a dilated and tortuous segment termed the ampulla of vas deferens before ending[3]: 1297 by uniting with a duct of the seminal vesicle to form the ejaculatory duct.[2]
The vas deferens forms part of the spermatic cord.[4]
Blood supply
The vas deferens is supplied by an accompanying artery (artery of vas deferens). This artery normally arises from the superior (sometimes inferior) vesical artery, a branch of the internal iliac artery.[5]
Innervation
The vas deferens receives innervation from an autonomic plexus of post-ganglionic sympathetic fibres derived from the inferior hypogastric plexus.[3]: 1297
The vas deferens is innervated by a variety of different types of nerve ending. Adrenergic synapses are found in the smooth muscle layers. Cholinergic synapses and vasoactive intestinal peptide synapses are found in the connective tissue of the mucosa.[6] Noradrenergic synapses may also be present in the vas deferens.[7]
Anatomical relations
Within the spermatic cord, the vas deferens is situated posterior (and parallel to) the vessels of the spermatic cord.[3]: 1297
The vas deferens traverses the inguinal canal to reach the pelvic cavity; it enters the pelvic cavity lateral to the inferior epigastric vessels. At the deep inguinal ring, the vas deferens diverges from the testicular vessels to pass medially to reach the base of the prostate posteriorly.[3]: 1297
Histology
The vas deferens consists of an external adventitial sheath containing blood vessels and nerves, a muscular middle layer composed of three layers of smooth muscle (with a circular muscle layer interposed between two longitudinal muscle layers), and an internal mucosal lining consisting of pseudostratified columnar epithelium (which bears non-motile cilia).[3]: 1297
The vas deferens has the greatest muscle-to-lumen ratio of any hollow organ.[3]: 1297
Function
During ejaculation, the smooth muscle in the walls of the vas deferens contracts reflexively, thus propelling the sperm forward. This is also known as peristalsis.[8] The sperm is transferred from each vas deferens into the urethra, partially mixing with secretions from the male accessory sex glands such as the seminal vesicles, prostate gland and the bulbourethral glands, which form the bulk of semen.[9]
Clinical significance
Contraception
A vasectomy is a method of contraception in which the vasa deferentia are permanently cut, though in some cases it can be reversed. A modern variation, vas-occlusive contraception, involves injecting an obstructive material into the ductus to block the flow of sperm.[10]
Disease
The vas deferens may be obstructed, or it may be completely absent in a condition known as congenital absence of the vas deferens (CAVD, a potential feature of cystic fibrosis), causing male infertility. Acquired obstructions can occur due to infections. To treat these causes of male infertility, sperm can be harvested by testicular sperm extraction (TESE) or microsurgical epididymal sperm aspiration (MESA).[11]
Uses in pharmacology and physiology
The vas deferens has a dense sympathetic innervation,[12] making it a useful system for studying sympathetic nerve function and for studying drugs that modify neurotransmission.[13]
It has been used:
- as a bioassay for the discovery of enkephalins, the endogenous opiates.[14]
- to demonstrate quantal transmission from sympathetic nerve terminals.[15]
- as the first direct measure of free Ca2+ concentration in a postganglionic nerve terminal.[16]
- to develop an optical method for monitoring packeted transmission (similar to quantal transmission).[17]
Other animals
Most vertebrates have some form of duct to transfer the sperm from the testes to the urethra. In cartilaginous fish and amphibians, sperm is carried through the archinephric duct, which also partially helps to transport urine from the kidneys. In teleosts, there is a distinct sperm duct, separate from the ureters, and often called the vas deferens, although probably not truly homologous with that in humans.[18] The vas deferens loops over the ureter in placental mammals, but not in marsupial mammals.[19][20]
In cartilaginous fishes, the part of the archinephric duct closest to the testis is coiled up to form an epididymis. Below this are a number of small glands secreting components of the seminal fluid. The final portion of the duct also receives ducts from the kidneys in most species.[18]
In amniotes, however, the archinephric duct has become a true vas deferens, and is used only for conducting sperm, never urine. As in cartilaginous fish, the upper part of the duct forms the epididymis. In many species, the vas deferens ends in a small sac for storing sperm.[18]
The only vertebrates to lack any structure resembling a vas deferens are the primitive jawless fishes, which release sperm directly into the body cavity, and then into the surrounding water through a simple opening in the body wall.[18]
Additional images
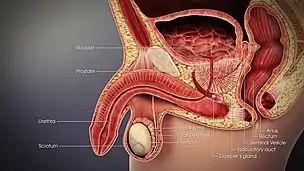
 Male reproductive system.
Male reproductive system. Coronal section of pelvis, showing arrangement of fasciae. Viewed from behind.
Coronal section of pelvis, showing arrangement of fasciae. Viewed from behind. The relations of the femoral and abdominal inguinal rings, seen from within the abdomen. Right side.
The relations of the femoral and abdominal inguinal rings, seen from within the abdomen. Right side. The spermatic cord in the inguinal canal.
The spermatic cord in the inguinal canal. Fundus of the bladder with the vesiculae seminales.
Fundus of the bladder with the vesiculae seminales.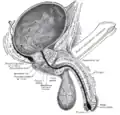 Vertical section of bladder, penis, and urethra.
Vertical section of bladder, penis, and urethra.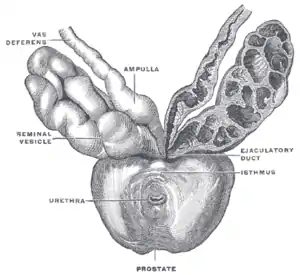 Prostate with seminal vesicles and seminal ducts, viewed from in front and above.
Prostate with seminal vesicles and seminal ducts, viewed from in front and above.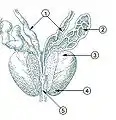 Prostate
Prostate Microscopic cross section.
Microscopic cross section. Testis, spermatic vessels and vas deferens
Testis, spermatic vessels and vas deferens A deep dissection showing the vas deferens.
A deep dissection showing the vas deferens.
See also
- Intra vas device
- Excretory duct of seminal gland
- Vas deferens in the reproductive system of gastropods
References
- Pozor, Malgorzata (2022). "Seminal Vesiculitis". Comparative Veterinary Anatomy: 825–833. doi:10.1016/B978-0-323-91015-6.00067-4.
- Gonzales, GF (December 2001). "Function of seminal vesicles and their role on male fertility". Asian journal of andrology. 3 (4): 251–8. PMID 11753468.
- Gray's anatomy : the anatomical basis of clinical practice. Susan Standring (Forty-second ed.). [New York]. 2021. ISBN 978-0-7020-7707-4. OCLC 1201341621.
{{cite book}}: CS1 maint: others (link) - Liu, Longfei (2019). "Chapter 1 - Applied Anatomy of the Scrotum and its Contents". Scrotoscopic Surgery. Academic Press. pp. 1–8. doi:10.1016/B978-0-12-815008-5.00001-7. ISBN 978-0-12-815008-5. S2CID 81721236.
- One or more of the preceding sentences incorporates text in the public domain from page 615 of the 20th edition of Gray's Anatomy (1918)
- Alm, Per (1982-07-01). "On the autonomic innervation of the human vas deferens". Brain Research Bulletin. Elsevier. 9 (1–6): 673–677. doi:10.1016/0361-9230(82)90172-1. ISSN 0361-9230. PMID 6184134. S2CID 4761228.
- Mirabella, Nicola; Squillacioti, Caterina; Varricchio, Ettore; Genovese, Angelo; Paino, Giuseppe (2003-05-01). "Innervation of vas deferens and accessory male genital glands in the water buffalo (Bubalus bubalis): Neurochemical characteristics and relationships to the reproductive activity". Theriogenology. 59 (9): 1999–2016. doi:10.1016/S0093-691X(02)01260-8. ISSN 0093-691X. PMID 12600736 – via Elsevier.
- Berridge, Michael J. (2008). "Smooth muscle cell calcium activation mechanisms". The Journal of Physiology. 586 (21): 5047–5061. doi:10.1113/jphysiol.2008.160440. PMC 2652144. PMID 18787034.
- Mann, T (1954). The Biochemistry of Semen. London: Methuen & Co; New York: John Wiley & Sons. Retrieved November 9, 2013.
- Cook, Lynley A; Van Vliet, Huib AAM; Lopez, Laureen M; Pun, Asha; Gallo, Maria F (2014). "Vasectomy occlusion techniques for male sterilization". Cochrane Database of Systematic Reviews (3): CD003991. doi:10.1002/14651858.CD003991.pub4. PMC 7173716. PMID 24683020.
- Schroeder-Printzen, I. (1 December 2000). "Microsurgical epididymal sperm aspiration: aspirate analysis and straws available after cryopreservation in patients with non-reconstructable obstructive azoospermia". Human Reproduction. 15 (12): 2531–2535. doi:10.1093/humrep/15.12.2531.
- Sjöstrand, N.O. (1965). "The adrenergic innervation of the vas deferens and the accessory male genital organs". Acta Physiologica Scandinavica. 257: S1–82.
- Burnstock, G; Verkhratsky, A (2010). "Vas deferens--a model used to establish sympathetic cotransmission". Trends in Pharmacological Sciences. 31 (3): 131–9. doi:10.1016/j.tips.2009.12.002. PMID 20074819.
- Hughes, J; Smith, T. W.; Kosterlitz, H. W.; Fothergill, L. A.; Morgan, B. A.; Morris, H. R. (1975). "Identification of two related pentapeptides from the brain with potent opiate agonist activity". Nature. 258 (5536): 577–80. Bibcode:1975Natur.258..577H. doi:10.1038/258577a0. PMID 1207728. S2CID 95411.
- Brock, J. A.; Cunnane, T. C. (1987). "Relationship between the nerve action potential and transmitter release from sympathetic postganglionic nerve terminals". Nature. 326 (6113): 605–7. Bibcode:1987Natur.326..605B. doi:10.1038/326605a0. PMID 2882426. S2CID 4303337.
- Brain, K. L.; Bennett, M. R. (1997). "Calcium in sympathetic varicosities of mouse vas deferens during facilitation, augmentation and autoinhibition". The Journal of Physiology. 502 (3): 521–36. doi:10.1111/j.1469-7793.1997.521bj.x. PMC 1159525. PMID 9279805.
- Brain, K. L.; Jackson, V. M.; Trout, S. J.; Cunnane, T. C. (2002). "Intermittent ATP release from nerve terminals elicits focal smooth muscle Ca2+ transients in mouse vas deferens". The Journal of Physiology. 541 (Pt 3): 849–62. doi:10.1113/jphysiol.2002.019612. PMC 2290369. PMID 12068045.
- Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 393–395. ISBN 978-0-03-910284-5.
- C. Hugh Tyndale-Biscoe (2005). Life of Marsupials. Csiro Publishing. ISBN 978-0-643-06257-3.
- Patricia J. Armati; Chris R. Dickman; Ian D. Hume (17 August 2006). Marsupials. Cambridge University Press. ISBN 978-1-139-45742-2.
External links
- Anatomy photo:36:07-0301 at the SUNY Downstate Medical Center—"Inguinal Region, Scrotum and Testes: Layers of the Spermatic Cord"
- Anatomy photo:44:02-0301 at the SUNY Downstate Medical Center—"The Male Pelvis: Distribution of the Peritoneum in the Male Pelvis"
- MedicalMnemonics.com: 2424 319
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- inguinalregion at The Anatomy Lesson by Wesley Norman (Georgetown University) (testes)