Goitre
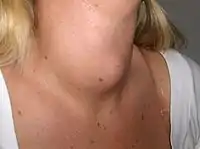
A goitre, or goiter, is a swelling in the neck resulting from an enlarged thyroid gland.[1][2] A goitre can be associated with a thyroid that is not functioning properly.
| Goitre | |
|---|---|
| Other names | Goiter |
 | |
| Diffuse hyperplasia of the thyroid | |
| Specialty | Endocrinology |
Worldwide, over 90% of goitre cases are caused by iodine deficiency.[3] The term is from the Latin gutturia, meaning throat. Most goitres are not cancerous (benign), though they may be potentially harmful.
Signs and symptoms
A goitre can present as a palpable or visible enlargement of the thyroid gland at the base of the neck. A goitre, if associated with hypothyroidism or hyperthyroidism, may be present with symptoms of the underlying disorder. For hyperthyroidism, the most common symptoms are associated with adrenergic stimulation: tachycardia (increased heart rate), palpitations, nervousness, tremor, increased blood pressure and heat intolerance. Clinical manifestations are often related to hypermetabolism, (increased metabolism), excessive thyroid hormone, an increase in oxygen consumption, metabolic changes in protein metabolism, immunologic stimulation of diffuse goitre, and ocular changes (exophthalmos).[4] Hypothyroid people commonly have poor appetite, cold intolerance, constipation, lethargy and may undergo weight gain. However, these symptoms are often non-specific and make diagnosis difficult.
According to the WHO classification of goitre by palpation, the severity of goitre is currently graded as grade 0, grade 1, grade 2.[5]
 Goitre Class I
Goitre Class I Goitre Class II
Goitre Class II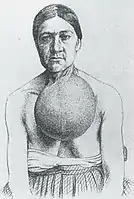 Goitre Class III
Goitre Class III
Causes
Worldwide, the most common cause for goitre is iodine deficiency, commonly seen in countries that scarcely use iodized salt. Selenium deficiency is also considered a contributing factor. In countries that use iodized salt, Hashimoto's thyroiditis is the most common cause.[6] Goitre can also result from cyanide poisoning, which is particularly common in tropical countries where people eat the cyanide-rich cassava root as the staple food.[7]
| Cause | Pathophysiology | Resultant thyroid activity | Growth pattern | Treatment | Incidence and prevalence | Prognosis |
|---|---|---|---|---|---|---|
| Iodine deficiency | Hyperplasia of thyroid to compensate for decreased efficacy | Can cause hypothyroidism | Diffuse | Iodine | Constitutes over 90% cases of goitre worldwide[3] | Increased size of thyroid may be permanent if untreated for around five years |
| Congenital hypothyroidism | Inborn errors of thyroid hormone synthesis | Hypothyroidism | ||||
| Goitrogen ingestion | ||||||
| Adverse drug reactions | ||||||
| Hashimoto's thyroiditis | Autoimmune disease in which the thyroid gland is gradually destroyed. Infiltration of lymphocytes. | Hypothyroidism | Diffuse and lobulated[8] | Thyroid hormone replacement | Prevalence: 1 to 1.5 in a 1000 | Remission with treatment |
| Pituitary disease | Hypersecretion of thyroid stimulating hormone, almost always by a pituitary adenoma[9] | Diffuse | Pituitary surgery | Very rare[9] | ||
| Graves' disease—also called Basedow syndrome | Autoantibodies (TSHR-Ab) that activate the TSH-receptor (TSHR) | Hyperthyroidism | Diffuse | Antithyroid agents, radioiodine, surgery | Will develop in about 0.5% of males and 3% of females | Remission with treatment, but still lower quality of life for 14 to 21 years after treatment, with lower mood and lower vitality, regardless of the choice of treatment[10] |
| Thyroiditis | Acute or chronic inflammation | Can be hyperthyroidism initially, but progress to hypothyroidism | ||||
| Thyroid cancer | Usually uninodular | Overall relative 5-year survival rate of 85% for females and 74% for males[11] | ||||
| Benign thyroid neoplasms | Usually hyperthyroidism | Usually uninodular | Mostly harmless[12] | |||
| Thyroid hormone insensitivity | Secretional hyperthyroidism, Symptomatic hypothyroidism | Diffuse |
- Sarcoidosis
- Amyloidosis
- Hydatidiform mole
- Cysts
- Acromegaly
- Pendred syndrome
Diagnosis
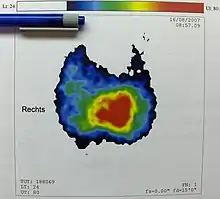
Goitre may be diagnosed via a thyroid function test in an individual suspected of having it.[13]
Types
A goitre may be classified either as nodular or diffuse. Nodular goitres are either of one nodule (uninodular) or of multiple nodules (multinodular).[14]
- Growth pattern
- Uninodular goitre: one thyroid nodule; can be either inactive, or active (toxic) – autonomously producing thyroid hormone.
- Multinodular goitre: multiple nodules;[15] can likewise be inactive or toxic, the latter is called toxic multinodular goitre and associated with hyperthyroidism. These nodules grow up at varying rates and secrete thyroid hormone autonomously, thereby suppressing TSH-dependent growth and function in the rest of gland. Inactive nodules in the same goitre can be malignant.[16] Thyroid cancer is identified in 13.7% of the patients operated for multinodular goitre.[17]
- Diffuse goitre: the whole thyroid appearing to be enlarged due to hyperplasia.
- Size
- Class I: the goitre in normal posture of the head cannot be seen; it is only found by palpation.
- Class II: the goitre is palpable and can be easily seen.
- Class III: the goitre is very large and is retrosternal (partially or totally lying below the sternum), pressure results in compression marks.
Treatment
Goitre is treated according to the cause. If the thyroid gland is producing an excess of thyroid hormones (T3 and T4), radioactive iodine is given to the patient to shrink the gland. If goitre is caused by iodine deficiency, small doses of iodide in the form of Lugol's iodine or KI solution are given. If the goitre is associated with an underactive thyroid, thyroid supplements are used as treatment. Sometimes a partial or complete thyroidectomy is required.[18]
Epidemiology

Goitre is more common among women, but this includes the many types of goitre caused by autoimmune problems, and not only those caused by simple lack of iodine.[20]
History


Chinese physicians of the Tang Dynasty (618–907) were the first to successfully treat patients with goitre by using the iodine-rich thyroid gland of animals such as sheep and pigs—in raw, pill, or powdered form.[21] This was outlined in Zhen Quan's (d. 643 AD) book, as well as several others.[21] One Chinese book, The Pharmacopoeia of the Heavenly Husbandman, asserted that iodine-rich sargassum was used to treat goitre patients by the 1st century BC, but this book was written much later.[21]
In the 12th century, Zayn al-Din al-Jurjani, a Persian physician, provided the first description of Graves' disease after noting the association of goitre and a displacement of the eye known as exophthalmos in his Thesaurus of the Shah of Khwarazm, the major medical dictionary of its time.[22][23] The disease was later named after Irish doctor Robert James Graves, who described a case of goitre with exophthalmos in 1835. The German Karl Adolph von Basedow also independently reported the same constellation of symptoms in 1840, while earlier reports of the disease were also published by the Italians Giuseppe Flajani and Antonio Giuseppe Testa, in 1802 and 1810 respectively,[24] and by the English physician Caleb Hillier Parry (a friend of Edward Jenner) in the late 18th century.[25]
Paracelsus (1493–1541) was the first person to propose a relationship between goitre and minerals (particularly lead) in drinking water.[26] Iodine was later discovered by Bernard Courtois in 1811 from seaweed ash.[27]
Goitre was previously common in many areas that were deficient in iodine in the soil. For example, in the English Midlands, the condition was known as Derbyshire Neck. In the United States, goitre was found in the Appalachian,[28][29] Great Lakes, Midwest, and Intermountain regions. The condition is now practically absent in affluent nations, where table salt is supplemented with iodine. However, it is still prevalent in India, China,[30] Central Asia, and Central Africa.
Goitre had been prevalent in the alpine countries for a long time. Switzerland reduced the condition by introducing iodised salt in 1922. The Bavarian tracht in the Miesbach and Salzburg regions, which appeared in the 19th century, includes a choker, dubbed Kropfband (struma band) which was used to hide either the goitre or the remnants of goitre surgery.[31]
Society and culture
In the 1920s wearing bottles of iodine around the neck was believed to prevent goitre.[32]
Notable cases
- Former U.S. President George H. W. Bush and his wife Barbara Bush were both diagnosed with Graves' disease and goitres, within two years of each other. The disease caused hyperthyroidism and cardiac dysrhythmia.[33][34] Scientists said that, absent an environmental cause, the odds of both a husband and wife having Graves' disease might be 1 in 100,000 or as low as 1 in 3,000,000.[35]
See also
References
- "Thyroid Nodules and Swellings". British Thyroid Foundation.
- "Goitre - NHS Choices". NHS Choices. 2017-10-19.
- Hörmann R (2005). Schilddrüsenkrankheiten Leitfaden für Praxis und Klinik (4., aktualisierte und erw. Aufl ed.). Berlin. pp. 15–37. ISBN 3-936072-27-2.
- Porth CM, Gaspard KJ, Noble KA (2011). Essentials of pathophysiology: Concepts of altered health states (3rd ed.). Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins.
- "Goitre as a determinant of the prevalence and severity of iodine deficiency disorders in populations". World Health Organization. 2014.
{{cite web}}: CS1 maint: url-status (link) - Mitchell RS, Kumar V, Abbas AK, Fausto N (2007). Robbins Basic Pathology (8th ed.). Philadelphia: Saunders. ISBN 978-1-4160-2973-1.
- "Toxicological Profile For Cyanide" (PDF). Atsdr.cdc.gov. Retrieved 2017-03-16.
- Babademez MA, Tuncay KS, Zaim M, Acar B, Karaşen RM (November 2010). "Hashimoto thyroiditis and thyroid gland anomalies". The Journal of Craniofacial Surgery. 21 (6): 1807–9. doi:10.1097/SCS.0b013e3181f43e32. PMID 21119426.
- Thyrotropin (TSH)-secreting pituitary adenomas. By Roy E Weiss and Samuel Refetoff. Last literature review version 19.1: January 2011. This topic last updated: July 2, 2009
- Abraham-Nordling M, Törring O, Hamberger B, Lundell G, Tallstedt L, Calissendorff J, Wallin G (November 2005). "Graves' disease: a long-term quality-of-life follow up of patients randomized to treatment with antithyroid drugs, radioiodine, or surgery". Thyroid. 15 (11): 1279–86. doi:10.1089/thy.2005.15.1279. PMID 16356093.
- Numbers from EUROCARE, from Page 10 in: Grünwald F, Biersack HJ (2005). Thyroid cancer. Berlin: Springer. ISBN 978-3-540-22309-2.
- Bukvic BR, Zivaljevic VR, Sipetic SB, Diklic AD, Tausanovic KM, Paunovic IR (August 2014). "Improvement of quality of life in patients with benign goiter after surgical treatment". Langenbeck's Archives of Surgery. 399 (6): 755–64. doi:10.1007/s00423-014-1221-7. PMID 25002182. S2CID 34137703.
- "Goitre". nhs.uk. 19 October 2017. Retrieved 27 March 2019.
- "Nodular Goiter - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2022-03-06.
- Frilling A, Liu C, Weber F (2004). "Benign multinodular goiter". Scandinavian Journal of Surgery. 93 (4): 278–81. doi:10.1177/145749690409300405. PMID 15658668. S2CID 38834260.
- "Toxic multinodular goitre - Symptoms, diagnosis and treatment | BMJ Best Practice". bestpractice.bmj.com.
- Gandolfi PP, Frisina A, Raffa M, Renda F, Rocchetti O, Ruggeri C, Tombolini A (August 2004). "The incidence of thyroid carcinoma in multinodular goiter: retrospective analysis". Acta Bio-Medica. 75 (2): 114–7. PMID 15481700.
- "Goiter – Simple". The New York Times.
- "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- 1
- Temple R (1986). The Genius of China: 3,000 Years of Science, Discovery, and Invention. New York: Simon and Schuster, Inc. pp. 134–5. ISBN 0-671-62028-2.
- Basedow's syndrome or disease at Who Named It? – the history and naming of the disease
- Ljunggren JG (August 1983). "[Who was the man behind the syndrome: Ismail al-Jurjani, Testa, Flagani, Parry, Graves or Basedow? Use the term hyperthyreosis instead]". Läkartidningen. 80 (32–33): 2902. PMID 6355710.
- Giuseppe Flajani at Who Named It?
- Hull G (June 1998). "Caleb Hillier Parry 1755-1822: a notable provincial physician". Journal of the Royal Society of Medicine. 91 (6): 335–8. doi:10.1177/014107689809100618. PMC 1296785. PMID 9771526.
- "Paracelsus" Britannica
- Davy, Humphry (1814-01-01). "VI. Some experiments and observations on a new substance which becomes a violet coloured gas by heat". Philosophical Transactions of the Royal Society of London. 104: 74–93. doi:10.1098/rstl.1814.0007. S2CID 109845199.
- "Iodine Deficiency".
- Hollingsworth, Dorothy R. (1977). "Kentucky Appalachian Goiter Without Iodine Deficiency". American Journal of Diseases of Children. 131 (8): 866–869. doi:10.1001/archpedi.1977.02120210044010. PMID 888801.
- "In Raising the World's I.Q., the Secret's in the Salt", article by Donald G. McNeil, Jr., December 16, 2006, The New York Times
- Wissen, Planet (16 March 2017). "Planet Wissen".
- "ARCHIVED – Why take iodine?". Nrc-cnrc.gc.ca. 2011-09-30. Retrieved 2012-11-01.
- Lahita RG, Yalof I (2004-07-20). Women and Autoimmune Disease. HarperCollins. p. 158. ISBN 978-0-06-008149-2.
- Altman LK (14 September 1991). "A White House Puzzle: Immunity Ailments". The New York Times.
Doctors Say Bush Is in Good Health
- Altman LK (28 May 1991). "The Doctor's World; A White House Puzzle: Immunity Ailments". The New York Times.
- Fox-Davies AC (1904). The Art of Heraldry: An Encyclopædia of Armory. New York and London: Benjamin Blom, Inc. p. 413.