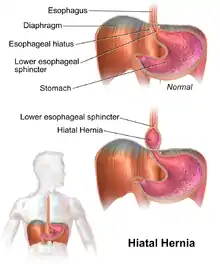
Hiatal hernia
A hiatal hernia or hiatus hernia[2] is a type of hernia in which abdominal organs (typically the stomach) slip through the diaphragm into the middle compartment of the chest.[1][3] This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn.[1][3] Other symptoms may include trouble swallowing and chest pains.[1] Complications may include iron deficiency anemia, volvulus, or bowel obstruction.[1]
| Hiatal hernia | |
|---|---|
| Other names | Hiatus hernia |
 | |
| A drawing of a hiatal hernia | |
| Specialty | Gastroenterology, general surgery |
| Symptoms | Taste of acid in the back of the mouth, heartburn, trouble swallowing[1] |
| Complications | Iron deficiency anemia, volvulus, bowel obstruction[1] |
| Types | Sliding, paraesophageal[1] |
| Risk factors | Obesity, older age, major trauma[1] |
| Diagnostic method | Endoscopy, medical imaging, manometry[1] |
| Treatment | Raising the head of the bed, weight loss, medications, surgery[1] |
| Medication | H2 blockers, proton pump inhibitors[1] |
| Frequency | 10–80% (US)[1] |
The most common risk factors are obesity and older age.[1] Other risk factors include major trauma, scoliosis, and certain types of surgery.[1] There are two main types: sliding hernia, in which the body of the stomach moves up; and paraesophageal hernia, in which an abdominal organ moves beside the esophagus.[1] The diagnosis may be confirmed with endoscopy or medical imaging.[1] Endoscopy is typically only required when concerning symptoms are present, symptoms are resistant to treatment, or the person is over 50 years of age.[1]
Symptoms from a hiatal hernia may be improved by changes such as raising the head of the bed, weight loss, and adjusting eating habits.[1] Medications that reduce gastric acid such as H2 blockers or proton pump inhibitors may also help with the symptoms.[1] If the condition does not improve with medications, a surgery to carry out a laparoscopic fundoplication may be an option.[1] Between 10% and 80% of people in the United States are affected.[1]
Signs and symptoms
Hiatal hernia has often been called the "great mimic" because its symptoms can resemble many disorders. Among them, a person with a hiatal hernia can experience dull pains in the chest, shortness of breath (caused by the hernia's effect on the diaphragm), heart palpitations (due to irritation of the vagus nerve), and swallowed food "balling up" and causing discomfort in the lower esophagus until it passes on to the stomach. In addition, hiatal hernias often result in heartburn but may also cause chest pain or pain with eating.[1]
In most cases, however, a hiatal hernia does not cause any symptoms. The pain and discomfort that a patient experiences is due to the reflux of gastric acid, air, or bile. While there are several causes of acid reflux, it occurs more frequently in the presence of hiatal hernia.
In newborns, the presence of Bochdalek hernia can be recognised[4] from symptoms such as difficulty breathing,[5] fast respiration, and increased heart rate.[6]
Causes
The following are potential causes of a hiatal hernia.[7]
- Increased pressure within the abdomen caused by:
- Heavy lifting or bending over
- Frequent or hard coughing
- Hard sneezing
- Violent vomiting
- Straining during defecation (i.e., the Valsalva maneuver)
Obesity and age-related changes to the diaphragm are also general risk factors.
Diagnosis
The diagnosis of a hiatal hernia is typically made through an upper GI series, endoscopy, high resolution manometry, esophageal pH monitoring, and computed tomography (CT). Barium swallow as in upper GI series allows the size, location, stricture, stenosis of oesophagus to be seen. Besides, it can also evaluate the oesophageal movements. Endoscopy can analyse the esophageal internal surface for erosions, ulcers, and tumours. Meanwhile, manometry can determine the integrity of esophageal movements, and the presence of esophageal achalasia. pH testings allows the quantitative analysis of acid reflux episodes. CT scan is useful in diagnosing complications of hiatal hernia such as gastric volvulus, perforation, pneumoperitoneum, and pneumomediastinum.[8]
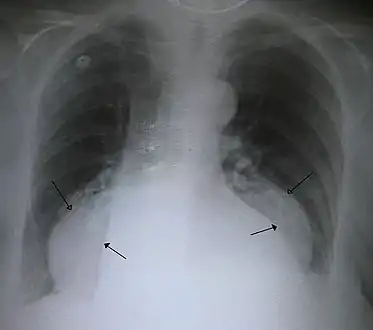 A large hiatal hernia on chest X-ray marked by open arrows in contrast to the heart borders marked by closed arrows
A large hiatal hernia on chest X-ray marked by open arrows in contrast to the heart borders marked by closed arrows This hiatal hernia is mainly identified by an air-fluid level (labeled with arrows).
This hiatal hernia is mainly identified by an air-fluid level (labeled with arrows).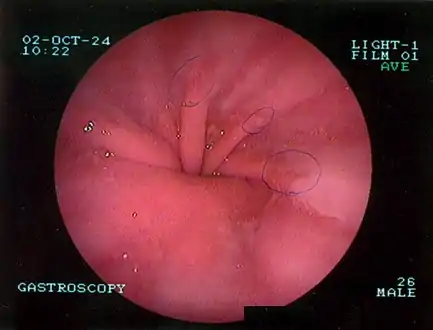 Upper GI endoscopy depicting hiatal hernia
Upper GI endoscopy depicting hiatal hernia Upper GI endoscopy in retroflexion showing Type I hiatal hernia
Upper GI endoscopy in retroflexion showing Type I hiatal hernia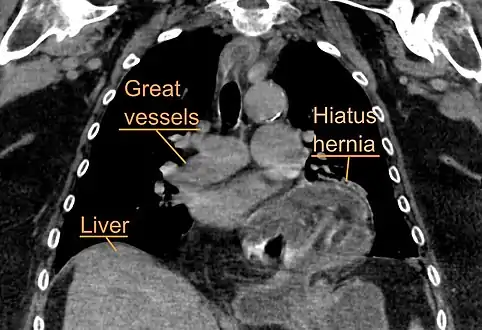 A hiatal hernia as seen on CT
A hiatal hernia as seen on CT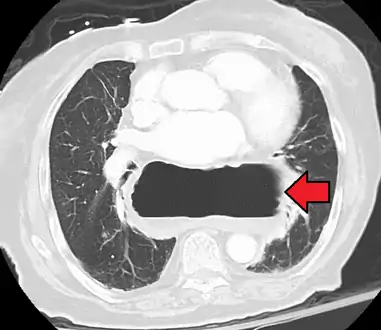 A large hiatal hernia as seen on CT imaging
A large hiatal hernia as seen on CT imaging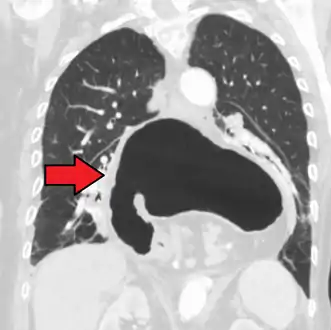 A large hiatal hernia as seen on CT imaging
A large hiatal hernia as seen on CT imaging
Classification
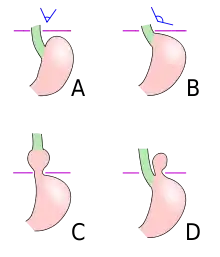
Four types of esophageal hiatal hernia are identified:[10]
Type I: A type I hernia, also known as a sliding hiatal hernia, occurs when part of the stomach slides up through the hiatal opening in the diaphragm.[11] There is a widening of the muscular hiatal tunnel and circumferential laxity of the phrenoesophageal ligament, allowing a portion of the gastric cardia to herniate upward into the posterior mediastinum. The clinical significance of type I hernias is in their association with reflux disease. Sliding hernias are the most common type and account for 95% of all hiatal hernias.[12] (C)
Type II: A type II hernia, also known as a paraesophageal or rolling hernia, occurs when the fundus and greater curvature of the stomach roll up through the diaphragm, forming a pocket alongside the esophagus.[11] It results from a localized defect in the phrenoesophageal ligament while the gastroesophageal junction remains fixed to the pre aortic fascia and the median arcuate ligament. The gastric fundus then serves as the leading point of herniation. Although type II hernias are associated with reflux disease, their primary clinical significance lies in the potential for mechanical complications. (D)
Type III: Type III hernias have elements of both types I and II hernias. With progressive enlargement of the hernia through the hiatus, the phrenoesophageal ligament stretches, displacing the gastroesophageal junction above the diaphragm, thereby adding a sliding element to the type II hernia.
Type IV: Type IV hiatus hernia is associated with a large defect in the phrenoesophageal ligament, allowing other organs, such as colon, spleen, pancreas and small intestine to enter the hernia sac.
The end stage of type I and type II hernias occurs when the whole stomach migrates up into the chest by rotating 180° around its longitudinal axis, with the cardia and pylorus as fixed points. In this situation the abnormality is usually referred to as an intrathoracic stomach.
Treatment
In the great majority of cases, people experience no significant discomfort, and no treatment is required. People with symptoms should elevate the head of their beds and avoid lying down directly after meals.[1] If the condition has been brought on by stress, stress reduction techniques may be prescribed, or if overweight, weight loss may be indicated.
Medications
Antisecretory drugs such as proton pump inhibitors and H2 receptor blockers can be used to reduce acid secretion. Medications that reduce the lower esophageal sphincter (LES) pressure should be avoided.
Procedures
There is tentative evidence from non-controlled trials that oral neuromuscular training may improve symptoms.[13] This has been approved by the UK National Health Service for supply on prescription from 1 May 2022.[14]
Surgery
In some unusual instances, as when the hiatal hernia is unusually large, or is of the paraesophageal type, it may cause esophageal stricture or severe discomfort. About 5% of hiatal hernias are paraesophageal. If symptoms from such a hernia are severe for example if chronic acid reflux threatens to severely injure the esophagus or is causing Barrett's esophagus, surgery is sometimes recommended. However surgery has its own risks including death and disability, so that even for large or paraesophageal hernias, watchful waiting may on balance be safer and cause fewer problems than surgery.[15] Complications from surgical procedures to correct a hiatal hernia may include gas bloat syndrome, dysphagia (trouble swallowing), dumping syndrome, excessive scarring, and rarely, achalasia.[15][16] Surgical procedures sometimes fail over time, requiring a second surgery to make repairs.
One surgical procedure used is called Nissen fundoplication. In fundoplication, the gastric fundus (upper part) of the stomach is wrapped, or plicated, around the inferior part of the esophagus, preventing herniation of the stomach through the hiatus in the diaphragm and the reflux of gastric acid. The procedure is now commonly performed laparoscopically. With proper patient selection, laparoscopic fundoplication studies in the 21st century have indicated relatively low complication rates, quick recovery, and relatively good long term results.[17][18][19][20] Regarding the discussion of partial versus complete fundoplication procedures, significant variations in the postoperative outcome emphasize the increased prevalence of dysphagia after Nissen. The statistics given support the superiority of laparoscopic over traditional surgery, owing to the greater aesthetic result, shorter admission time – with lower costs – and faster social reintegration.[21]
Epidemiology
Incidence of hiatal hernias increases with age; approximately 60% of individuals aged 50 or older have a hiatal hernia.[22] Of these, 9% are symptomatic, depending on the competence of the lower esophageal sphincter (LES). 95% of these are "sliding" hiatal hernias, in which the LES protrudes above the diaphragm along with the stomach, and only 5% are the "rolling" type (paraesophageal), in which the LES remains stationary, but the stomach protrudes above the diaphragm.
Hiatal hernias are most common in North America and Western Europe and rare in rural African communities.[23] Some have proposed that insufficient dietary fiber and the use of a high sitting position for defecation may increase the risk.[24]
References
- Roman, S; Kahrilas, PJ (23 October 2014). "The diagnosis and management of hiatus hernia". BMJ (Clinical Research Ed.). 349: g6154. doi:10.1136/bmj.g6154. PMID 25341679. S2CID 7141090.
However, the exact prevalence of hiatus hernia is difficult to determine because of the inherent subjectivity in diagnostic criteria. Consequently, estimates vary widely—for example, from 10% to 80% of the adult population in North America
- "Hiatus hernia - Illnesses & conditions". NHS inform. Retrieved 10 May 2022.
- "Hiatal Hernia". PubMed Health. Archived from the original on 28 April 2017.
- Chang SW, Lee HC, Yeung CY, Chan WT, Hsu CH, Kao HA, Hung HY, Chang JH, Sheu JC, Wang NL (2010). "A twenty-year review of early and late-presenting congenital Bochdalek diaphragmatic hernia: are they different clinical spectra?". Pediatr Neonatol. 51 (1): 26–30. doi:10.1016/S1875-9572(10)60006-X. PMID 20225535.
- Ganeshan DM, Correa AM, Bhosale P, Vaporciyan AA, Rice D, Mehran RJ, Walsh GL, Iyer R, Roth JA, Swisher SG, Hofstetter WL (2013). "Diaphragmatic hernia after esophagectomy in 440 patients with long-term follow-up". Ann Thorac Surg. 96 (4): 1138–45. doi:10.1016/j.athoracsur.2013.04.076. PMID 23810174.
- Alam, A; Chander, B.N. (July 2005). "Adult bochdalek hernia". MJAFI. 61 (3): 284–6. doi:10.1016/S0377-1237(05)80177-7. PMC 4925637. PMID 27407781.
- "Hiatal hernia - Symptoms and causes". Mayo Clinic.
- Sfara, Alice; Dumitrașcu, Dan L (12 September 2019). "The management of hiatal hernia: an update on diagnosis and treatment". Medicine and Pharmacy Reports. 92 (4): 321–325. doi:10.15386/mpr-1323. ISSN 2668-0572. PMC 6853045. PMID 31750430.
- "UOTW #39 - Ultrasound of the Week". Ultrasound of the Week. 25 February 2015. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- Kahrilas, Peter J.; Kim, Hyon C.; Pandolfino, John E. (2008). "Approaches to the diagnosis and grading of hiatal hernia". Best Practice & Research Clinical Gastroenterology. 22 (4): 601–616. doi:10.1016/j.bpg.2007.12.007. PMC 2548324. PMID 18656819.
- Lewis, Sharon Mantik (2017). Medical-surgical nursing : assessment and management of clinical problems. Bucher, Linda,, Heitkemper, Margaret M. (Margaret McLean),, Harding, Mariann (10th ed.). St. Louis, Missouri. ISBN 978-0-323-32852-4. OCLC 944472408.
- Dennis Kasper; Anthony Fauci; Stephen Hauser; Dan Longo; J. Larry Jameson; Joseph Loscalzo (8 April 2015). Harrison's Principles of Internal Medicine, 19e (19 ed.). McGraw-Hill Global Education. p. 1902. ISBN 978-0071802154.
- Clinical and technical evidence - IQoro for hiatus hernia (Report). National Institute for Health and Care Excellence. 6 March 2019. MIB176.
- "Innovative IQoro neuromuscular treatment device achieves NHS prescription status". Advances in Clinical Neuroscience and Rehabilitation (ACNR). 25 March 2022.
- Stylopoulos N, Gazelle GS, Rattner DW (2002). "Paraesophageal hernias: operation or observation?". Ann Surg. 236 (4): 492–500. doi:10.1097/00000658-200210000-00012. PMC 1422604. PMID 12368678.
- Laparoscopic Nissen fundoplication - Information for patients (PDF) (Report). Oxford University Hospitals NHS. December 2021. OMI68160.
- Migaczewski M, Pędziwiatr M, Matłok M, Budzyński A (2013). "Laparoscopic Nissen fundoplication in the treatment of Barrett's esophagus — 10 years of experience". Wideochir Inne Tech Maloinwazyjne. 8 (2): 139–45. doi:10.5114/wiitm.2011.32941. PMC 3699774. PMID 23837098.
- Witteman BP, Strijkers R, de Vries E, Toemen L, Conchillo JM, Hameeteman W, Dagnelie PC, Koek GH, Bouvy ND (2012). "Transoral incisionless fundoplication for treatment of gastroesophageal reflux disease in clinical practice". Surg Endosc. 26 (11): 3307–15. doi:10.1007/s00464-012-2324-2. PMC 3472060. PMID 22648098.
- Ozmen V, Oran ES, Gorgun E, Asoglu O, Igci A, Kecer M, Dizdaroglu F (2006). "Histologic and clinical outcome after laparoscopic Nissen fundoplication for gastroesophageal reflux disease and Barrett's esophagus". Surg Endosc. 20 (2): 226–9. doi:10.1007/s00464-005-0434-9. PMID 16362470. S2CID 25195984.
- Abbas AE, Deschamps C, Cassivi SD, Allen MS, Nichols FC, Miller DL, Pairolero PC (2004). "Barrett's esophagus: the role of laparoscopic fundoplication". Ann. Thorac. Surg. 77 (2): 393–6. doi:10.1016/S0003-4975(03)01352-3. PMID 14759403.
- Lucenco, L.; Marincas, M.; Cirimbei, C.; Bratucu, E.; Ionescu, S. (2012). "The 10 years' experience in the laparoscopic treatment of benign pathology of the eso gastric junction". Journal of Medicine and Life. 5 (2): 179–184. PMC 3391883. PMID 22802887.
- Goyal Raj K, "Chapter 286. Diseases of the Esophagus". Harrison's Principles of Internal Medicine, 17e.
- Burkitt DP (1981). "Hiatus hernia: is it preventable?". Am. J. Clin. Nutr. 34 (3): 428–31. doi:10.1093/ajcn/34.3.428. PMID 6259926.
- Sontag S (1999). "Defining GERD". Yale J Biol Med. 72 (2–3): 69–80. PMC 2579007. PMID 10780568.